Vent about Permanent Neuropathy
Comments
-
That is so true. Vent away, those of us dealing with the reality of neuropathy being a permanent part of our life need a place to go. Like so many other things, you can't understand until you're living it. To think every time before you get up if you want something badly enough to walk across the pain it will take to get there. Every single morning, every morning, havine the ear rings you wear determined by what you can put in. Not putting up your hair because bobby pins and neuropathy don't mix, dropping things in the kitchen all of the time so that the floor and counter cleaner and paper towels take up a permanent spot on the counter at the side of the kitchen. To say nothing about the drive to a different job because you can no longer do what you used to do. Watching your feet every where you walk because your balance is terrible and you won't feel changes in the side walk that will land you doing a face plant.
Or----scalding yourself because a toe or finger don't recognize how hot the water is. Looking down and wondering where the blood is coming from and realizing you stepped on something or picked up something and cut yourslef (back to the look with all the cleaning products out and ready on the cupboard).
And some days, you just wish for a break from the pain
0 -
Hello all!! I would love your opinions/advice. I am going to call my primary this week for perhaps some referrals (and maybe my onc after talking to primary). I did not have any issues with neuropathy/feet/hands during chemo...had cytoxan/taxoteere 4 teatments. After radiation I noticed alot of aches and pains (finished two months ago) but alot have gotten much better, had pain/burning on sides of my feet and across the top, left foot has stopped completley, right foot continues (non radiated side). In the past I have dealt with plantar fasciitis, been fine for 5 years. Diabetes does run in my family, I have been ok, checked yearly. Any ideas? suggestions? I have tried many shoes, sneakers, inserts, expensive ones at that, and every couple of days it comes back, burns for a few hours, and disappears. Never had any of the burning before chemo/rads..the gift that keeps on giving...ugh!
Thanks for listening!!
0 -
Rads can also cause of worsen neuropathy. So I would go see your PC or your MO for their opinion.
We had our family vacation at the beach. I can say it was much better than last year. However I did notice on the last day how much my neuropathy is effecting my life. Yes if I would loose this weight it would help. The last day I stood on the beach letting my girl boogie board for a few minutes and then we went for a walk. We didn't even make it from my lifeguard chair to the other before I had to turn around. I knew my right leg bothers me with weakness I just didn't realize how numb it can get while out in the heat. Walking on the beach I realize I was dragging my foot behind. I was actually scared I wouldn't make it back to the pool. I was never so happy to jump into that cold water and get a little less numb.
So I guess I have been managing it well by staying in the house during this unusual hot hot hot summer. I can't wait till fall.
0 -
I've posted my first installment of my NYC Memorial Sloan-Kettering Cancer Center Rehab and Dr Stubblefield evaluation at http://community.breastcancer.org/forum/69/topic/762916?page=2#idx_56 if you'd like to follow along with this adventure in surviving survivorship
Stay Strong,
Cindy0 -
Cindy, I read your post on the other thread - thanks for the update!!! What an incredible visit... we may not individually benefit from this type of visit, but it can certainly help educate our young doctors in training and hopefully help avoid some of this crap for others!
0 -
MSKCC Rehab - second installment -
Tuesday, Aug 16th, I had my first Occupational Therapy session. It was mostly information gathering for the therapist, and a few measurements. Several were related to range of motion and flexibility. Another was sensory - a series of pen-like gadgets (5 or 6), each with varying size fiber attachments, from the thinness of a hair, to the thickness of a drinking straw. With my eyes closed, each size was touched to different points on each finger and hand to determine what size I could feel. Right hand could only feel the thickest one (drinking straw like) fiber, and only in a few spots. Left hand could only feel the middle sized fiber on fore and middle fingers. And the next thicker fiber on other two fingers. After that, she had me squeeze a hand held gadget that measures the strength of grip in lbs of pressure. The right hand gripped at its maximum 13 lbs of pressure. The left hand gripped at its maximum 45 lbs of pressure.
