i have more delays...is it bad or i am overreacting
Dear all, I had biopsy on right breast and result :DCIS as of now
After that i had an appointment with my surgeon and he ordered 2 more biopsies of calcification: the same breast and also left breast.
Today i called to find out if i can have biopsies sooner than 11/25. Instead:
found out about more delays today... please let me know if this is not a big deal...
i am not talking about emotional state, this is bad for that...but i am scared of delays in terms of what will be developing in my breasts.
So my 2 biopsies will be on 11/25. And results will be after that ...i don't know ...in 3-5 days(this is usually how it is, i did not ask now).
BUT doctor will be away, and the earliest appt. i will have with him: dec 13.
And, no, i can not be seen by another doctor...or i should start "transition" ...and i will not be able to get back to this surgeon...and also i don't know at this point if doctors(i got a few names from my friends) do have appt. available much earlier than dec.13
First i was hysterical...I don't know yet what they will find with those 2 biopsies ...and when my surgery will happen if my appt. with the doctor only on dec 13.
I am trying to calm myself down...
what do you think about this situation ? is it really bad delay? thank you
Comments
-
It's not that much of a delay, and the vast majority of cancers don't grow or spread in a short period of time. Breathe and try to focus on other things until the appointment.
0 -
Here is a copy of the answer I just provided in your same question in your other discussion thread:
The delay is not bad medically.
Your diagnosis is DCIS, and the additional areas of concern are both sites with calcifications, which, if cancer, usually (but admittedly not always) means DCIS. DCIS is a pre-invasive condition. While removing DCIS cells before they develop into invasive cancer (which might never happen or might take years) is almost always recommended (although there are some "watchful waiting" trials underway with DCIS), DCIS is not a medical emergency. With DCIS there is no urgent need to get into surgery.
Mentally, the extra waiting time is brutal. Since you already have a DCIS diagnosis and the only question about surgery is how extensive the surgery will be, can you request that the surgeon's office schedule you for surgery, and then the type of surgery will be determined based on these biopsies? And if you are considering a mastectomy or bilateral mastectomy if the biopsy results are positive, and if with a MX or BMX you are considering reconstruction, can you get in to see a Plastic Surgeon while you are waiting for the biopsy and results? I think there are ways you can use this time to get things done that cut down on the waiting time after your biopsy results are in.
0 -
thank you. I was not sure if i have to start a new topic...or continue in previous one.
what is the best way to do it in the future? because things are happening...and developing...and i don't know who to talk to but you, guys.
thank you Beesie!
0 -
If the new information is related to what you've said in a previous thread, it's best to maintain a single discussion thread. This way new people responding will get the whole story and will have the benefit of seeing the previous responses. And often people who post a response go back to check for updates, and if you've started a new thread, they might miss it.
If your question is about something completely different and the previous discussion doesn't factor in or add to the story, or if it is more appropriate in a forum specifically about this new topic (questions about Radiation, for example), then a new thread might be appropriate.
0 -
Just chiming in to agree with Alice and Beesie. We are all thinking good thoughts for you.
0 -
thank you, Beesie and Georgia1.
it is kind off this topic: but how you decide if it is mastectomy -to have reconstruction or not.
thank you
0 -
Marinochka - I agree with Beesie & Alice. If you stay on one thread, those of us who have been following you can continue. When you start a new thread, we don't remember your details. Particularly since you don't yet have specs to post in your tag line. There are lots of existing threads that discuss reconstruction. Check in "all threads" and you'll find many posts.
0 -
good morning, i was able to move my appt. 2 days ahead, 12/11.
Not much difference, i know, but it is what it is.
I want to ask (i read here and it makes me thinking), if i will have all results at this point of all 3 biopsies, and i will be talking to a doctor which surgery is planned...but as i understand some other things which are not clear after biopsy yet (like HER2, for example)...they should affect decision of what type of surgery(lumpectomy or mastectomy)...how it works at this point.
