Starting Radiation December 2019
Hi All,
I will be starting radiation today. Just started the thread for folks starting radiation in december.
Comments
-
Hello
I will have my setup on December 10th and start radiation on December 17th.
0 -
Hi Neeli and ChaClarey and all other December RADs warriors....
I just wanted to stop by and wish you all good luck on your RADS journey. I finished my RADs on Halloween in 2018. Though my experience in RADs was a "bit" rough, and I ended up with Fibrosis, a broken rib, Breast Lymphedema, and Rib Dysfunction (Costochondritis), many others in our Oct 2018 group did just fine and so have many other members since! The odds are in the favor of y'all having minimal SEs .

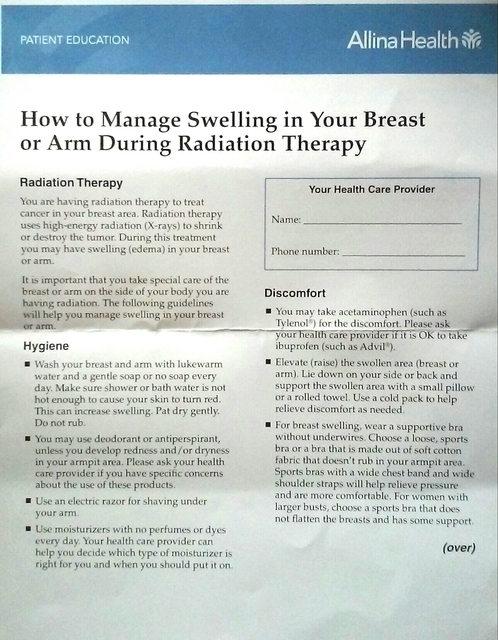
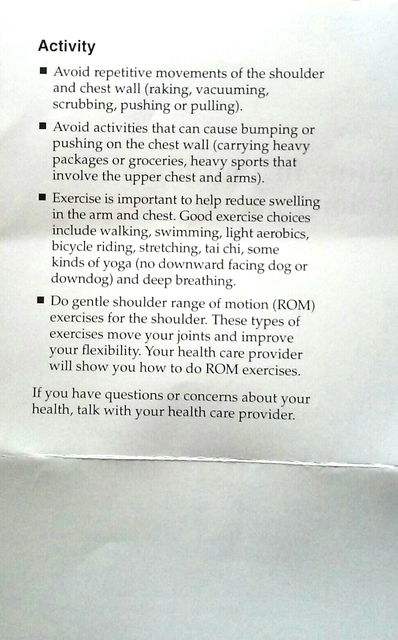
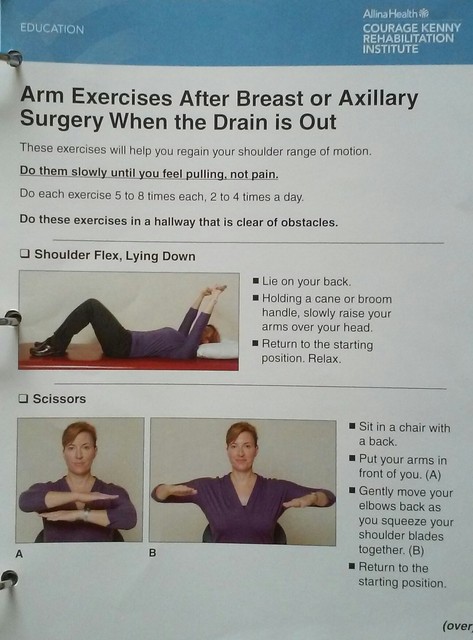
