Dense Breasts and History of Breast Cancer
I have dense breasts - Category C - Heterogeneously Dense - and was diagnosed with breast cancer in my right breast 7/29/21.
I had a lumpectomy and just finished 16 rounds of radiation. My tumor was small (3mm) and luckily no lymph node involvement, so no chemo. Because of the tumor size I also was unable to get Oncotype, so my recurrence numbers are a little murky, but they range between 3-5%, 5% being what my oncologist determined. I will see my MO in late Dec to start hormone blockers as my tumor was ER/PR+.
A huge part of this journey has been education. I recently learned that having "dense breasts" - either category C or D puts one in a higher than normal risk category. As does having had breast cancer already. I pulled my last mammo letter and it notes that I have heterogeneously dense breasts, and may be at high risk for breast cancer, and that dense breast tissue makes it harder to evaluate the results of a mammogram and may be assoc with a higher risk of breast cancer. It states that I should talk to my doctor about having additional screenings - US or MRI.
Never once has anyone told me any of this or talked to me about additional screenings. So I've done research on my own and found that the American College of Radiology in 2018 recommended annual surveillance MRI in women with dense breasts and with a personal history of breast cancer. That's me.
So I called my breast surgeon's office, and a message was relayed to me from the PA by an admin person that that's just a standard statement they put on mammo reports, and it only applies to women with Category D, extremely dense breasts. I am kind of floored that this is their response.
I'm guessing (maybe wrongly) that my whole breast radiation probably killed off anything in my cancerous breast, but what about the other breast? Only a 3D mammo has been done. Shouldn't they at the very least do an Ultrasound, or now, given the recommendations by the American College do an MRI? The breast surgeon's office told me that since I had a 3D mammo, that is sufficient.
I don't know what to do here. There are only two doctor groups here. Each group is affiliated with one of two large hospitals. My group that my breast surgeon doesn't belong to does not take my insurance, so I would have to pay out of pocket for any consult or additional testing. I'm afraid every doctor - breast surgeons, oncologists, etc. in the group I am with will tell me the same thing.
I feel like I am being let down here. Am I wrong in thinking that I should be having imaging other than just mammos? I know the next thing they will tell me is there are too many false positives leading to unnecessary biopsies. Well that may be, but I'd rather that than go through breast cancer again, and maybe a worse stage, needing chemo, etc., or have something that has progressed to METS.
Can anyone guide me here?
Comments
-
Hi - I have dense breast tissue as well and have been called back for follow-up mammograms from time to time over the past five years or so. They've been monitoring the calcifications I received similar letters mentioning that ultrasound or MRI could be appropriate depending on individual risk factors. This year, in addition to follow-up screenings on the left breast, they added an ultrasound, which definitely caught my attention because I knew they were digging a little deeper. That visit led to the biopsy, which led to the DCIS diagnosis, which led to surgery earlier this week. Prior to surgery, I had an MRI on both breasts, which showed nothing unusual in the right breast. I don't know what the screening process will look like after radiation, because I'm a little behind you in the process. As far as what happened in the past, my sense is that they were watching it, caught it at just the right time and doing anything earlier would have been overtreatment. Maybe that's naiveté, and I may come to second guess that assessment in the future, but that's where I stand at this point.
0 -
Breast density is really poorly explained by doctors and even by most websites about breast density.
Category C density is actually quite normal for your age. And as you can see from this graph, breast density tends to decline with age. Of greatest concern are those who continue to have Category D density post-menopausally. This is why MRIs are only routinely done on those with the highest level of density - otherwise, MRIs would be necessary for 50% of all women.
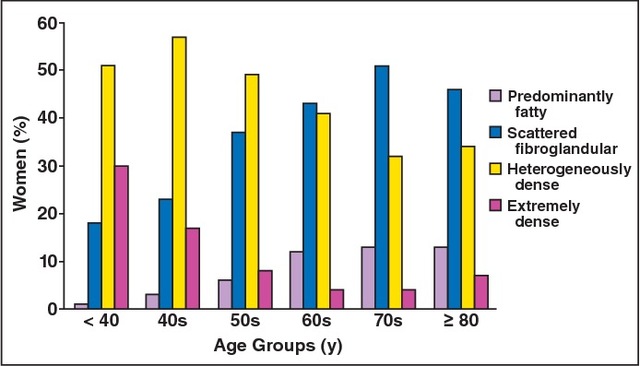
The other thing to understand is that when you see risk figures related to breast density, usually the increase in risk quoted is a comparison between those with the lowest density vs. those with the highest density. The two middle categories are more normal and are pretty much baked into the "average" risk figures. Therefore while risk may be somewhat increased for those with heterogeneously dense breasts, the increase against average risk would not be that great.
