Birads 5 with calcification
Comments
-
That's really good news at this point. They will likely do a sentinel lymph node biopsy when they do your mastectomy to confirm that there's no involvement of the lymph nodes. With ER+, you are NOT considered triple negative. They will likely put you on an aromatase inhibitor or Tamoxifen to lessen the changes of the Cancer coming back after surgery/radiation. If you do not have lymph node involvement, I think that you will likely be classified as Stage 2 by the size of the tumor.
Regardless, I hope that you have a great weekend. You've got this! As I was told, you don't have to be a hero, you just need to show up. Let the experts take care of things for you.
0 -
@scaredme You're right. I completely forgot about that part. She did mention they would be testing some lymph nodes during the mastectomy. She also explained that even if the nodes turn out to be clear, a lumpectomy still wouldn’t be the best option for me because I have two sizable tumors that are spaced too far apart. So, in my case, a lumpectomy just wouldn't make sense. I told her, “Do whatever you need to do.”
I’ve seen how emotional and difficult these decisions can be for people. Thankfully, I’m not someone who gets too caught up in the physical aspects. No judgment at all to those who do ❤️ everyone’s experience is deeply personal and valid. For me, it’s more about doing what’s best for my health. I just want to live, watch my kids grow into adults, and meet my grandkids one day. Losing my hair or worrying about what my chest looks like under my shirt doesn’t bother me. Plus, chemo curls are always so beautiful to me, anyway!
Wow! I love that “you do not need to be a hero, you just need to show up”. Very motivational for this who are super emotional like me.
1 -
@lisat8228 I misread the previous biopsy results, so you are not considered triple negative. Hopefully, I did cause you any extra worry.
0 -
What good news, Lisa, to sleep on at the start of a weekend! As your wonderfully knowledgeable BC sisters have already told you, MRI evaluation of the chest wall anatomy is a valuable tool and step in the process. Glad it's now behind you.
I've been thinking about you and checking your updates this week. With your advanced grasp of BC terminology, it's difficult to believe you're still only a newbie... although learning very quickly! All those layers of soft & fibro-glandular tissues with fat, vessels & lymphatics, the pectoralis major & minor muscle area is a complicated area of anatomy to understand. But you're plowing thru it.
I remember from when a friend had her double mastectomy with a careful thorough scraping of her chest wall during surgery. She also had been given radiation to the area following her BMX, and 10+ years later she's still doing fine. She got 3-4 alternate opinions from different BC surgeons with solid experience, I recall. Her (3) grade-3 tumors had been very deep adjacent to her chest wall with minor infiltration, but today she has very little recall. That's what we all wish for and some day you'll hopefully put this all behind you. But for now, you need to continue focusing on each & every little baby step, only one at a time. It's a lot, but you're super smart & insightful, stronger than you think, so you'll get thru it with all your gals' great support here.
I found my double mastectomy to be much less painful & less cumbersome than my first surgery (lumpectomy) and I was busty too. I didn't mind the 4 drains either. I've been fine being flat for years, especially during the hot summer. (I now think good riddance.) Glad you're catching a break for your summer weekend. Hugs 💜💚
0 -
@illimae You're totally fine 😊 I wasn’t panicked at all. I also forgot to mention something my oncologist told me that I want to share with you all. She said there’s been a noticeable rise in colon cancer among younger people, and it's really concerning. She’s not sure what’s causing it, but she’s treated 8 patients in their 30s for colon cancer in just the past 6 months and that’s just in Tuscaloosa, which is a small city. She’s encouraging everyone to help raise awareness about this trend.
I have a family history of colon cancer on my mom’s side, my grandmother and uncle passed away from it, and a great aunt survived it. I won’t be getting a colonoscopy this year since I’ll be having a PET scan, but I definitely plan to talk to my doctor about future screenings. Even though my relatives were diagnosed between the ages of 50 and 70, with the rise in cases among younger people, I think I’d be considered high risk at 33. It’s always something, isn’t it? 🤦🏽♀️
0 -
@obsolete Your comment truly made my day! I’d be lying if I said all this knowledge came from me researching anything. Honestly, I can’t even remember the last time I googled anything about breast cancer. Everything I know has come from you all… this group of brave, encouraging, beautiful women. From the moment I joined, you’ve all guided me through each appointment, prepared me for what to expect, and offered more support than even some of my own family.