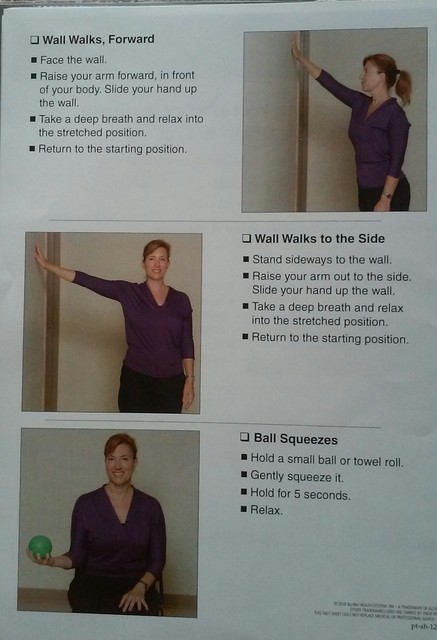
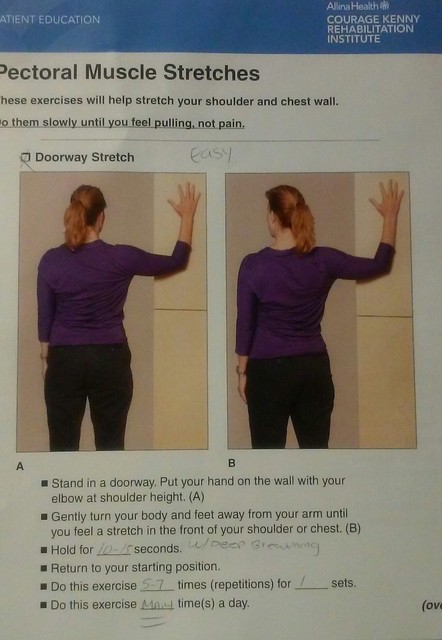
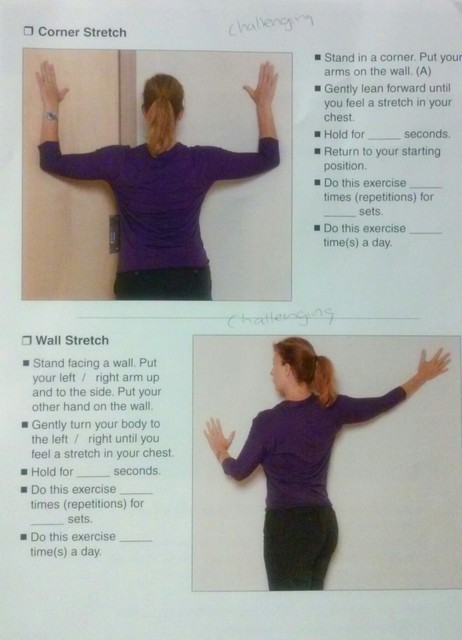
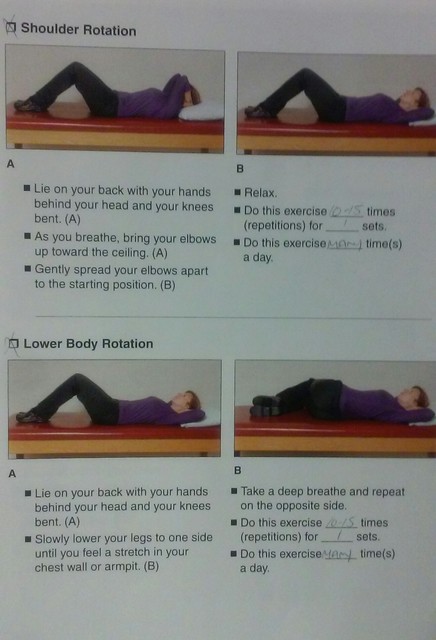
I was given many stretches and exercises by my Cancer Rehab PT and RO that helped me to keep from losing range of motion and manage the Breast Lymphedema that developed during my RADs treatments, which I had posted in my RADs group and I'll share here too in case anyone might find them helpful. Two rules of thumb - go slow and gentle and If in doubt, ask your team. Always.
Oh and before I forget, there's a really great link about What To Expect During Radiation from the Memorial Sloan Kettering Cancer Institute that MissouriCatLady in her June RADs thread and she was right!! it's really full of good stuff, things I wished someone had told me before I started too. Give it a look see, can't hurt.