Having said that, with your history of breast cancer and your Cat. C breast density, a reasonable request would be to supplement your mammogram with an ultrasound. That is usually the approach taken when MRIs are not available.
0 -
Hi Macdebbie,
I have some ideas but I don't have enough expertise to call it guidance.
I would consider paying OOP for a second opinion from a breast center that is more prestigious than your local center and a doctor who is more senior/credentialed. If they can give you the opinion that additional screening is recommended, then I would take that back to your local center and discuss it with your doc. If your doc is still reluctant, the magic words I have read about are something like, "Can you please note it in my file that despite the recommendation for _____ screening from Dr. Abc at Medical Center XYZ, and against the recommendations from the American College of Radiology, you are declining to prescribe it for me?" and waiting to be shown that it's added to the doctors' notes, and asking for a copy. If it get that far, then I would take the recommendation and the file to my regular doctor/ob (even if they're not an oncologist) and ask them to order the screening. AFAIK, any doctor can order any test.
I don't know that that will work, but I think it has a decent shot.
FWIW, I am a survivor without dense breasts, but due to younger age and family history, my doctor agreed to let me alternate between MRIs and mammos every 6 months and my insurance is covering it. The MRI has already led to one biopsy for a benign finding - that false positive rearing its ugly head. It really was wrenching and stressful, and I second guessed my request for that extra level of screening. But neither the radiation oncologist nor my regular oncologist said a single thing to imply that I was somehow over the top or wasting money and resources.
---
Another thing you might try first is having a male come with you and speak to your doctor. It doesn't have to be a husband. A dad, brother, boyfriend, or even male friend, make a difference: https://aleteia.org/2018/06/07/why-you-should-brin...
Bleh.
---
Good luck!
0 -
Beesie - thanks for weighing in. I did read that Category C dense breasts are quite common, but it is the combination of having dense breasts and having had cancer that is weighing on my and looking at the sensitivity rates - mammogram alone - 31-33%, MRI alone 87-96%, and mammogram and ultrasound 44-48%.
The ACR recommendations are for either breast density category of C or D to include an annual MRI if the patient has a personal history of breast cancer. The American Cancer Society recommends MRI screening in "high risk" women regardless of breast density. I would assume having had breast cancer puts me in the "high risk" category?
At the very least I would like an ultrasound as supplement to my mammograms. However, I don't understand the reluctance of doctors to prescribe and MRI when it could save lives and when it is warranted. I am not just a woman with dense breasts. They always cite "cost" but why are docs so concerned with cost. They aren't paying for it, I am, or in this case my insurance is. So why do they care? I can only guess there must be some disincentive to order MRIs or some tie with the insurance companies, but I feel like they should care about me more than they care about the insurance companies.
Unfortunately my breast density has not improved. I am 64 now and my breasts are just as dense as they were in my 40s and 50s.
Salamandra - Thx for your thoughts. It's very hard for me to get a second opinion from a prestigious cancer center. Unfortunately Telehealth visits are disallowed and I don't want to be traveling with COVID. The best I could do is go to the other hospital group for a consult with another breast surgeon. That hospital is a teaching hospital and is nationally ranked in Cancer. Certainly not on the level of a Dana Farber which I would have gone to back home, or a Johns Hopkins though.
The breast surgeon I went to is considered the best in this area, probably the entire state. I felt very comfortable with her and her level of expertise but I do not agree with her here. I'd much prefer to be cautious. And if I have to go through a few false positive biopsies so be it. Better than getting cancer again.
I have heard of the "please make a note in my file" play, and if push comes to shove I will use it, but I don't want to create tension in this relationship as she is who I would want to go to if I need breast surgery ever again, God forbid.
0 -
Debbie - Have you talked to your GYN? That's who wrote my orders for an ultrasound.