Does it make sense what i am asking? How we can make a plan for surgery on 12/11 if we don't have HER2 yet or oncotype?
And when it is decided to have a lymph node removal/biopsy...it is always done during surgery.
I want to understand how to get ready for this appointment and what to ask there. thank you
0 -
Let's see if I can answer your questions.
First, checking the nodes. If your diagnosis from all your biopsies is DCIS, and if you are having a lumpectomy, then there is no reason to have a sentinel node biopsy. Nodes do not need to be checked when the diagnosis is DCIS. This is a good thing, because removal of lymph nodes presents a lifelong risk of lymphedema.
However if you are having a mastectomy, normally even with a DCIS diagnosis, an SNB will be done. This is because in about 20% of cases where the needle biopsy diagnosis is DCIS, some invasive cancer is found during the surgery, changing the diagnosis from Stage 0 DCIS to Stage I (or higher) IDC. Once invasive cancer has been found, the nodes do need to be checked. The SNB procedure involves making an injection (or blue dye and/or isotopes) into the breast. After a lumpectomy for DCIS, if invasive cancer is found in the final pathology, an SNB can be done afterwards as a quick second surgery. But after a mastectomy, there is no longer a breast so it becomes much more difficult to do an SNB. This is why with a DCIS diagnosis, normally an SNB isn't done with a lumpectomy but is done with a MX.
Should one of the biopsies show invasive cancer, then an SNB will be done whichever type of surgery you have.
As for details from the pathology changing the type of surgery recommended, that's not the case. First of all, if you have pure Stage 0 DCIS, HER2 testing probably won't be done and you will not need the Oncotype test (unless you have a lumpectomy and are considering skipping radiation, which means a different Oncotype test, the Oncotype DCIS).
If you have invasive cancer, the significance of HER2 status and the Oncotype result is that they provide indications as to the aggressiveness of the cancer. The more aggressive the cancer, the greater the risk that some cancer cells might have moved beyond the breast prior to the surgery/removal of the cancer from the breast. With any invasive breast cancer, there is always the possibility that some rogue cells might have escaped and moved into the body setting up the risk of a future metastatic recurrence. It is the degree of risk that determines the treatment plan and whether chemo and other systemic treatments are recommended. With HER2+ invasive cancer, because it is so aggressive, even for a very small cancer, chemo and Herceptin will be recommended. Together, these treatments are extremely effective and bring the risk back down to what it would be (or even lower) for an HER2- cancer. Similarly, for ER+ cancers, with a higher Oncotype DX score (the invasive cancer Oncotype test), chemo will be recommended. WIth a lower score, usually only endocrine therapy (a daily pill or 5 or 10 year, either Tamoxifen or an Aromatase Inhibitor) will be recommended.
To net it out, for invasive breast cancer, the pathology of the cancer and tests such as the Oncotype test determine the treatment plan beyond surgery. These results don't make a difference to the surgery plan. Whether the patient has a lumpectomy or a mastectomy has no impact on the chemo or Herceptin recommendation because these are systemic (whole body) treatments given to address the risk of a distant (in the body) recurrence, i.e. metastatic cancer. For local recurrence, the treatments are radiation, which is pretty much always recommended after a lumpectomy (and usually is not required after a MX but may sometimes be recommended) and endocrine therapy for ER+ cancers. Because endocrine therapy addresses both local and distant recurrence risk, endocrine therapy will be recommended regardless of whether the patient has a lumpectomy or MX and will be prescribed even after chemo for those who are ER+.
Hope that makes sense. And since your preliminary diagnosis is DCIS, this thread might help:
Topic: A layperson's guide to DCIS
0 -
Thank you very much Beesie for such a detailed explanation. it is very important for me.
0 -
I was diagnosed with IDC and DCIS at the end of February. I met with both the MO and BS less than a week later. The biopsy had showed a small mass, which turned out to be 1.5cm. The hitch in scheduling was MINE -- I was flying across the country on March 23 to spend 3 weeks with family, a long-planned and important trip. Surgery couldn't be scheduled reasonably before the trip, so it happened as soon as I got back in mid-April. While that might not have been the ideal, it was fine. Neither the surgeon nor the MO had any issues with it. It didn't change my treatment plan a bit, only the timing. It didn't put me at risk.