Also, if you've not read this thread yet, List of what to do/get/pack to prep for Radiation Therapy, it's also a good place to go for tips and tricks on what helps during the next few weeks.
At the end of this post, I've shared some info/sites/videos about Gated Radiation (where you need to hold your breath). I had to do this due to my Left Sided BC in order to help protect my heart from the RADs. Some of you may need this and hopefully these resources will put your minds more at ease.
Ok, sorry to drone on. Think I'm nearly done! I sure hope all of you will sail through treatments with the minimum of SEs. This was our thread Radiation October 2018 and we discussed quite a few things that were very helpful along the way - including different creams, hydration, NAPS, exercise, etc. Maybe it might be helpful to you on your journey too.
My best advice that I can pass on, that helped me is this:
1) Start using Calendula or other creams 2 weeks prior to treatments on the area of RADs (if one breast, be sure to get up into the armpit and into the ribs as well). This is what my RO asked me to do. Continue as your team directs you, most of ours seemed to say 2- 4 times depending on various SEs.
2) Drink lots of water.
3) Walk or move as much as you can, given your own limitations.
4) Double check with your RO/team about meds you are on, as some on my list were ones I shouldn't take before AND during RADs & after for at least 2 weeks (antioxidants especially).
5) Everyone is different. Some experience SEs immediately (like me lol), others sail by with very minimal SEs. If you are concerned or experiencing pain/redness/swelling/heavy feeling/etc, don't be afraid to speak up to your team. That's what they are there for!

6) If you do experience SEs, one of the things that SAVED me was "Boob Lasagna" - whuch us a cream called Aloe Vesta that's layered on with special gauze and then wrapped under a compression bra. I think I would have lost my mind the last 2 weeks without it. Ask your team. Also, you can find it on page 6 of the Oct Rads Group.
Ok all, hope this will help you all a bit on your RADs journeys.
Wishing you all the best and quick healing after you get to ring the bell! Good luck Warriors! You got this!


Breath Holds (Gated Respiration or DEEP INSPIRATION BREATH HOLD (DIBH)
This might be something some of you will have. I did. It's usually used for left sided BC to keep the heart out of the way of the RADs.
I was afraid I was going to screw it up somehow. What helped me was asking my RADs techs about this directly. For me and the machine I was being treated on, they input thousands of data points from all my imaging info from the "setup" (plus recalibration for each treatment and a new scan each week) and other mumbo jumbo I couldn't hope to ever comprehend into the computers that run the machine and it established a "parameter" for me, a gate.
If I, through holding too much breath, not enough, or couldn't continue to hold my breath any longer for whatever reason, the machine automatically shut off in a nano second when I "fell" out of that parameter (gated) range. Hearing that made me feel a ton better about the role I played in potentially screwing the treatment up and accidentally radiating my neck, brain, foot, whatever. LOL.
Good explanations can be found here:
https://www.verywellhealth.com/respiratory-gating-for-radiation-therapy-with-breast-cancer-4154077
A couple of good videos on YouTube are here:
"Deep Inspiration Breath Hold with VisionRT System" https://www.youtube.com/watch?v=JLWaTFHkCXA (I like this one because it shows exactly HOW the computer knows WHEN to shut off the radiation!)
"Deep Inspiration Breath Hold Technique" https://www.youtube.com/watch?v=n6jXkgLnNnY
"Deep Inspiratory Breath Hold (DIBH) Treatment" https://www.youtube.com/watch?v=oU8TE0fvqMgHopefully something here helps ya'll get through the rest of the RADs in your plan.