Wednesday, Aug 17th, was my EMG/nerve study with Dr. Stubblefield. An electromyogram (EMG) measures the electrical activity of muscles at rest and during contraction. A nerve conduction study, measures how well and how fast the nerves can send electrical signals. Not a very pleasant test, but certainly not the worst either. The overall study took 2 ½ hours.... I am very sore this evening.... muscles and nerves are very unhappy with those studies. The result is confirmation of RIBP (Radiation Induced Brachial Plexopathy) and Radiation Induced Fibrosis. Damage is more extensive on the right side, entire neck, and both shoulders. The Brachial Plexus has 3 main sections. The lower section is severely and extensively damaged by the radiation, which killed the nerves by stripping the sheathing off, causing them to short circuit, burning up the nerve cells. This lower part of the Brachial Plexus affects the hand/fingers. The middle portion of the Brachial Plexus is also damaged, in the same way, but not quite as severely. This middle section affects the forearm. The upper section of the Brachial Plexus, pertains to the upper arm. I do not have much damage to that section, so my upper arm may retain more strength. Loss of right hand usage will continue and eventually become a dangling arm extension. Forearm will continue to become weaker, and not be much more useful. Neck and shoulder weakness will also progress. The weakness is caused by the inability of the damaged nerves to feed the muscles. The nerve cells that have been destroyed are unable to repair on their own or with any medical/science treatments. Since the muscles can't be fed, they too die, which is the atrophy. No CIPN (Chemo Induced Peripheral Neuropathy) findings - which is good. Lower leg weakness, paresthesia and foot drop are stemming from my lower back, possibly where I had surgery/fusion in 2003.
I am going to be fitted with a neck support that simply acts as it sounds. I'll use it when I tire or am sitting up for more support, less fatigue on neck/shoulder muscles. Also, I will be fitted for lower leg/foot braces to help with walking and providing foot support. So, prognosis isn't great - but at least there are items to help, and range of motion/core strength/stretching/posture building PT/OT to build on. I need lots of help with that, and this is definitely the place to get it.
I asked Dr Stubblefield about stem cell regeneration, and if it is a possibility for this kind of nerve damage - sadly, he shook his head no, and said it is not anywhere in the works for this survivorship problem.
I have a full spine MRI and a brachial plexus MRI scheduled next week for further diagnosis and definitions.
Dr Stubblefield is amazing, as is the entire MSKCC Rehab PT/OT team. I have been given so much attention and assistance and information in just the first 3 days, I feel my head will explode - in a good way. Cancer survivors are living much longer than before, and they are just discovering the intensity and magnitude of the long term effects from treatments. Focus now, is improving the quality of the life that's been saved.
More to come after further PT/OT and MRIs completed...
Stay Strong,
Cindy
0 -
I feel your pain. I have chemo induced neuropathy in my hands and feet. I have two choices.
1) Walk and feel as tho I am walking across a frozen tundra.
2) Sit or lay down and wait for the shooting pain to start.
To ease the sensation of popsicle toes, I wear down filled booties. It has been 8 months since chemo was stopped account neuropathy. My feet and hands are marginally better.
kwag
0 -
so sorry Cindy. So glad you are getting some great help.
Kwag....I too getting the shooting pains when I am resting. I can go all day but sit down and get comfy...
0 -
Kwag and kittydog, I also notice feet much worse after being up all day, but also in the morning when I wake up before I have gotten up. Fingers same way except much exacerbated even DURING activity such as typing, but really flared up big-time after I cleaned my filthy kitchen. Choices.... just couldn't stand seeing the grunge around the base of the faucets and DH just doesn't see it at all to clean it. Kitchen looks great again, hands will be better tomorrow I hope. Starting back on topical cream tonight.
0 -
MSKCC Rehab - third installment -
Middle of week two in NYC - Memorial Sloan Kettering Cancer Rehab - Both MRIs are completed. It'll still be a few days till the results/reports are received.