You’ve explained things so clearly, shared invaluable advice, and provided the kind of encouragement I didn’t know I needed. I can’t put into words how grateful I am. As someone who’s always felt like the black sheep, it’s incredibly healing to feel so supported by people I’ve never even met in person. Having people who believe in you, even more than you believe in yourself, feels like it’s mending a part of me I didn’t realize was broken (my inner child). Thank you all, from the bottom of my heart.
Note: I don’t think I’ll mind being flat either. I was never really attached to having breast. honestly, that’s why I had a reduction 13 years ago. When the oncologist explained that I might need a mastectomy instead of a lumpectomy, she sounded so apologetic. But I told her I’m not bothered by it “take them off”. I’m not even sure I’ll go through with reconstruction, unless the scars become traumatic or emotionally difficult for me to handle.
0 -
I decided to review my MRI report, and I’m honestly in shock. The initial mammogram and ultrasound-guided biopsy measured my tumor at 3.4 x 2.4 x 3.5 cm. But just two weeks later, the MRI shows a larger size: 3.4 x 2.2 x 7.3 cm. This sudden increase, especially the doubling in length, is making my anxiety spiral. How accurate is this measurement? And why would the length change so drastically?
I have 2 appointments tomorrow. An ultrasound on my lymph nodes and another appointment with my oncologist.0 -
It didn't necessarily grow in size: the measurements from imaging and biopsy are approximations. Accurate measurements are assessed only when directly visualizing the tumor, i.e., during surgery. This was explained to me after the radiologist who did my ultrasound said 7mm., the one who did the biopsy 2 weeks later said 9mm, and the surgeon & pathologist said 1.3cm 2 weeks after that. Hope this assuages some of your concerns!
0 -
Imaging can be variable for a number of reasons. My tumor didn’t show at all on mammograms, was 1.6 cm on ultrasound at the local hospital, 2.8 cm on ultrasound at the big hospital with newer machines and 3.2 cm post surgery. My breast surgeon told me it felt like it was a bit over 3 cm so her estimation was closest to the actual size. MRIs are often more accurate for dense breast tissue but can also have more false positives. Sometimes it is difficult to distinguish IDC from DCIS on MRIs if the two are next to each other. It’s unlikely that your tumor size has changed in such a short time span. I would ask the oncologist to ask the radiologist their opinion on this. I hope your appointment tomorrow goes well.
0 -
My lymph node ultrasound appointment didn’t go as well as I’d hoped, at least not from my perspective. I saw areas light up red on the screen, and the tech took multiple measurements of some spots, especially above my collarbone near my neck, and also under my arms. I’ve been trying to stay positive, but it’s getting harder. Everything just seems to keep getting worse. I’m feeling overwhelmed,angry, sad, and disappointed all at once.
My legs still hurt, and I’m still short of breath. I just need something! anything! to finally go right. So far, it feels like nothing has. Even when I get what seems like good news, it’s quickly taken away by another test or scan.
I’m heading to my oncologist now. The radiology tech said the results likely won’t be ready until tomorrow, so I won’t get any clarity today. Still, I’m hoping I can at least leave this appointment with a start date for treatment.
0 -
@lisat8228 I’m sorry you’re going through more tough times, especially after a decent oncologist appointment last week. Cancer is definitely ups and downs. I just want to add that while we can’t help but try to assess the situation during scans, we are not techs. I’ve sent myself into worst case scenarios several times and have been so wrong. Waiting for official answers is hard but it really is best.
0 -
@illimae thanks so much. hopefully the pet scan is good news 🤞🏾
results of ultrasound:
no enlarged adenopathy is seen in the left sternal, infra, or supraclavicular regions.In the left axilla, 2 lymph nodes are present with the largest in the axillary tail measuring 2.6cm x 1.0cm x 1.1cm
Does this mean cancer has spread to 2 of them?