0 -
I had my setup on the 10th. It took about an hour and was pretty easy. I had my five tattoos and needles stung but nothing serious. I am doing the deep inspiration breathing as radiation on left side. This is supposed to reduce radiation to heart. I asked tech if some of my heart still in range and he said a tiny bit. I’m not sure what tiny means in medical terms but will ask the radio oncologist. I asked if there was anything else I could do to reduce this exposure and he said no. I was feeling a little low after appointment due to info on heart And that I will be only doing five days for two of the five weeks due to Christmas and New Years holidays. I will 1 week of 3 days, 2 weeks of four days, and two weeks of five. The optimal is five days a week and 8-12 weeks after lumpectomy. It will be 13 weeks as I had two sentIntel node biopsies as none were in initial sample and I was awaiting Oncotype results to determine chemo. I went for walk afterwards to try to clear some negatives thoughts and it helped at time, but doubt and discouragement still creeps in at times. I will be happy to get started with rest of December’s
0 -
I start my radiation on Monday! I’ve worked in radiation oncology for 20 years so this is really weird for me to be on the other side of things. I might be the worst patient they’ve had because I know too much!
0 -
Deweygirl19,
I hope all went well on Monday. It must be surreal to be on the other side.Neeli,
I hope things are going well for you too.Spoonie77
Thanks for all tips and adviceI have done 2 sessions so far and will be finished January 16th if all goes well.
0 -
Hi All,
I was allergic to aloe vera and developed red bumps all over in the first week of radiation itself. Now using calendula its better. I get tired by late afternoon/evening.
0 -
thanks ChaClarey, it went well! I work with a great team who I trust, literally, with my life. Very quick and easy. 5 fx down 31 to go!
0 -
I just wanted to check in and share that I had my first radiation treatment 10 years ago today. I was lucky as I was able to do the shorter protocol which was about 19 rounds total. Can't suggest aquaphor enough...i slathered it on and applied it about 3 times a day. Wasn't working so I just wore a big, huge Tshirt. Good luck to you all.
0 -
Hello December’s
Neeli, I hope your skin is doing better.
Deweygirl19, I’m glad it went well.
Cowgirl13, thanks for the check in and advice.
I have 4 down and 16 to go, so far so good. I am using Cavilon barrier film on advice of radiation tech.
0 -
Hi All. I started radiation 12/16 and will have 15 treatments. Thank you all for sharing experiences and advice. Today was treatment #6 for me. Skin is ok, I guess. I find it disconcerting that out of nowhere it will start to burn, hours after treatment. But so far cream has helped. I have been warned that fatigue is a bigger problem for many people. I have added a protein shake to my daily diet and am crossing my fingers that it will work. (p.s. I didn't know that Trader Joe's sells protein shakes!)
0 -
michrsm, are you applying lotion immediately after you finish radiation treatment? I applied lotion when I was dressing immediately after radiation. I didn't have the burning feeling starting later like you are - but we all get different side effects.
0 -
Ideweygirl19 : I am curious what you found regarding left side breast cancer and Heart and lung exposure. I think it is difficult to have this problem as a health professional, I am a RN. I would have preferred to be ignorant. I don't work in RO and am not an expert. I think the radiation oncologists don't talk about all side effects because if we knew them all, we wouldn't do it. I have delayed it because 1st of all I am scared of long term side effects, but also I am older. 69 this year. By the time I have my simulation, it will be 7 weeks after surgery. I am still not 100% sure I am going thru with it. Any insight would be appreciated.
0 -
Redhead: I had left sided radiation to chest wall six years ago. It was optional for me and I really struggled with the decision and researched everything. What I can say, is stats about risks are way out of date. Left sided radiation is similar to right sided radiation for risk factors. Technique is so much better. But it is not risk free. Nor is avoiding radiation. Hate how difficult these decisions are. Have serious discussions with your health team. And then factor in your personality and tolerance for risk and SE’s. A pro con debate is the reality. Wish a best practice was obvious. Hug
0 -
I had left sided radiation 10 years ago and I am just fine. I was 63 at the time.