I was fitted for and received the lower leg/foot braces and neck support on Friday. The leg/foot braces may need to be adjusted. And the neck support will need some getting used to - both are not to be worn all the time, just when most needed to aid when doing more walking, and when my neck muscles tire from holding my head up during the day.
So far, I've had 12 total sessions of physical, occupational, and manual manipulation therapies - learned so much in this short time. They always give me printouts with detail pictures and instruction on each exercise. It's a good thing they do - chemo brain would never be able to remember it all! I had to by a binder with sheet protectors to keep all the exercises in. There are many posture correcting exercises I can do on my own, that help stretch and position my shoulders and neck. Most are very simple, yet very beneficial. Breathing from the diaphragm is helpful for core strength. Using the diaphragm allows deeper breaths and better posture. Remembering to sit and stand erect as if there is a string pulling my head straight up to the ceiling. Squeezing shoulder blades together while leaning against the outer corner of wall. Pushing each shoulder against a towel along the edge of a wall corner, while keeping my body straight. Multiple hand flex and finger coordination exercises, some using play-doh type putty.... I always liked play-doh! There are strength exercises to help maintain my upper arm muscles, as they are least affected by the nerve damage. These are more isometric, not using any weights. The weights dramatically increase my stinging paresthesia pain and what I call "bee stings" in fingers/hand. The PT manual manipulation is incredible... she is able to get down into the tissue, with very little pressure, but so exact in positioning that it has already helped loosen my bound shoulder from my neck. Amazing. She gets into my neck/head at just a couple points, and it makes a huge beneficial difference. Learning again how to use leg muscles that haven't been used properly in quite some time is a big challenge, and probably the most physically demanding. The entire plan will be brought home to continue. Suggestions on therapists at home were even provided, based on their completed levels of training and knowledge. Goals of feeling better and enhancing quality of life are being met.Learning to sleep on my back is still taking time to get used to - sleeping in a hotel bed isn't helping either - back sleeping is best because it opens your chest for better breathing, and helps keep the shoulders stretched out, much better for back health. Its important to use a flat head pillow, and be sure to place it above the shoulders, so it isn't pushing your shoulders forward. Placing pillows under the legs helps keep the natural curve of your back. Once you are in a comfortable position, there should not be much movement through the night. A long restful sleep - what a concept?! Sleeping on your side can cause the shoulders to fold inward, allowing them get into the position that only encourages them to want to stay that way - binding the scar tissue/fibrosis even tighter.
Two more days of therapy and learning to go - then I head home to continue on this path of rehab and QOL goals. This has been incredible - thanks to the MSKCC rehab medical staff - thanks to my life partner - thanks to my supportive friends who came on this journey with me - thanks to the internet for providing so much knowledge at my fingertips, and connecting new friends for support and knowledge sharing..... let's see, who is that? Al Gore??? LOL
More to come after I get home and have the results of my MRIs.