0 -
@lisat8228 No, it does not mean cancer. Lymph nodes can be enlarged for a number of reasons, like an infection, it’s their job. Only a biopsy can prove what’s going on for sure. Did they do or schedule a biopsy for that or a CT or PET scan yet?
1 -
@illimae My oncologist said he was planning to place the orders for the PET scan and port today, but since my appointment ran late and I was there until closing, I should expect a call in the morning with the scheduled date. He prefers to wait for the PET scan results before starting treatment. However, he mentioned that if the lymph nodes looked good on the ultrasound, we could move forward sooner, but it looks like that won’t be the case now.
I also looked up the location of the axillary tail. it’s in the upper outer quadrant, right next to where my tumor is. This lump appeared after my biopsy, and I assumed it was a hematoma or swelling, but it never went away. I’m starting to wonder if this is what the MRI picked up on, and if that’s why the tumor size seemed to change so drastically from the ultrasound. Could the MRI have measured both the tail lymph node and the tumor together, since they’re so close? Who knows? All of these different scans are running me crazy. Lol!0 -
Hi @lisat8228, Imaging helps with planning treatment but can’t provide an accurate diagnosis. Presurgery my lymph nodes looked fine on US but one was positive by pathology. After surgery I had anther lymph node become visibly enlarged. When it remained that way for six months it was biopsied and found to be negative. It eventually returned to normal size. Path found my tumor was surrounded by numerous radial scars, benign fibrotic growths. That explained why the tumor didn’t show up on mammograms. Reasons for imaging results sometimes get explained later.
You need the PET scan before they can proceed with treatment since the results of that could affect it. Hopefully it will be scheduled soon so treatment can begin. You were right when you said that starting treatment would make you feel better; at that point you are doing something to inactivate the cancer. The term scanxiety was coined for a good reason.
0 -
I am sorry to hear that they are now concerned about your lymph nodes. Unfortunately, the only way they can give you a 100% definitive answer is though pathology when they take them out.. It is such a rollercoaster ride, I know.
That said, I had 8 cancerous lymph nodes and no spread 5 years ago and am still here (knock on wood). As my Oncologist said to me in the beginning, this is scary for us, but very routine for them. Just keep showing up. Hugs.
0 -
Hi, one more step in the long learning process to keep you on your toes. You're doing well putting one foot in front of the other. Your upcoming scan will be looking for any possible increased metabolic activity.
As your other sisters commented, there are multiple possibilities. I had a benign shotty lymph node similar in size, and surgery also found a larger cluster consisting of two enlarged benign shotty lymph nodes clumped together.
Keep hanging in there, sister! 💚💜
0 -
0
-
Thank you all so much! I really love that phrase, “just keep showing up.” This journey definitely feels like a roller coaster. I’ve been meaning to come back and post sooner, but depression got the best of me for a while. These past couple of days have been especially tough. I went down a bit of a rabbit hole researching PET scans. Found that they’re incredibly detailed and expensive which is why doctors usually don’t order them unless they’re genuinely concerned about something. And they’re so sensitive that they can sometimes pick up things that turn out to be false positives, leading to more tests, more waiting, and more delays.
In my case, the doctor ordered one because, to his defense, my situation is a bit more “complicated”. the cancer is just starting to touch the pectoral muscle. His decision to hold off on treatment until the PET scan results are in makes me think he may be just as concerned about possible metastasis as I am.
I did get the call from scheduling that my PET scan is scheduled for next week. I also have my appointment set with the larger hospital where I’ll be transferring my care; that’s on August 5th.
Thank you again for being here for me. It means a lot.
1 -
Thanks for the update.. Just one thing to throw out there once again.. These scans are not 100%, so don't freak if they uncover something (easier said than done, I know) It is also standard practice to order these type of body scans when they suspect lymph node involvement to rule out mets. It does not mean that your Oncologist thinks you have them.