Or I would suggest a consult with an oncologist. Yes, I see that maybe you didn't have any other treatment, but surgeons cut. That's what they do then most often they're through. Oncologists look at the entire panorama of cancer. I met with one before my mastectomy even though everyone was sure I wouldn't need chemo (which I didn't that time) because I wanted a 'driver of the bus' for whatever happened.
0 -
Hi macdebbie, I am sorry you are going through this. But I am glad you are asking questions. I also have dense breasts and I’ve had breast cancer in the same breast twice now and the 3D mammo didn’t catch it either time. Because of this we will be doing both 3D mammo and a MRI 6 months apart moving forward. I would hope your MO would be willing to do this for you too. So keep fighting for it!
0 -
@macdebbie - I'm sorry you are going through this. An excellent point was made above about consulting with an oncologist to review the overall picture. I'm also 64 with a similar diagnosis, strong family history and a genetic mutation. My MO has recommended alternating a mammogram and MRI every 6 months because of the genetic issue. I have declined for my own reasons but believe everyone who is high risk should be allowed an MRI if they wish.
A few weeks ago, I mentioned to my BS that the MO recommended an MRI. The BS orders the mammogram, but the MO would order the MRI. The two doctors practice in different hospital systems although the BS can do breast surgery in both systems. The BS doesn't believe an MRI would be helpful in my case but said her hospital system believes a Mammo + ultrasound is more useful. I did have both the mammo and u/s last summer because of a suspicious skin lesion on the left and skin thickening/swellingon the right - both of which were suspicious for IBC but turned out to be nothing. In the future, I don't plan to do a u/s unless there is a suspicious finding. I think it's interesting to note that there are different schools of thought between and among doctors and hospital systems. And yes, there may be some financial incentive or disincentive for which screenings are recommended over and above a mammogram.
Best of luck and keep us updated. I'll be thinking of you.
0 -
I have very dense tissues and the breast center where I do my mamos actually after the 3D mamo said I needed it and did it automatically. No doctor had to request other than the radiologist who read it said I needed it. They do read it when I am there and report before I leave because of my history. They do it with all the people who come in for testing there. It is affiliated with a local university hospital system though and that might make a difference as well. Best wishes.
0 -
I agree that you should see a gynecologist. That’s who always made the script for a diagnostic mammogram, followed by ultrasound because of dense breasts. It wouldn’t have helped me because I have lobular mets, and they’ve never found the cancer in my breasts, but that’s who asked for it for me.
0 -
macdebbie, I do understand that your concern is the combination of having a personal history of breast cancer + dense breasts. I was simply trying to provide some more information about your level of breast density, which is average for your age. With Cat 3 density, I think your higher risk comes from having been previously diagnosed - and I personally believe that alone should get you supplemental screening. I think all women previously diagnosed, who have not have had a BMX, should be considered "high risk" and receive high risk screening. Unfortunately that's not how it generally works out, however.
What is your source for this data? "looking at the sensitivity rates - mammogram alone - 31-33%, MRI alone 87-96%, and mammogram and ultrasound 44-48%."
There may be one or two studies with those results, but the studies and meta-analyses I've looked at suggest that for women with dense breasts, mammograms alone have sensitivity of ~45%-65%, versus about 80%-90% for the combination of mammograms and ultrasounds.
"The researchers found that adding ultrasound to mammography increased cancer detection by an absolute rate of 29% -- rising from 53% with mammography alone to 82% with both screenings." RSNA: Ultrasound, MRI Helpful Aids for Dense Breasts https://www.medpagetoday.com/meetingcoverage/rsna/17318
"Overall, the sensitivity of mammography for the detection of breast cancer is 85%; however, in women with dense breast tissue, the sensitivity of mammography is reduced to 47.8–64.4." The Role of Ultrasound in Screening Dense Breasts—A Review of the Literature and Practical Solutions for Implementation https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872003/
I recall seeing a study a while back that compared the efficacy of adding an MRI to a mammogram versus adding an ultrasound to a mammogram. As I recall, adding the MRI did increase the cancer detection rate, although the difference was surprisingly small and the rate of false positives was higher. I will dig around to see if I can find that study.
0 -
I agree that we should have screening appropriate for our increased risk. I don't know what "appropriate" means, and where the balance is between sensitivity and accuracy.
What I do know is that even if your doctor orders a test, your insurance might not pay for it. So even if you get that order, it might be important to you to find out whether you need to pay out of pocket or not.