0 -
thank you MountainMia for sharing your situation. Wish you health!
0 -
I had 2 biopsies today....it was not bad at all, but i was not worried about the procedures, i am worried about the result.
praying now....
0 -
I am not sure i should ask this question here or somewhere else.
I have not identified autoimmune disease ...i have for 15 years, and i was lucky, i don't take any medication and the only symptom i have: photo sensitivity to UVA and UVB. I wear long sleeves during summer, don't go to the beach, wear hats and use sunscreen for my face, because you can not hide your face from sun.
I am used to that condition and it does not interfere with my life.
But i am worried now if i will be able to have radiation because of that condition. I did not discuss it with doctors...because i am still waiting for discussing my future treatment plan...but of course i am wondering about it.
My understanding that radiation is different than UVA/UVB....and i don't feel any effect on my skin of x- ray or mammogram.
I know how important radiation treatment is ...and i hope i still can have it.
thank you
0 -
i got result that those 2 other places i had biopsies are benign.
Of course i am very happy about that.
now want to get ready to surgeon appt. and make sure i have all questions to ask.
please let me know any thoughts of what else i should discuss with the doctor.
thank you!!!!
0 -
That's great news about the biopsies!
Given your questions/concerns about radiation, although usually patients don't see the Radiation Oncologist until after surgery, you should probably request a consult appointment prior to surgery. I have no idea if your photo sensitivity will be an issue for rads, but if it is, you need to know this before you make the decision about what type of surgery to have.
And given this concern, a question for the surgeon is whether he thinks there is any possibility that you can get away with a lumpectomy without rads. If the area of DCIS is relatively small and confined, and if the DCIS is not overly aggressive, then it's possible that a lumpectomy with wide margins (at least 1cm), followed by Tamoxifen or an AI (if your DCIS is ER+), will be sufficient to deliver a low recurrence risk. This would be a bit risky, since the surgery could turn up something unexpected (some invasive cancer, or more DCIS than expected, compromising the size of the margins) but it may be worth discussing with your surgeon, just so that you can make your surgery decision knowing all your options.
0 -
Hi, Beesie
thank you for your kind words and advice what and how to discuss with the surgeon.
I also found a woman with similar situation on lupus forum, who had rads...and she has also extreme photo sensitivity.
she told me that it was ok, she was not badly effected by rads...she was more effected there, in the room, but red light beams on the ceiling, so she was covering her face from those lights. otherwise she was ok. it gives me encourangment and hope.
0 -
I just want to chime in about SNB (sentinel lymph node) biopsy for DCIS. It is a standard of care to do it for DCIS. I had 3 nodes removed on my DCIS side. Reason being - biopsy is just that - a small piece of tumor, not the entire tumor, and they can't say with 100% certainty until the entire tumor is removed that it doesn't have an invasive component. Therefore, they do check lymph nodes with DCIS.
0 -
FarAwayToo, you had a mastectomy, not a lumpectomy, correct? That's an important distinction when it comes to whether or not an SNB is indicated after a biopsy finds DCIS. It also appears from your signature line that you had invasive cancer in your right breast at the same time that DCIS was diagnosed in your left breast. That is a unique situation that would likely warrant a greater concern that invasive cancer might also be present on the left side. So your situation was quite different from where marinochka is right now.
An SNB is NOT the standard of care for those having a lumpectomy for DCIS. Removing lymph nodes, even just 1-3 nodes through a sentinel node biopsy, results in a life long risk of lymphedema. So it's preferable to not remove nodes unless necessary. This is why DCIS treatment guidelines do not recommend an SNB for anyone having a lumpectomy. However an SNB is usually done for those who have a biopsy finding of DCIS and are having a mastectomy. I explained the reason for this in my earlier post in this thread:
......