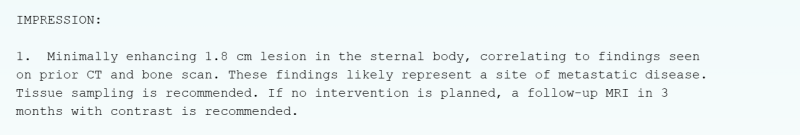
I had a terrible scare last summer with an incidental finding on a bone scan when I was experiencing hip pain. The scan found nothing wrong with my hip, but discovered an unexpected lesion on my sternum. In the next 6 weeks, my Oncologist ordered a Cat Scan, an MRI and eventually a bone biopsy. The process was awful.. I literally had to alternate between Lorazapm and Pot gummies to stay sane (and I am normally a substance free gal) . Here was the radiologist's report..
It was 2.5 weeks later when I finally got the results of my bone biopsy.. completely benign. Apparently it was a result of a fall I had a few years ago. I am now terrified of any imagery and hope I don't have a need to do any more. Too high of a chance for false and incidental findings.
0 -
I have a similar story, scaredme—and it predated my bc diagnosis. In 2004 when I was 53, shortly after returning from a flight on which I caught a cold, I woke up one morning and found that music on TV—commercials, themes, etc.—sounded tinny, sour and completely off-key. Vocals and instrumentals sounded like they were in different keys, in the same song! My best Martin guitar sounded like a cheap solidbody electric that wasn't plugged in. And stuff sounded a quarter-step flatter in my L ear than my R. That weekend I had 2 gigs (plugged in, and miked so I could hear myself sing and ignore the fact that the guitar sounded off) and a large-group recording session for the anniversary of "Give Peace a Chance" (I was assigned to play dulcimer and be part of a 12-member harmony choir of Chicago folkies and rockers). I managed to get through it, gritting my teeth all the way, and a week later I was part of a folk festival—my workshop set was miked so it was tolerable, but the sound of acoustic instruments jamming all over the festival grounds was like fingernails on a blackboard, so I went home early. Now, a few weeks earlier, my right hip began "snapping" painfully—the only thing that relieved it was swinging that leg in an arc as I held on to things like I was a dancer at the barre. At that folk festival, I was forced to use a cane to walk because of the pain.
Went to an ENT for the hearing problem—he said "must be something with your cochlea" (ya think?) and told me to hydrate and take Sudafed to decongest my middle & inner ear. I went online to a female musician listserv to which I subscribed and described the problem—and received a flood of "me too!" responses (unlike what the young ENT said). One musical colleague from Seattle gave me the name of a local neurotologist who successfully treated her "sudden sensorineural hearing loss" and even offered to put me up should I decide to fly out. Because of the congestion, though, flying was out of the question. The neurotologist gave me the name of his colleague in Chicago—but when I called for an appointment I was told he had passed away a week earlier, and I was referred to another neurotologist in the suburbs. I went to him, he gave me a standard hearing test, declared there was nothing wrong, saying "you're a musician, you're just too picky about pitch." He concluded I had atypical Meniere's syndrome (a diagnosis made when everything else has been excluded), put me on a restrictive diet and ordered a brain MRI, which I had the day after I saw my orthopedist for the hip problem.
Meanwhile, back at the orthopedist (who had a room full of residents and fellows), I described the symptom and how I relieved it, and he ordered an X-ray. When the films came back (they still used film), he gasped and said "What the f***?" (not something you want to hear from your doctor). There on the film, the tip of that side of my hip had broken off and there was a chip floating free. At 53 I was too young for osteoporosis. So he ordered a PET scan.
I spent that weekend awaiting the results of both the brain MRI & PET scan. (I'd asked the ENT "are you considering bone mets from a brain tumor, or brain mets from bone cancer?" and he replied "Yes." Also not what you want to hear from your doctor). I spent that weekend frantically Googling "bone cancer" and "brain tumors affecting hearing," and the prognosis for either was not encouraging. I began looking at obituaries of people at least 5 years older than me and began to resent that I might not live that long.