Stay strong,
Cindy0 -
MSKCC Rehab - 4th Installment
It's been a couple weeks since I've left my new friends at Dr Stubblefield's Cancer Rehab Center. I was able to speak with Dr Stubblefield on the morning prior to leaving NYC. He talked to me about the MRIs I had earlier in the week. The total spine MRI showed no additional cancer or tumor activity. I do have moderate to severe stenosis at L2-L3 and severe stenosis at L3-L4. This is what affects my lower legs/feet/toes with weakness, pain and numbness/tingling. The MRI of my Brachial Plexus did not show any additional cancer or tumor activity. It did show that the bottom 3rd portion (nerves leading to the hand/fingers) has been severely burned/damaged by radiation. The middle portion (nerves leading to the forearm/wrist) have also been severely burned/damaged by radiation. The upper portion (nerves leading to the shoulder/upper arm) has been burned/damaged, but not severely. From the elbow to fingers will continue to get worse with pain, numbness, tingling, and muscle atrophy. Eventually becoming nothing more than a dangling appendage. Time frame is an unknown factor. The upper arm, should potentially remain stronger, allowing movement to some degree. It's not the best of news, but at least confirms all that has been occurring over the years, and more so over the past 12 months. Dr Stubblefield told me that my Brachial Plexus radiation damage was the worst he has yet to see... Overall radiation fibrosis throughout the neck and chest areas was also abundant. He said that my individual case shows just how radiation treatments can damage. In particular, the Hodgkins mantle treatments of the 80's, followed by Breast Cancer overlapping radiation. He said that he is going to change his presentation and related MRI slides at his upcoming conference to use my case, because it clearly shows the long term affects of the damage caused by the radiation. He told me that i am an incredibly strong woman, for he understands the results on every day life of this type of damage. He said to be able to do as much as I force myself to do is amazing in itself. This somewhat embarrassed me, and at the same time gave me more strength. I have always done what I have to do to endure and hang onto quality of life. The same as we all do. It's never ever been easy as all of you who have had these same symptoms well know. It felt good because finally, a medical professional who actually knows what the hell has happened, and understands what the hell we actually have, and doesn't look at me with that "deer in the headlights I don't know what to tell you" look. He also reached out to my oncologist here in TX to discuss. She in turn told him she will discuss with her radiology partners. Going forward, the more they understand the long term effects of overlapping radiation fields for patients with prior mantle radiation, the more consideration they can give to the individualized treatment plan. And the more they can give to the patient for combined Dr/patient decisions on their treatment plan. I was at my oncologist this week for my 5th year "cancer-versary" from end of treatments. November 17th is my 6th year from diagnosis mark. We talked specifically about the findings of my MSKCC visit, and her discussion with Dr Stubblefield. She was grateful for his call and indicated the new information was beneficial for her and the radiologist for treatments on patients with prior Hodgkins radiation. YAY!! Finally, recognition from the oncologist world! That alone is a huge leap in the right direction.
By the way, my overall visit with the oncologist was good! No obvious signs of recurrence.... A little lab work, and I was dismissed for 1 year! That's a HUGE step!
Now, I continue with the PT/OT plan established by the MSKCC Rehab group. I still have, and will continue to have, the intense nerve pain, and constant paresthesia 24/7.... That does not go away, or get better - no magic pill or treatment. I totally get the severity of my condition, and know it can't be fixed.
The entire journey to MSKCC was well worth the time, cost, EMG pain, and exhaustion endured. The last day there, I hugged Dr Stubblefield, and cried. Same thing with the PT/OT staff.
My anticipated results were - and the RESULTS
1. A clear understanding of what damage has occurred - CHECK
2. What to expect going forward. - CHECK
3. An actual plan of action - CHECK.
4. Physical therapy to help with range of motion. - CHECK
5. Occupational Therapy to help with day to day life adjustments beyond what I've taught myself. - CHECK
6. Pain/paresthesia relief. - UNFORTUNATELY NO
7. A better outlook on quality of life. - CHECK
Overall, SUCCESS!
Stay Strong,
Cindy1 -
Cincerely,
A lot of sucess there, so happy the trip was worth it, but, wish #6 there had said check
0 -
Cindy, I agree with kmmd on that #6. There is a single line in one of the medical textbooks about this type of neuropathy: This type of neuropathy is devastating. That doesn't even BEGIN to describe it.... young stuents reading this type of statement have NO IDEA what it means in reality. I hope your docs can get this addressed by using your case in his presentations.
And we will rejoice that you had such successes, and are there for you on those days when you feel a little lower, but mostly hoping you can take each day as it comes, pain included, find some little bit of joy in other things. What are you able to do that you really enjoy?
I have a friend who is an artist and had to have shoulder surgery on her dominant arm, she was so fearful of losing function, but then decided to try painting left-handed. The work she did with her left hand was absolutely amazing!!! Completely different than her usual work, certainly not "photographic reality" but some really beautiful work from the heart. The point of this is, what can we do to help each other develop something that gives us inner peace and jooy with each day, despite our neuropathy?
