Considerations: Lumpectomy w/Rads vs. UMX vs. BMX
Comments
-
I have a question re:
From page 3, bottom right column
"Currently, it is unclear why breast-conserving therapy with radiation would demonstrate an overall survival benefit. One of the theories proposed is that improved systemic therapy options are resulting in improved control of micrometastatic disease leading to decreased distant recurrence of breast cancer. Currently, it is unclear why breast-conserving therapy with radiation would demonstrate an overall survival benefit. One of the theories proposed is that "improved systemic therapy options are resulting in improved control of micrometastatic disease leading to decreased distant recurrence of breast cancer. Therefore, improved locoregional control provided by radiation therapy with tangential axillary exposure may contribute to a survival benefit by preventing secondary dissemination of the disease".9,10 Unfortunately, because the NCDB does not gather information on recurrence, this is only theoretical as it pertains to the current study.9,10 Unfortunately, because the NCDB does not gather information on recurrence, this is only theoretical as it pertains to the current study"
"Improved systemic therapy options". My question: To my understanding radiation is not systemic. Wouldn't chemo and/or the anti-hormonal meds be the only systemic therapy options? Many thanks for any clarification.
0 -
What the article is saying is basically that while it is not clear exactly why BCT offers slightly better OS than a MX, it might be because of the extra local control that radiation provides.
In other words: Cancer cells left behind after any surgery (lumpectomy or mastectomy) could still disseminate and cause metastatic disease later. We know that systemic treatment (chemo and/or hormone therapy) help to eliminate undetectable microscopic metastatic disease, but these drugs are certainly not 100% effective. That is why radiation might offer an additional layer of local control beyond surgery alone, possibly accounting for the greater effectiveness of BCT over an MX. At least that is the possible explanation.
I think this is really important information for early stage patients making a surgery decision. I hope BCO will consider including this new information on their pages soon also.
0 -
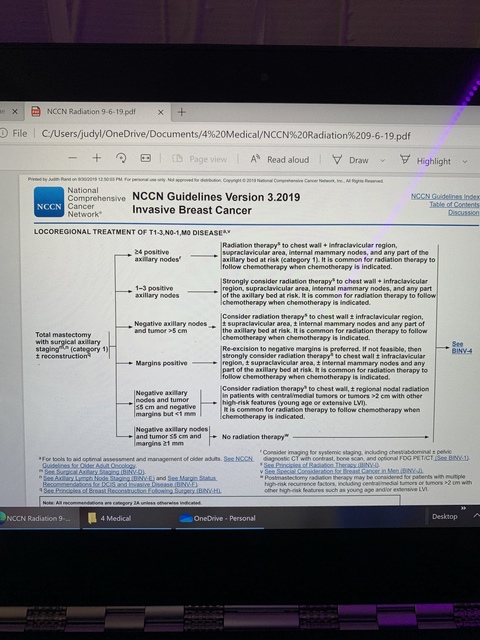
I didn’t see that in the article, but it is exactly what I was thinking. And per my more detailed thoughts above, the problem is that lumpectomy patients are getting radiation to the nodes and mastectomy patients are not. This makes no sense to me. Looks like the study is node negative. But of course there could always be a few cells lingering. Even node positive doesn’t always get radiation which is beyond ridiculous. Nccn recommends it be “considered”. I think that needs to change. It is not consistent.
 0
0 -
buttonsmachine and JRNJ, if you look at the other studies that I reference in my opening post, there are earlier studies that have reached the same conclusion. For example:
Survival Comparisons for Breast Conserving Surgery and Mastectomy Revisited: Community Experience and the Role of Radiation Therapy (June 2015) "We found no difference in overall survival by breast cancer surgery type when the effects of adjuvant radiation therapy and other covariates were eliminated using statistical methods. However, comparison of BCS plus radiation to mastectomy alone revealed a significant survival benefit with breast conserving therapy, suggesting that the prognostic differences reported here and by others may be related to use of adjuvant radiation therapy after BCS rather than to the extent of surgery itself. Given the limitations inherent in this type of study design, prospective confirmation of this finding is necessary."
0 -
Beesie, the sentence structure in your first point of consideration in the main post confused me. You said
However you should be aware that there is no guarantee that radiation may not be necessary even if you have a mastectomy,
Perhaps change it to
However, you should be aware that even if you have a mastectomy, radiation may be necessary...
Also, this question comes up in new posts so often, I've saved it as a favorite to make it easier to provide for them. Thanks.