0 -
Redhead - I am only 5 months after my full breast radiation on the left side. I had lymphvascular invasion, so I felt that having radiation was important. I read a study that said that "breath holding" reduces damage to heart significantly. The first radiation oncologist I went to did not believe that breath holding made a difference. So, went with a different radiation oncologist. I found out towards the end of radiation when I couldn't see the "breath holding box" that was projected on the ceiling after they moved the machine that they actually monitor how well my breath holding is working as they verbally coached me to relax my breath just a tad, etc. I've had PCP, med onc and rad onc all listen to my heart and lungs in the last two months and none of them expressed any concern. I am not aware of any long term negative side effects yet.
0 -
My tumor was small but I had a positive superior margin which is why they want 20 treatments plus some boosts thank you DorothyB , cowgirl13, and TB90 for your responses The heart issue could be damage to the left. Anterior descending coronary artery. No symptoms noted for 5 to 10 years. It's a long-term side effect that is late. Thanks again.
0 -
I did the 'breath holding' protocol with my radiation. It was really easy. Also wanted to say that after my treatments, as I was changing into my clothes that is the time I would generously apply the aquaphor. I basically wore extra large t-shirts.
0 -
Regardless of breath holding or other techniques (it really is determined by the skill of your RO who sets up the initial measurements), long term SE to heart and lungs is minimal. According to research. I keep a close eye on the research for personal reasons. Lol. Personally, due to an exercise regime, I am in far better shape now than at dx. I did have a total thyroidectomy almost one year ago as I rated a Tirads 5. Benign! I researched that association to death also. No definitive association. But some suggestive studies. I find some comfort in having had rads when others with DCIS have recurrences in same breast, but I also worry about secondary cancers, etc. My BS’s advice was, “if you go ahead with radiation, make certain you have a damn good RO”. That’s what can make the difference.
0 -
Hi all. I just started radiation yesterday (yes, the day after Christmas!). I am getting 30 days on both sides which includes 5 boost treatments. I may be imagining things but my skin already feels itchy and swollen (after only 2 treatments). I used aquaphor right after and calendula cream before bed.
I must admit I struggled with this part of the treatment more than the others (I did chemo, then hormone suppression, then double mastectomy and now radiation). But it has started and now I am eager to get this over with!
Terry
0 -
Tldougan, I started radiation on the 26th also and am experiencing the same thing! Today I had my weekly follow up with the doctor and he said *usually* the skin irritation does not start this early but he didn't discount me. He said there's always that person who doesn't respond like everyone else. It does have me concerned about what things will look like by the time I'm done. 🤷
I saw a woman at my appointment today who had a large, open, peeling wound on her back due to radiation. I'm not going to lie, it made me so nervous. 😣
0 -
redhead403- I can’t speak for what every doctor does but at my clinic they do deep inspiration breath hold for left sided breasts to reduce dose to the heart. We also do a treatment technique called IMRT (intensity modulated radiotherapy) that allows us to reduce lung and heart dose. This is more expensive and insurance doesn’t like to pay for it but are more willing for left sided breasts. The rad onc I work for gives a larger boost dose for positive margins or close margins. I’m getting more because my margins were close. As for heart dose it really depends on your body habitus (or placement of your organs) each person is different. Some patients hearts are far away from their chest wall. Some patients hearts are right up against the chest wall and even taking in a deep breath doesn’t move the heart away much. My rad onc dr is very specific where he puts the borders to reduce dose to lung and/or heart no matter which breast we are treating. We do so much more now to reduce doseto lung and heart than we did 20 years ago.
That being said there is always a risk of late effects from radiation. You have decide what’s right for you. I hope you have a doctor willing to talk to you about all of your fears.
0 -
Thank you Deweygirl19 She gave me the option of prone or supine. She called me right after the simulation and said that the prone position moved my heart in to the area of radiation. When I go back thursday for a "dry" run, the RO will show me the CT. I just have one other question, and that is I am receiving fractionated ex beam therapy. I had margins that weren't clear. Do you have any idea why I wouldn't be a candidate for Hypofractionated therapy? I plan on asking Thursday. Just wondering what the rationale might be, as she never gave me a reason, just no hypofractionated. Thanks in advance.