0 -
Macdebbie I wish you success in pursuing proper screening given your history and density. Speaking as someone for whom mammography and ultrasound both failed to find my mass, MRI is another tool that can make the difference. In reading your post, I was unclear if you have ever had an MRI or if you have not had one post treatment. Regardless, it may make sense to add one into the rotation with some frequency.
0 -
Google "abbreviated MRI" it is a new way to screen dense breasts for a cancer. I asked my breast surgeon about it. Given that a regular mammogram missed my tumor, I will have the abbreviated MRI and a regular mammogram, alternating 6 months. Unfortunately it's not covered by my insurance, so I have to pay $500 for it. Good luck,
Julie
0 -
Thanks all. I have an appt with my GYN Monday, my RO 12/22 and my MO 12/27. I am hoping between the two of three of them I can can a direct, honest, and detailed conversation about my personal situation and the recommendations of the ACR.
No, I have never had an MRI. All I've ever had was a 3D mammogram and when the found an issue on the right side they ordered an ultrasound. No MRI. My breast surgeon said it wasn't necessary and it might cause false positives.
I had a lumpectomy right breast with radiation in Sept, and will start Tamoxifen at the end of Dec after my visit with my MO. All these years, all the mammo reports that have listed that I had dense breasts and might benefit from additional screening, not one person - my PCP, my GYN, the breast surgeons I saw for multiple cysts and "suspicious findings" over the years, the dx of fibrocystic breasts, the aspirations, year after year, no one ever talked to me about the benefit of additional screening. I know that is on me, but disappointed also in the health care providers not being proactive.
Beesie - sorry, I knew what you meant. What I wrote came out wrong. Thank you for those links. I got the sensitivity info the the ACR Appropriateness Criteria Report, Variant 5 or Variant 6 section, can't remember, which is specific to the sensitivity of those tests specifically for women with dense breasts (heterogeneous or extreme).
Here's the link, which includes their recommendation of an annual MRI for someone with dense breasts AND a personal history of breast cancer.
https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria
Juju-mar - thanks for the info on the Abbreviate MRI. I did see that in the ACR report. If push comes to shove I will fight for that, it that fails, I will seek a second opinion elsewhere.
I am trying to gather all my records now so that I can prepare for a second opinion elsewhere if need be. That in and of itself has proved to be a bigger task than I anticipated.
Thanks again for everyone's help and suggestions and links. I appreciate the ideas and support.
0 -
macdebbie,
I, too, have heterogeneously dense breasts. I did the annual mammograms. I didn't know MRI was an option before the dx. My first breast MRI was 07/2021, which showed three masses (2.2cm, 1.1 c.m, .5 cm) correlated with the positive cancer biopsy. Although the MRI picked up cancer, it did not show the extent of the tumor. The three masses were one tumor. The Cancer Center recommended I get an MRI each year now. I chuckled behind my mask, wondering why it was never mentioned before with the dense breasts. I understand you can request the MRI from your medical team if it is not offered. Check with your insurance to confirm it is covered now that you have a dx. I think it makes sense to have an MRI annually since it shows more findings though the findings can be benign. I ask for everything. I figure all I can get is a "no" which I am already at without requesting tests.
0 -
I have dense breast also.. I was diagnosed with breast cancer this past August.. I never had a MRI until after they knew I had breast cancer.. and now want me to have one again next year.. I was lucky.. Stage 1, no lymph node involved but they did remove 2 to check to make sure.. The MRI had already showed no cancer in lymph nodes but still took 2.. better safe than sorry I guess.. that right now is giving me the biggest problems.. the soreness under my arm. Had my lumpectomy tumor was only 1.8 cm.. I am still undergoing radiation treatment.. had 12 treatments, 4 more to go..
They want to put me on Arimidex for 5 years starting in January.. I hate pills and fear these.. are any of you on these.. And how are you doing with on them?
0 -
Tasha35 - My next step (end of Dec) is endocrine therapy. I chose to go on Tamoxifen rather than any of the AIs since I already have osteoporosis and didn't want to add a bisphosphonate to the pile of drugs since there are some serious side effects. I also didn't want to take any of the AIs due to the risk of cardiac events that they can incite.