Blessings to you all,
Linda
0 -
Wanted to share some YouTube video posted by Memorial Sloan Kettering Cancer Center, featuring Dr Michael Stubblefield. He is describing Radiation Induced Fibrosis, and Radiation Induced Brachial Plexopathy issues for Hodgkins Disease, Head & Neck Cancers, Breast Cancers, and Sarcoma survivors. Very well done - you'll find these to be easy to understand. Dr Stubblefield is who I went to specifically see in NYC at MSKCC in August 2011. My previous installments in this forum were focused on that 2 week visit with him and his PT/OT staff. This is good stuff!
 http://www.youtube.com/watch?v=xumJojH94Ts&feature=youtube_gdata_player
http://www.youtube.com/watch?v=xumJojH94Ts&feature=youtube_gdata_player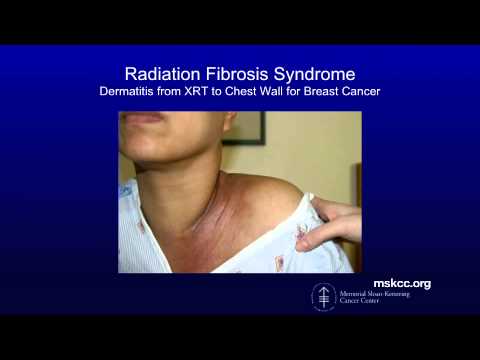 http://www.youtube.com/watch?v=LvZJKNtNXXc&feature=youtube_gdata_player
http://www.youtube.com/watch?v=LvZJKNtNXXc&feature=youtube_gdata_player http://www.youtube.com/watch?v=cp5PGCUYRdE&feature=youtube_gdata_player
http://www.youtube.com/watch?v=cp5PGCUYRdE&feature=youtube_gdata_player http://www.youtube.com/watch?v=dczzQxAaLYQ&feature=youtube_gdata_player
http://www.youtube.com/watch?v=dczzQxAaLYQ&feature=youtube_gdata_player
Stay Strong,
Cindy0 -
Cindy, thanks for the links! I am going to use them for my class in Pain Management for pharmacy students. These young health professions students are amazingly tuned in to the effect of pain on a patient's life and I am so privileged to help them learn about pain and the options for managing it.
0 -
Another one of those days when I am just so sick of putting up with the pain from the neuropathy and wonder what it must be like to get up in the morning and not deal with it. I can't even remember anymore
0 -
kmmd, I felt the same way today. Am tired of taking meds to treat SEs of meds to treat SEs of first meds. I am going to take a refresher meditation and qi gong movement class this week to try to readjust my attitude. Gentle hugsfor you tonight. You are loved.
0 -
Just a flying visit. As always, the support here helps. Its a day where walking is so hard,..
0 -
Nancy, the refresher class was helpful in that after the hour, I felt very relaxed and encouraged. I was able to do all the movements without pain as they were very gentle, and the instructor checked with me several times to see if I needed an alternate - she asked each person as they entered if they had any medical issues that would impact their ability to move in certain ways. The meditation was great to help my mind focus on just me. We were asked to dedicate our hour to someone, and they said ourselves were fine, so I dedicated my practice to myself. And I was very grateful for that when we finished.
I have been intermittently practicing meditation, and when I do it regularly, I feel better. When I don't, I get back to being overwhelmed by the busyness of life. I enjoy the moving meditations, like yoga and tai chi, because I feel like I am helping my body to recover along with keeping my mind healthy as well. So bottom line, I can recommend this type of class, and just wish they were available in a more convenient time and place.
Tai chi is really good for peripheral neuropathy with balance issues as it is really focused on balance, slow and purposeful movements. I had started going to this class twice a week before surgery in October, and hope to get back to it in the next few weeks. I am still dealing with post-op issues, but am doing better.