Come Monday morning, the MRI results came back negative for any brain abnormalities. I went to the orthopedist, and he showed me the scan that he concluded showed only inflammation, no lesions. He then asked, "Say, didn't my former partner harvest bone from your hip in 1996 in order to put your broken leg (from having been hit by a car) back together? Looks like he dug a bit too deep, but better to over-harvest than not take enough." Thus, the two swords of Damocles were retracted back up into the ether. (A course of antioxidants & steroids cleared up the hearing disturbance, and the bone chip was resorbed by my body so the ligament stopped getting hung up on the jagged edge of the iliac crest).
So 11 years later when I was diagnosed with IDC, I was a bit more prepared (though still pretty scared).
1 -
@scaredme
Your story really resonated with me. I can only imagine the stress of going through all those tests and the awful waiting game that followed. I’d probably need a similar stash of calming aids to get through something like that too. It’s so frustrating how “routine scans” can spiral into full-blown panic especially when the findings end up being totally unrelated, like an old injury.@chisandy
Wow, what a powerful and intense story you had me captivated the whole way through. It's incredible how interconnected everything in our bodies is, and how often we end up having to advocate for ourselves when doctors can’t quite piece things together. That ENT telling you you're "too picky about pitch" has to be the most musician-specific brush off I’ve ever heard. 😂As for me, I honestly don’t know what scares me more right now, the PET scan picking up something benign that causes a delay in treatment, or it actually finding metastasis. My leg pain is getting worse. What used to come and go, mainly at night, is now a constant, all day issue. It’s not excruciating, but it’s definitely uncomfortable. More of a dull, biting or burning sensation that’s hard to ignore.
What really worries me is that it’s both legs, and the pain started in both at exactly the same time and has progressed equally on both sides. I’ve combed through tons of posts on the discussion boards about leg pain and bone mets, but nothing has really helped me make sense of what I’m feeling.
I’m only 33. While my knees haven’t always been the greatest, I’ve never experienced anything like this before, and I can’t shake the fear that this could be cancer in my bones. My platelet count was slightly elevated during pre admission on Friday. I’m not sure what that means. I’m getting my port placed on Monday, and while I’m trying to stay grounded, it’s hard not to spiral.
0 -
Quick update: The port placement surgery went really well this morning. My neck is sore, but otherwise I’m feeling okay. They also did a chest X-ray, and the report showed no abnormalities. Both the MRI and X-ray came back clear for the lungs. Now I’m praying the PET scan brings good news too. I’m finally seeing some light in this tunnel. Thank you so much ladies for being here with me throughout this.
3 -
@Lisat8228. We are happy to hear that your surgery went well this morning. We will be keeping you in our thoughts as well for your scans.
The Mods.
1 -
I'm glad that the port placement went well. I'm assuming that they are planning on chemo first since they put it in so soon? I'm curious what type they plan to give you.. Mine was the AC-T Dose Dense regimen, but they did it after my surgery.
Fingers crossed for you that the Pet Scan comes out clean and it is scheduled soon. Can you believe that they did not do mine until right before they started chemo (after 2 surgeries)? My mind hadn't gotten to the "What if it is metastatic?" until the Oncologist mentioned ordering the scan, Thank God.
0 -
@scaredme I have to start with chemo and radiation before surgery because the ultrasound and biopsy showed potential involvement with the chest wall. Initially, they weren’t sure how deep it went, but the MRI later showed that it’s only pressing against the pectoral muscle, not actually invading it. Still, to avoid the risk of losing any of that muscle during surgery, they decided the best course is to do chemo and radiation first.
I’m honestly a bit embarrassed to admit that I don’t fully remember my chemo plan. I completely blanked out during my last visit with the oncologist. What I do remember is that he was very upfront and told me he wouldn’t be going easy on me. He mentioned something about “the red devil,” 13 rounds, and that the regimen he’s giving me is much stronger than what he’d give someone older. He said it’s more aggressive because I’m “young” and can handle it.
Also… I kind of wish he hadn’t brought up the PET scan so soon. Is it silly that I don’t want to know right now if it’s spread? I just want to hold on to a little peace of mind, even if it’s temporary. It feels like too much to go from being diagnosed with cancer to possibly hearing it’s already stage 4, all in a matter of months. What we go through is so overwhelming. I just want a little peace. Just a little.
