Tamoxifen and fatty liver disease
Hi All- I was diagnosed with breast cancer two years ago and I've been on tamoxifen for about a year and a half now. I was just diagnosed with fatty liver disease after my blood tests indicated that I have elevated liver enzymes. My doctor says that tamoxifen cannot cause fatty liver disease but the research I'm doing says otherwise. I'm wondering if anyone else has experience with this.
Comments
-
Yes it happened to me too. Now, I haven't done tamoxifen in almost six months, and nothing else either, so I am really interested to see what my next liver imaging tests show. But I was under the impression that liver enzymes and a fatty liver were two separate things. I will have to check when I am on my own home computer, and not my nieces very slooooow ipad
0 -
tamoxifen does cause fatty liver in up to 50% users..your doctor is wrong..I got fatty liver from tamoxifen as well
0 -
my liver enzymes were elevated when I was on Tamoxifen, but I had fatty liver before that. Started Arimidex in Dec, waiting to see if liver enzymes improve during my next physical
0 -
I've been on tamoxifen for 5 years and my last CT about 3 months ago said that I have fatty liver. From what I read tamoxifen does give you fatty liver.
0 -
I do think tamoxifen can cause fatty liver, but my liver enzymes have actually gone down on tamoxifen from mid-normal range to low-normal. And I take twice as much tamoxifen as most women (40mg/day).
I believe the reason tamoxifen has not adversely affected my liver is because I am on a ketogenic diet (I have lost 150 lbs on it too). The desired effect of a very low carb diet is that my body has adapted to burning fat rather than glucose for energy. Fat doesn't accumulate in my liver because it all gets used.
Some doctors know a low carb diet can help a fatty liver, but a lot probably don't have a clue, so your doctor won't necessarily suggest it. Based on my own experience I think it's worth trying dietary changes before doing something more drastic like stopping tamoxifen. Especially if you can't make a clean switch to an AI without an oophorectomy or ovarian suppression, and you would rather not.
0 -
I was on T from 12/13 to 10/16, during that time, my liver enzymes started increasing, and in August of 16 i had a pre-surgical ct done, where my liver was shown to be very fatty. i'm fat, but was not as fat when I started all this mess. I think T increases your % body fat all over. I can't lose weight no matter what I do, and a lot of is stores in my abdomen. My MO had me go off the T for a few months, I tried arimidex, but it turns out i am not menopausal, and it almost crippled me with joint and bone pain. My liver numbers have decreased back to normal, though it is still fatty, and I am still having a very difficult time losing weight.
I am going back on it, with monthly liver tests to see what happens. Obviously we don't want to damage my liver further, but, my other option at this point is either ovarian suppression and another AI or ovarian removal and an AI, which also don't appeal to me.
Sucks that pre-menopausal women have little choice and they have not come up with anything in the last 40 years as an alternative to T
0 -
I had fatty liver before Tamox. I have a big belly, like 9 mo preggers.
 My liver function results are about the same. Obesity is the reason given in my case.0
My liver function results are about the same. Obesity is the reason given in my case.0 -
I was diagnosed with breast cancer in 2013 and have been on Tamoxifen since May 2013 to present. About 1 year ago they diagnosed me with a fatty liver and they told me the same thing. What should we do?
0 -
was diagnosed with breast cancer in 2015 been on tamoxifen for a year and three months, never had a problem with fatty liver disease was diagnosed with it in Oct 2017. I haven't been told from a doctor that tamoxifen caused fatty liver but I'm beginning to think that it does. We all have one thing in common and that is, TAMOXIFEN! Gremillion1 I wish we could all get together and get some answers.I wonder have a study been done concerning the possibility that TAMOXIFEN cause fatty liver?
0 -
Hi everyone
I don't think developing fatty liver while on Tamoxifen is all that unusual. The question is does actually cause any damage/symptoms and does it resolve after Tamoxifen is discontinued?
A bit of light reading:
LiverTox-Drug Induced Liver Injury
0 -
Hi! I was diagnosed with BC in Jan/18, then surgery, radiation. Tamoxifen for 4 1/2 months. I had a history of mild fatty liver but enzymes were normal before surgery. On August 9th I woke up with ascites (fluid in the peritoneal cavity) and jaundice. I went to hospital and they drained 2 litres from my belly and kept me for extensive testing. Tests revealed I had a hepatotoxic response to the Tamoxifen and now have end stage decompensated liver failure. I need a transplant and will receive a live liver donation from my son when I get sicker but they want me to be cancer free for 5 years. If my liver really goes bad and I am near complete failure they will transplant me. I have seen a hepatologist, (liver doctor), a gastroenterologist, a team of doctors at the transplant clinic/liver specialists, and all agree that the biopsies reveal a toxic response (similar to if you had taken an overdose of Tylenol.) SO YES, TAMOXIFEN IS A KNOWN HEPATOTOXIC DRUG AND WILL TAKE A MILDLY FATTY LIVER AND RACE IT TO THE FINISHLINE. I AM LIVING (for now) PROOF. I start a 1/2 dose of Letrozole next week. I am praying my liver can tolerate it. Cheers, Liz
0 -
Yes! Had taxotere this summer..5 weeks in started having right side pain like crazy..was made to feel like it wasnt normal..finally had CT scan which showed enlarged liver but enzymes normal..gained 9 lbs the week pain started..stomach bloated..they found a very hard edge on liver..i had to research on my own..the GI nurse prac finally made me feel like i wasnt crazy! But then f/u w GI doc and he told me i prob had fatty liver for a few years and it was not the chemo..i say BS to that..4 months later its finally getting better..i hope it goes well for you
0 -
I know this is an older thread, but just wanted to cross post. Hope555 you are not wrong. There is so much research and studies on the effects of Tamox and damage/risk to the liver.