First, checking the nodes. If your diagnosis from all your biopsies is DCIS, and if you are having a lumpectomy, then there is no reason to have a sentinel node biopsy. Nodes do not need to be checked when the diagnosis is DCIS. This is a good thing, because removal of lymph nodes presents a lifelong risk of lymphedema.
However if you are having a mastectomy, normally even with a DCIS diagnosis, an SNB will be done. This is because in about 20% of cases where the needle biopsy diagnosis is DCIS, some invasive cancer is found during the surgery, changing the diagnosis from Stage 0 DCIS to Stage I (or higher) IDC. Once invasive cancer has been found, the nodes do need to be checked. The SNB procedure involves making an injection (or blue dye and/or isotopes) into the breast. After a lumpectomy for DCIS, if invasive cancer is found in the final pathology, an SNB can be done afterwards as a quick second surgery. But after a mastectomy, there is no longer a breast so it becomes much more difficult to do an SNB. This is why with a DCIS diagnosis, normally an SNB isn't done with a lumpectomy but is done with a MX.
......
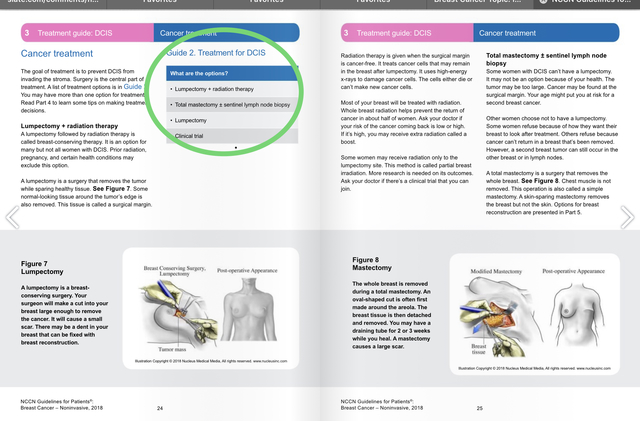
Here are the NCCN treatment guidelines for DCIS. A "lumpectomy + sentinel lymph node biopsy" is not included as a surgical option: https://www.nccn.org/patients/guidelines/stage_0_breast/26/
 0
0 -
thank you FarAwayToo for information.
I would ask then: when they check SNB in this case -during surgery?
thank you
0 -
I apologize, I misunderstood the surgery plan. Yes for SNB for mastectomy, no for lumpectomy.
0 -
thank you Beesie
thank you FarAwayToo
Now it is more clear.
0 -
i will have a lumpectomy on 12/19.
Beesie, thank you for all your knowledge and help, i was able to have a good discussion with a surgeon with questions and answers.
I also did not hear from him anything what i did not know already, felt prepared.
Of course now is important to see what after surgery pathology report would show: hopefully not something worse than DCIS.
But is something to wait and find out.
0 -
Glad I was able to help.
Good luck on the 19th. Hoping for a final diagnosis that is Stage 0 DCIS!
0 -
thank you Beesie. will report how it will go.
0 -
I had localisation procedure today, it was easy...and fast.
Tomorrow i have to be at the hospital at 7a.m. ...for surgery.
0 -
Good luck with your surgery!
0 -
thank you MikaMika
I had lumpectomy today. I feel ok, not much pain. I can take a shower in 24 hours after surgery.
Now will be waiting for a pathology report and pray that it would show the same not worse what biopsy showed.
I was told that i can walk starting tomorrow(outside) and it is even good for me. But no other excersises till i see a doctor which is jan 6.
Also that margins would be ok...and it does not need additional surgery(but this is not so scary, i am prepared mentally that it might happen).
0 -
would you please let me know when usually radiation treatment starts after the day of surgery.
is it after 3-4 weeks?
thank you
0 -
I had another round of chemo infusions after surgery so my radiation didn't start for several months. Sorry I don't know what it will be for you.
Do go to My Profile and put in your diagnosis and treatment details. It will make it much easier for people to answer.
0