0 -
redhead403, I have copied this article on hypofractionated radiation therapy from our BCO site here.
New Guidelines Say Accelerated Whole-Breast Irradiation Should Be Used to Treat Most Breast Cancers
The American Society for Radiation Oncology (ASTRO) has put out updated guidelines on whole-breast radiation therapy.
The updated guidelines say that most women diagnosed with breast cancer should be treated with accelerated whole-breast irradiation as the standard of care. The new guideline greatly increases the number of women recommended to have accelerated whole-breast irradiation.
The updated guidelines were published online on March 12, 2018 by the journal Practical Radiation Oncology. Read "Radiation therapy for the whole breast: Executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline."
The new guideline replaces the ASTRO guideline released in 2011, which recommended accelerated whole-breast irradiation for selected patients only: mainly women 50 and older when diagnosed and women diagnosed with breast cancer that was small and had not spread to the lymph nodes.
Women diagnosed with early-stage breast cancer who have lumpectomy to remove the cancer usually have radiation therapy after surgery. Radiation therapy after lumpectomy lowers the risk of the cancer coming back (recurrence) and makes lumpectomy as effective as mastectomy.
Whole-breast radiation therapy after breast cancer surgery is usually given as one treatment per day, 5 days a week, for 5 to 7 weeks. A Gray is the way radiation oncologists measure the dose of radiation therapy; if you're on a 5-week treatment schedule, 50 Gray is the usual amount given during the 5 weeks (2 Gray at each treatment). A supplemental "boost" dose may be included at the end of the regimen that targets the area where the cancer was.
Radiation treatment schedules were developed based on research results. But a 5- to 7-week nearly daily commitment may be difficult for some women, especially if they live far away from a treatment center. So doctors developed and studied a different radiation therapy schedule that involves fewer treatments with higher doses of radiation at each treatment, but the same total radiation dose. This accelerated, or hypofractionated, radiation schedule puts the same radiation dose into a 3- to 5-week schedule.
A hypofractionated whole-breast radiation schedule is appealing to doctors and people getting radiation for several reasons:
convenience: arranging daily trips to get treatment can be a problem for some women; fewer treatment days or a shorter period of time may be easier to schedule
if radiation is more convenient to schedule, it's probably easier for women to get all the recommended radiation therapy
"Recent long-term results from several large trials strongly support the safety and efficacy of accelerated treatment for most breast cancer patients," guideline task force co-chair Benjamin Smith, of the University of Texas MD Anderson Cancer Center in Houston, said in a statement. "Conventional therapy does not provide an incremental benefit in either tumor control or side effects compared to hypofractionated whole-breast irradiation."
To write the updated guideline, ASTRO experts reviewed 100 studies on hypofractionated whole-breast irradiation published between 2009 and 2016.
The guideline provides doctors with guidance for dosing, planning, and delivering whole-breast irradiation with or without an additional boost. Key recommendations in the guideline are:
Treatment decisions, including decisions between hypofractionated and conventional whole-breast irradiation, should be personalized for each patient.
The preferred hypofractionated dose schedule is 4,000 Centigray (cGy) in 15 doses or 4,250 cGy in 16 doses.
The decision to offer hypofractionated whole-breast irradiation should not depend on:
cancer grade, whether the cancer is in the right or left breast on previous chemotherapy
or previous or current treatment with Herceptin (chemical name: trastuzumab) or hormonal therapy
or breast size
For women diagnosed with DCIS, hypofractionated whole-breast irradiation may be used an alternative to conventional dosing.
For women diagnosed with invasive breast cancer, a boost to the area where the cancer used to be is recommended for cancers with positive margins, women who are age 50 or younger, and women age 51-70 with high-grade breast cancer.
For women who are older than 70 with low-to-intermediate grade disease, and women with hormone-positive disease with wide negative margins, a boost to the area where the cancer was is not recommended.