0 -
Buttons, thank you for clarifying it for me.
0 -
Thank you Beesie
0 -
MountainMia, you mean you don't like my convoluted language? I specialize in it!
Change made, thank you!
 0
0 -
Looks good!
0 -
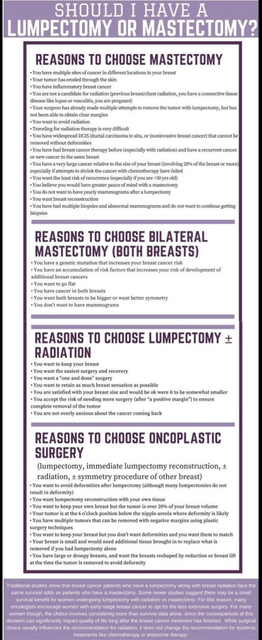
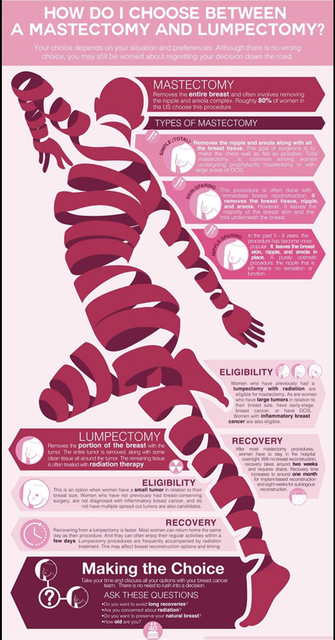
I thought I would add this link to one of my favourite websites on the topic of breast cancer surgery choice:
Lumpectomy vs Mastectomy: How to Choose http://www.melbournebreastcancersurgery.com.au/lum...Here are a couple of helpful graphics from the site, but for anyone struggling with this decision, I would suggest going to site itself - there is a lot of excellent information there to help with the surgery decision.
 0
0 -
Bessie - this information is exactly what I was looking for. Unbiased, thorough information. Thank you! ❤️
1 -
@dsc I think this may be the post you were looking for
0 -
Hi everyone, recent dx of IDC, Grade 2. I'm trying to decide whether to have lumpectomy or bilateral MX. For me, there will be many lifestyle advantages to going flat when I want—on hot humid days, and at the gym, staying cooler, and no sweating into a bra. No bouncing when jogging. Then when I want, I can wear falsies. I do recognize that it will be a long journey to get used to seeing myself without breasts. But I can do that.
I initially thought the medical advantage of MX would be I'd never risk BC again, no worries, no mammos, no sonos, etc. But at the first appt with breast surgeon, I learned that Post-Mastectomy Pain Syndrome lasting long after surgery has healed is not uncommon. I'm a wimp when it comes to pain!
I have to learn more about what radiation would be for me if I choose lumpectomy. My sister had 6 weeks, 5 days/week, but she was 49 years old. I've heard now it's only 5 days! Another factor is that I don't get sick leave. No work = no paycheck. So lumpectomy would have faster recovery. BUT I'd never get the lifestyle advantages of going flat, and I'd continue to have risk of new BC. If I get BC again, I'll regret not having MX. If I have significant Post-Mastectomy Pain Syndrome, I'll regret having MX.
My plan is to keep reading and talking to people, including doctors. I have an appt in two weeks with a plastic surgeon who will be part of the surgery to ensure I'm smooth with less scar tissue. I plan to make appts with my regular GYN and the breast surgeon I saw once. I wish the decision was easier! I went in 100% sure I wanted bilateral MX. I knew nothing—I actually thought I could go back on hormone replacement surgery to prevent the severe hot flashes and brain fog I had beginning at age 45.
0 -
Does anyone here know what is recently/ common for radiation treatment? How many days / weeks?
0 -
For people over the age of 50 with ER+/HER2- bc with no nodes involved the FAST radiation protocol is once a week for 5 weeks. The FAST Forward protocol is 5 consecutive days. If the hospital isn’t too far from your work you can ask to be scheduled early in the morning or late in the day so that you don’t miss too much time,
0 -
@k123456789 I just finished 16 days of radiation last week after having a lumpectomy and 5 nodes removed. I also had the choice of mastectomy or lumpectomy. My opinion was 1. You can still get breast cancer after mastectomy. 2. Recovery is harder from a mastectomy. 3. I can always have a mastectomy later if needed.
0