Kate, yes, there is support here. Keep breathing, my friend. Some days are just difficult, so come here and you will find love and understanding. People who have not had this experience just cannot have the understanding that we have for each other, and I was certainly one of those who had compassion but not understanding BN (before neuropathy). Sending you a couple of hugs and smiles.
Cindy, thinking of you tonight, hoping you are doing well. Kittydog, hope you are finally getting some relief from the hot summer weather!
0 -
Nancy, at least meditation won't hurt you! And it MIGHT help... good luck on finding a class. And if you do yoga, be sure to talk to the instructor before class to let him/her know about the neuropathy and any other problems you have. I have taken several classes and have found some instructors are very good at modifying movements, etc, but they have to know about it before they can make good suggestions.
0 -
I have a question for those of you who have neuropathy from chemo - did you have fatigue with chemo? And did it last a long time? I have been unable to be up all day every day for a year and a half, talked with my MO last week, and she said prolonged fatigue can occur with chemo. I know that chemo can affect both motor and sensory nerves, and I am beginning to wonder if it affects some nerves of the rest of our organ systems.... and muscles.... just wondering if there is some connection and have not yet found any research on it. I DID find that the prolonged fatigue has some research behind it, and it is now recognized by oncs, but no mechanisms or connection with other SEs.
0 -
Linda, yes fatigue and weakness. I've gotten some strength back but I'm not where I was. Fatigue has improved but, I still need more sleep, more rest time during the day than I used to. When I'm tired it is pure exhaustion and I can't function.
0 -
My mother has the same problem in her feet after taxotere treatment 4 years ago. The docs keep telling her it is temporary, so apparently it is her imagination making it chronic?
Right now I have it in my fingers, but I am only a few weeks out from chemo, so there is still hope that it may go away.
My mother says that getting enough rest and generally taking good care of herself helps cut back on how pronounced the neuropathy is.
I am also thinking that you may want to look for a PT who knows about this problem. They may be able to help somehow. I had some nerve damage after an epidural and it lasted for about 15 years, but did eventually go almost completely away and I found some kind of exercises for reactiviating the nerves that seemed to help a bit.
0 -
I have been prescibed Provigil for the post chemo fatigue. I have only been taking it two weeks, but I do think it helps.
Has anyone tried Qutenza for neuropathy. It is a high strength patch of capsacian that is applied at a doctor's office?
0 -
momine: personally, I think after a certain amount of years it is easier to have people quit denying what you're feeling and just help you deal with it. Chronic pain can become centralized, but that doesn't mean it is "in your head" or your imagination, it just means your nervous system is dealing with it in a different way than it used to and therefore the treatment needs to be different
rcca, I didn't have much luck with topical agents, my physician treating my neuropathy symptoms thought that was because the nerve damage was too much to benefit from application of something on the nerves. I'll have to check out provigil, good to know
edited to add: momine, I'm still chuckling over your description of that temporary 4 years
0 -
Momine, I commented about your neuropathy on the mastectomy thread I think, then remembered you had posted here as well. I forgot your mother had problems with taxotere also.
I am now working with my neurologist to taper off and discontinue the Effexor for the neuropathy. Even the lowest dose is giving me some major issues that I am just tired of dealing with. It's pretty discouraging, but I am hoping that maybe after 9 months on it I will be able to just use the topical stuff for my fingers and hope the teeth don't become sensitive again. *sigh*
kmmd, what topicals have you tried? I am using a compounded cream that was being used in a research study; my doc had to get pre-approval from the insurance company for them to cover it - they initially said they would cover 2 of the ingredients but not the third - my doc said it wasn't really something you could pick & choose which drug to leave out! lol! Anyway, they did approve it, and it has definitely given me some relief. It has ketamine, baclofen, and amitryptiline in lipoderm base and I can give you more info if you need it.