Wondering 44, yes, I will try and check with my insurance, but they require a CPT code to tell me if something is covered and I don't know what that code is. It's good your cancer center is being proactive. I did ask my breast surgeon's office for supplemental screening - I would have settled for an ultrasound but really want an MRI since it's the recommendation by ACR, but they told me supplemental screening is "not necessary".
0 -
macdebbie, thanks for the ACR site - it's really helpful and explains a lot.
First off, it explains why in your case a 3D mammogram is recommended, and not an MRI. While you may feel that with a history of breast cancer and with Cat.3 density that you are "high risk", officially you are not. A history of breast cancer does increase our future risk, but at your age, it does not take your remaining lifetime risk up high enough to break into the high risk category. Even doubling the risk of the average woman your age (that was how my first MO estimated my future risk) only takes your remaining lifetime risk to 15% or 16%. Adding breast density, with your density being Cat.3 and therefore pretty much average for your age, doesn't take your risk up much more. So at best, you might be considered to have "intermediate risk", defined as being 15%-20. (I'm not saying I agree with any of this but am just explaining how risk is assessed - as someone with a history of breast cancer who had Cat.4 density well into menopause and still was not classified as being high risk, I've spent a lot of time on this issue.)
Here is the ACR recommendation for women who are intermediate risk and have dense breasts:
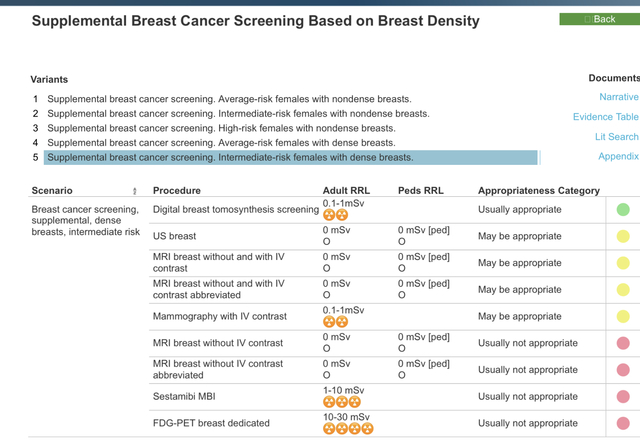
As you can see, the only green dot is for 3D digital mammos. Why? I dug into the narrative and the evidence table. There are lots of studies quoted, including one very small study that found that the effectiveness of mammograms (regular non-3D, non-digital) for women with extremely dense breasts was only 30%. This study is quoted in the narrative but is stated to be the low point of all studies - and again, it was a figure derived for women with Cat.4 density who had regular screening mammos that were not either 3D or digital (I looked at the actual study report).
A more reliable and significantly larger study included in the evidence table is this one:
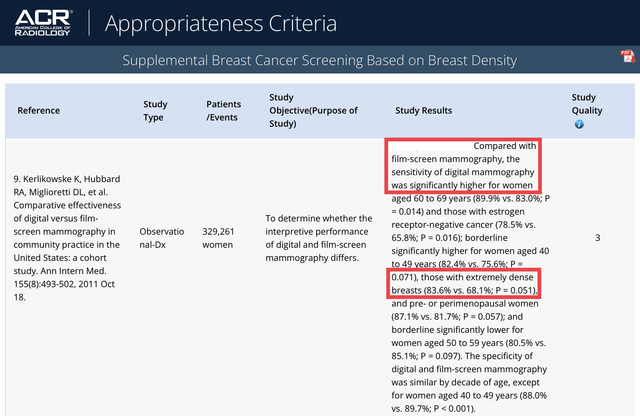
This study shows that for those with Cat.4 extremely dense breasts, 3D digital mammos are 83.6% effective. For those with Cat.3 density, the effective rate would be higher.
And that's why the screening that's been recommended for you is digital 3D mammos alone. Not saying I agree (I don't) but that is what you are up against.
0 -
Tasha35 - I've been taking anastrozole for almost a year now, with no side effects that I have noticed. I also had osteoporosis prior to my BC diagnosis and opted to do twice-yearly zometa infusions to deal with the risks to my bones. Because of the zometa infusions and the distant risk of osteonecrosis of the jaw, I upped my dental check-ups to four times a year instead of twice a year, but otherwise no issues at all.
0 -
Beesie - Wow, thanks so much! I see what you are saying. I appreciate you looking at and clarifying this.