For women diagnosed with DCIS, a boost to the area where the cancer used to be is recommended for women age 50 and younger, women with high-grade cancer, and women with positive or close margins.
Three-dimensional conformal (3-D CRT) treatment planning with a forward planned, field-in-field technique is recommended.
"These guidelines apply to most women diagnosed with breast cancer," said Marisa Weiss, M.D., Breastcancer.org chief medical officer and radiation oncologist. "There are some exceptions, however. The ability to deliver a larger daily dose requires that your doctor design a radiation treatment plan that is very even throughout the whole area of the breast. Sometimes this is hard to achieve. In women with very large breasts or who have a large chest size, it may be hard to achieve an even dose, so your doctor may recommend a traditional dose schedule of 5 to 7 weeks.
"It is important for each person to get the best care possible for her unique situation," she continued. "The hypofractionated schedule is likely more convenient and less disruptive in your busy life. Still, if you have to have a longer treatment plan, don't think that this means you have a worse situation or worse outcome. These guidelines have no impact on prognosis or how well you do."
If you've been diagnosed with early-stage breast cancer that has been removed with lumpectomy and radiation therapy will be part of your treatment plant, it makes sense to talk to your doctor about the new ASTRO guideline and whether hypofractionated whole-breast irradiation makes sense for you and your unique situation.
It's also a good idea to talk to your doctor about skin reactions to radiation -- together you can develop a plan to ease any skin irritation that happens during and after radiation therapy.
0 -
Cowgirl13 Thank you for the info. I am going to take a copy with me to The RO tomorrow, I do want to understand why I am not receiving hypofractionated radiation.
0 -
redhead, you are welcome. I've wanted to know more about this as I had the hypofractionated radiation10 years ago.
This is what really interested me (from the above article):
"There are some exceptions, however. The ability to deliver a larger daily dose requires that your doctor design a radiation treatment plan that is very even throughout the whole area of the breast. Sometimes this is hard to achieve. In women with very large breasts or who have a large chest size, it may be hard to achieve an even dose,
Good luck and don't forget you can always have a second opinion.
0 -
redhead403, glad your doctor is on top of things! I know most rad oncs offer hypofractionation to most women. Mine doesn’t, he’s very conservative and worries about late side effects to skin from the higher dose per day. He only offers it to DCIS, no positive nodes, over 50 years of age. I’m not getting it, (I’m IDC and under 50) but as I work there it isn’t exactly a burden for me to get my treatment each day, I just walk down the hall! I don’t blame anyone for wanting to get it over with faster. My breast surgeon and med onc were surprised I wasn’t getting hypofractionation. As someone who creates all the treatment plans I can also say we can’t always get a good plan for all women we offer and have to go with traditional fractionation for those, like the above says.
0 -
I also am not getting hypofractionaction. Not sure if it is offered here - but I am large breasted and also am getting full breast radiation and axial and some clavical radiation because I had micromets in my sentinel lymph node and slight lymphovascular invasion so it might not have been the best anyway. I just had the positioning visit Monday and a CT then they will start radiation next week after they do their calculations.
My radiation center has only been here 5 or 6 years - prior to that there wouldn't have been a radiation center within 600 miles. As it is I drive about 15 minutes to get there so the longer time is not an issue. At least I say that now. The ceiling above the radiation machine has light panels which are currently showing cherry blossoms. I didn't ask if they change them but I guess I'll have them memorized in a few weeks.
0 -
I'm 6 in for 20. Slight breast pain and some fatigue. Trying to exercise but anything that jostles my breast around hurts. Using calendula afterwards and then aquaphor at night.
0 -
Halfway done of 20 sessions( 15 plus 5 boosts) Nipple is pretty red and sensitive. A few jolts.I have been using Cavilon spray. Feeling a bit tired but not too bad. Back to work next week. Hope everyone else doing ok.
0 -
I'm now 8 treatments in my skin is starting to get red and itchy. Has anyone tried ice packs?
0