rcca, my MO offered something like the Provigil, but said it wouldn't be the best option because of other health issues that I have and she thought I might be at higher risk for adverse effects. Another *sigh*. I am beginning to think the fatigue may be related to the combination of meds I am taking either in addition to or instead of the chemo. I know I have not felt well nor had energy since I started chemo in Oct. 2011, the tamoxifen seemed to make it worse, and the other drugs all have listed "fatigue" as a SE in their labels. I would just like to ditch everything I am on, but still need the pain pills once a day and don't sleep without ambien. ANOTHER *SIGH*
Nancy, I will be starting another meditation class tomorrow. The one-day refresher on mindfulness-based stress reduction and the class in aromatherapy were good, but I need a weekly class to keep me on track right now. I know that if I take 5-20 minutes to just "be" or meditate each day, things go much better, but I get out of the habit if I am not going to a class where I will be embarassed to admit that I haven't practiced the previous week. The class I am going to start includes a variety of meditation types and about a half hour of qi-qong, which is VERY good with gentle movement. I would like to get to yoga in the next couple of months, but needed to start easier to get my body moving through the pain a bit.
Cindy, I think of you often, hope you are having some moments of joy today. Thank you again for sharing your story and the information that is so helpful. I dedicate my meditation practice tonight to you.
0 -
Linda-n3ypb, is there a name for the cream that you just described? Or do you have information on how much of each ingredient?
I'm 4 1/2 years out from chemo and still have my "temporary" neuropathy issues. My oncologist hasn't been helpful with this and I'm going to take it up with my pcp. Any information is appreciated. Thanks.
0 -
I finished AC/followed by Taxol, Aug. 30th - Thank goodness my fingers are no longer numb. I enjoy writing and had a terrible time the first two months. My toes are still bothering me a lot - especially in the a.m. I find that if I keep my feet very warm, the numbness is not as bad - or at least not as annoying. (For example, I put my heavy wool socks and heavy winter boots on to take my grandchildren to the bus stop this a.m. at 8:15 - I still have them on in my house as my toes are not bothering me right now - I have wood floors, so not worried about the boots in the house - would not care even if I had carpet - tired of the numbness -
0 -
Correction on my last post: I started chemo in Oct. 2010, NOT 2011, so it has been over a year since I felt good.
River_Rat, the study done by D. Barton et al. is published here:
http://www.ncbi.nlm.nih.gov/pubmed/20496177
It has information on the compounded cream, which is baclofen/amitriptyline/ketamine gel. My doc had to contact Dr. Barton to get the exact amounts to compound, and it expires every 2 weeks, so I have to get it refilled often. I ended up seeing a medical toxicologist who was willing to work with me because this is actually a "toxicity" problem, and she was quite knowledgeable about nerve damage from a wide range of toxic agents, and was able to explain how each of the ingredients in this compoud work together synergistically. I also saw a neurologist, but she mostly works with diabetic neuropathy and the mechanism of injury to the nerves is different, so the drugs she uses for the diabetics don't work the same for the chemo-induced neuropathy.
I saw my cardiologist today, who kind of opened the door, asking how I did with chemo, and so I told him. He commented that it seemed reasonable that I was angry because it seemed like the MO just didn't take me seriously when I complained after the first dose, and then went ahead and gave me the same drug again and yet a 3rd time. He was very sympathetic, very kind, and I felt very validated. He also said my heart is doing fine. Yayyy!!! At least ONE thing is doing OK!
0 -
I have neuropathy in my hands and feet from chemo. I ended chemo in November 2010. I am on a month break from Anastrozole and the severely increased hand pain has eased but not not fully stopped. I see my MO tomorrow and I think I will be back on arimidex.
My question is this: Is the neuropathy from Arimidex and anastrozole permanent like it is from ACx4 and Taxol x2 ?
I started getting neuropathy while on AC x4 then it increased so much on Taxol that the MedOnc stopped it. I actually had a book light inside my slipper and could not feel it at all. I was walking on it and had no idea it was even there, my husband saw the cord sticking out of my slipper and came over and began to pull it out. We were both amazed I couldn't feel it.
Thanks Ginger
0