How does all of this reconcile with this statement made by the ACR - "As of 2018, the ACR recommends annual surveillance MRI in women with dense breasts and with a personal history of breast cancer"?
0 -
It's odd how some facilities routinely use MRI and others don't. I had one prior to surgery - I was already diagnosed and had had the mammogram, ultrasound, and biopsy. My surgeon wanted a good look at both breasts "just in case" but also to assist her in seeing the exact location of the tumor. That may have had something to do with it being lobular; it never occurred to me to ask. But from what I picked up from her wording when ordering the MRI, it sounded pretty routine for her to do - and I do NOT have dense breasts. I kind of assumed all breast centers did this. Neither she nor my MO have ordered anything but routine annual diagnostic mammograms since the first year. I did have one off-schedule mammogram and an ultrasound because of lumpy and tender scar tissue, in the beginning of the second year after my lumpectomy. No extra screening since then.
0 -
macdebbie, they are inconsistent. The ACR classify women with a history of breast cancer as being intermediate risk, and their "Appropriateness Criteria" for intermediate risk with dense breasts only show digital 3D mammos to be "Usually appropriate". They do not break out women with a history of breast cancer as being a separate category, nor do they even include a footnote to reference the further recommendation for MRIs for women with a history of breast cancer and dense breasts. It's only in reading through the 20 pages of narrative that this is mentioned, but it comes just after mentioning that the data is not clear and that due to insufficient data, MRIs are not currently recommended by the American Cancer Society for women with a history of breast cancer who have dense breasts. So they seem to be playing both sides. This is where the yellow "May be appropriate" comes in.
Thinking about your breast density.... Although you continue to have Cat.3 density, this doesn't mean that your density is not coming down. In my case, my Cat.4 density was at the high end of the Cat.4 range when I was younger but was right at the bottom of the Cat.4 range, bordering right at 75% density, when I was diagnosed the second time. I'd actually had one mammo a couple of years earlier that put me in Category 3, but the next mammo and all future mammos, I was back up in Category 4. Since it's a judgement call by the Radiologist, anyone right at the edge between two categories could be assessed differently by different Radiologists.
Density does tend to decline once women hit menopause, but it can be a slow process (and of course there are some women who are the exceptions and whose density never declines). But it is possible that your density might have been closer to 75% 10 or 15 years ago and now might be still above but closer to 50%. In another few years, your classification might drop into Cat.2. Not saying that will happen, but that is a normal pattern and the categories are large so remaining in the same category doesn't mean there's been no reduction in density.
All that said, you certainly should push for supplemental screening, whether it's an MRI (ideally) or an ultrasound. Interestingly, in my case, when I was younger and my breasts were more dense, my breast cancer was found on a mammogram and was invisible on an ultrasound. 13 years later, when my breast density was lower (although still extremely dense), my breast cancer was invisible on a mammogram but was spotted on an ultrasound. The difference was in how the cancer presented - the first time as calcifications (which rarely show up on ultrasounds) and the second time as a small mass (obscured by my dense bresst tissue on the mammogram). So I'm a strong believer that all of us who've had breast cancer should receive 2 modalities of screening.
0 -
I also have heterogeneously dense breasts and, after receiving a letter informing me I had dense breasts and that mammography may not be a sufficient imaging modality, (like you, NOBODY talked to me in person or on the phone about this — I think imaging centers don’t want to cast doubt on mammography as they have millions invested in these buildings and equipment and the techs that operate them) I asked for an order for an MRI from my PCP. She obliged. I would not bother with your surgeon and make a request of your PCP. Doctors are supposed to be practicing patient-led care now. I can see how you shouldn’t be rubber-stamping everything a patient wants, but, as delay to diagnose breast cancer supposedly is the No.1 reason behind medical litigation in the U.S., I think it is a rare U.S.-based doctor that wouldn’t acquiesce to a request for breast imaging.
There are various websites offering discounts on MRI so look into that if you will pay out of pocket. I was cajoled by my doctor into going to the hospital for mine and it cost a relative fortune vs. the MRI clinic next door. Then the hospital tried to bill my insurance a crazy amount and told me they’d foist it onto me if they didn’t pay. I threw a fit. Now my doctor says, “I don’t care where you go, so long as you get the MRI.” If they try and get you to do it at a more expensive location emphasize harder you need to save money. Wish I had pushed harder for the clinic.