0 -
It sounds like you will be receiving the same chemo regimen I did. With the anti-nausea meds, I did fine with it.. never even vomited though it make me feel very odd for about a week after each treatment. The AC stands for Adriamycin and Cytoxin.. The Adriamycin is what is known as the "red devil". After this, they follow with Taxol which I found to be much easier. In my case, I had infusions every 2 weeks: 4 A-C, then 4 Taxol for a total of 8 rounds or total 16 weeks of treatment. Sometimes they do the Taxol in lower doses every week for 12 rounds, which sounds like what they are planning for you. Below is a link that talks more about AC-T chemo
Your Oncologist will very likely give you an injection after each chemo to boost your white blood counts (Neulasta).. Worked really well for me and my white counts were ridiculously high so I stopped even needing them when receiving Taxol.. There is also a version that will do the injection automatically so that you don't have to go back the next day for it.. Neulasta Onpro!
I know it all sounds really overwhelming. I remember crying when we went to pick up all of the prescribed meds, but if you take the steriods as prescribed and stay on top of the anti-nausea meds, you will be ok. Cancer treatment is not like they portray in the movies. That part really surprised me. In a way, it felt good to know that I was doing something active to combat the Cancer.
I think I've given you enough to think about, but can answer any specific questions you may have about treatment as you get closer.
One more note.. My Oncologist said exactly the same thing about me being young and able to handle it and I was 48!!! Had to laugh at that!
0 -
Glad to hear you got your port paced for pre surgery chemo. I didn’t do chemo since my Oncotype was borderline (not much benefit from chemo.) My tumor was central extending into the deep layer of superficial fascia (learned that this is the second of three layers of fascia) but it was removed without harming the pectorals. They had MRI and a pathologist with a microscope in the OR to check that they got all the cancer without cutting into muscle. I didn’t learn about this until after surgery so I never had a chance to worry about it. Having chemo and rads first to shrink/eliminate the tumor sounds like a safer way to preserve the muscle.
Chemo doesn’t sound like fun but everyone makes it through with the help of meds; it’s worth it for a good outcome. The upcoming PET scan is a worry but most initial scans are clean. I hope yours is. It’s a relief when treatment starts because you finally feel like you are doing something positive. Hang in there.
0 -
@scaredme Thank you so much for sharing your experience. It’s comforting to know that the treatment was manageable for you and that you found strength in taking action. That really resonates with me.
My doctor actually said something very similar, that chemo isn’t like what you see in the movies, and that not everyone has a hard time with it. He mentioned that some people go through treatment with minimal or even no side effects, and I’m definitely hoping I’ll be one of the lucky ones. But even if I’m not, I know I’ll get through it.
As long as my PET scan looks good, I’m ready to give this fight my all. I’m feeling surprisingly steady about starting treatment. I think having a plan in place helps a lot. My mom has really been my rock through all of this. She’s stepping in to help with the kids, cooking, and cleaning once things get going, and that gives me a lot of peace of mind.
Thanks again for your kindness and honesty. It helps more than you know. Im sure I’ll have a lot more questions as things move forward.
1 -
@maggie15 I truly wish my surgeon had moved forward with surgery after the MRI showed the tumor wasn’t deep. Knowing that yours was close to the fascia but successfully removed without involving the muscle gives me hope, but it also makes me question the delay on my end.
Honestly, I’m struggling with trust in my current team. The whole process has felt slow and disjointed, and it's hard not to feel like just another number. Even though my tumor is only rubbing against the surface, it’s still very uncomfortable and at times painful. The waiting and uncertainty just add to the stress.
I’ll be meeting with a new oncology team at UAB before returning to my current oncologist. They’ve already requested all my scans and reports, so I’m hoping there’s a chance they’ll start treatment there right away. I’m trying not to get my hopes up too much, but I’m desperate to feel like something is finally moving in the right direction.
Did your tumor ever cause you any pain before treatment started? I’m curious how common that is.
Thanks again for your kind words, it really helps.
0