0 -
Hi,
In the past four years, since my diagnosis, I have been classified as having dense breasts 3x out of four after mammograms. This seemed a bit random to me, and my surgeon’s PA who follows up after mammograms told me that two radiologists can look at the same mammogram and come to different conclusions. But I’ve always been told that I have dense breasts with lumps, so we just wrote that one report off as an outlier.
I’m scheduled for a diagnostic mammogram next week (with ultrasound if needed). My experience is to trust the mammogram, because my cancer was picked up by one after two doctors said that the lump I had found “didn’t feel like a cancerous lump.” They were both surprised when it turned out to be cancer.
With dense breasts it can be hard to know which lumps feel normal. But a 3D diagnostic mammogram with an ultrasound gives me peace of mind because of my experience four years ago. The breast center here doesn’t recommend MRIs routinely.
0 -
@thedisgruntledpatient - interesting comment about the MRI site. My insurance refused to cover it at the hospital but would cover it at an imaging center. The only difference would have been that I might have gotten in a few days earlier at the hospital because they have extended hours and probably more capacity. I work at a large company that self-insures, so they're cost conscious for their own purposes, but it benefits the employees during the deductible phase.
0 -
Well mine was at an imaging center, but owned by the hospital a stone’s throw away, so I consider that a hospital MRI.
Should have listed the discount website I know of. It is Radiology Assist. There are a few MRI clinics near me that have a deal with them. You pay through RA but cost is reduced from retail price by about $150.
0 -
Beesie - quick question if I may. My BCS told me that after genetic testing since I had no mutations, my risk of a NEW breast cancer. (not recurrence) was 1% a year. Considering my living potentially into my late 80s or at least until 84, doesn't that give me a 20%+ lifetime risk?
I am not clear how this gets calculated.
0 -
macdebbie, yes, a 1% risk per year would add to more than 20%. But honestly, that sounds a bit like a throw-away line from your surgeon.
When I was first diagnosed 16 years ago, many of the articles stated that the "risk of a new primary" for those previously diagnosed was in the range of 0.5% to 1%, depending on other risk factors. In the time since, more studies have come out that suggest that the figure is probably closer to 0.5%, particularly for those who have an ER+/PR+/HER2- cancer. So the models that are used to determine future risk would not assume 1%, which is why the ACR puts all of us who have a history of breast cancer into the intermediate risk (15%-20%) category. The exceptions would be those who are diagnosed very young, because they have enough years ahead of them that a 0.5% annual risk would bump them into the high risk category, and those who have high risk genetic mutations, such as the BRCA mutations.
The other factor to consider is that risk is not the same at every age and the timing of the first diagnosis factors in. Breast cancer risk is highest for those of us in our 60s and 70s, but drops down after that. So it would never be 1% (or 0.5%) per year for every remaining year of life. This is why it's relatively common to see younger women diagnosed again as they enter their higher risk years, but it is less common to see those diagnosed a first time when they are older get diagnosed again. Having been diagnosed a first time at age 49, I knew that my risk would be very high when I was in my 60s, and sure enough, I was diagnosed again. Off the top of my head I can provide a long list of others who were diagnosed at around the same age as me, who also returned here with a second diagnosis after 12-15 years. But I have seen very few women who were diagnosed in their prime breast cancer years (60s and 70) who've been diagnosed again. Not saying it doesn't happen and it isn't a risk, but the risk does not appear to be a high for those diagnosed once they are already post-menopausal.
0 -
That makes me feel a little better, thx.
0 -
I also have dense breast tissue. My primary doctor never mentioned extra screenings or MRI etc. to me regarding my high risk for breast cancer. I was always terrified of mammograms. I did my baseline mammogram early, then I did one or two more. I did not go back as I should have to continue my screenings. Once diagnosed with my breast cancer last year, my surgeon talked with me about my dense breast tissue. My oncologist still stands firm on his recommendation of me having yearly mammograms. I am going to insist on diagnostic mammograms and ultrasounds every six months. If I need to work out a plan to alternate screenings between mammograms, ultrasounds or MRI so that my insurance will cover it, I will do that. I am now an advocate for self breast exams. I found my breast cancer myself. We have to advocate for ourselves and do what we know is best for our health.
0