So please forgive me as I link some studies and information. I just think SO many BC patients need to be aware of the risk to our livers with Tamoxifen.
Hugs and healing to all.
--------------
(cross posted)
I'm just going to add this link, it goes to a thread where a member posted her experience with Tamoxifen.
I feel like anyone deciding on this hormone treatment should be aware of possible damage and risk to their liver, as I was never made aware of this by my MO or team.
Please, as her story illustrates, at the very least, before starting Tamoxifen, have a liver enzyme test run. Better safe than sorry and needing a liver transplant because of the damage!
(Reference post is written by CanadaLiz on 12/15/2018)
https://community.breastcancer.org/forum/78/topics/868854?page=1#idx_29
Symptoms to be aware of:
https://www.breastcancer.org/treatment/side_effects/liver_probs
Here are a few studies for info:
A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462391/
"In addition, fatty liver disease, also known as non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH), was observed in more than 30% of patients with breast cancer who received tamoxifen as adjuvant therapy.10,11 The first anastrozole-induced hepatotoxicity case was reported in 2006.12 A retrospective study demonstrated that fatty liver disease detected using ultrasound was more frequently seen with tamoxifen than with anastrozole (30.4% vs 6.25%).13 "Association between tamoxifen treatment and the development of different stages of nonalcoholic fatty liver disease
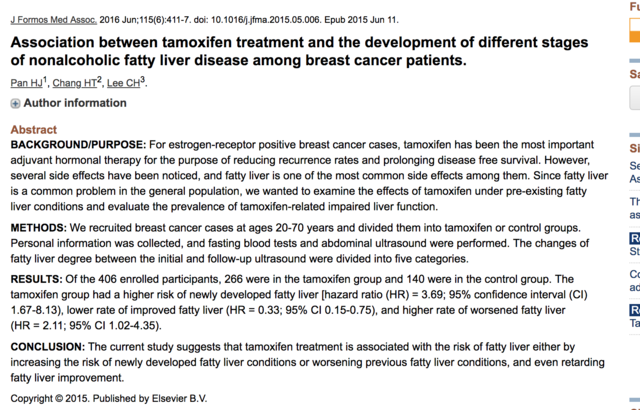
https://www.ncbi.nlm.nih.gov/pubmed/26071793
https://www.sciencedirect.com/science/article/pii/S092966461500176X
"Several studies showed that taking tamoxifen may incur a 30–40% risk of developing nonalcoholic fatty liver disease(NAFLD), according to different diagnosis instruments."ConclusionThe current study suggests that tamoxifen treatment is associated with the risk of fatty liver either by increasing the risk of newly developed fatty liver conditions or worsening previous fatty liver conditions, and even retarding fatty liver improvement."
"Our study suggests that tamoxifen is associated with the risk of NAFLD development, either by increasing the developed fatty liver or worsening the previous fatty liver condition and even retarding fatty liver improvement. The severity of fatty liver is associated with higher rates of abnormal LFT. During the follow-up period, regular abdominal ultrasound checkup, not just for detecting liver nodules, but also for identifying fatty liver change, is crucial. Further checking of liver function and other metabolic conditions once the fatty liver condition has progressed is essential."
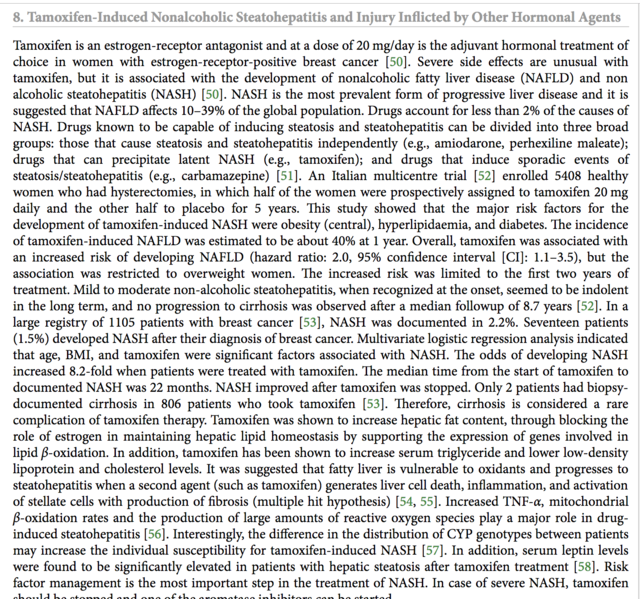
Drug Record: Tamoxifen
https://livertox.nih.gov/Tamoxifen.htm
"Outcome and ManagementWhile fatty liver arises in at least one third of women treated with tamoxifen for up to 5 years, clinically significant steatohepatitis is less common. Nevertheless, monitoring of serum aminotransferase levels during tamoxifen therapy is appropriate. In women with persistent elevations in ALT levels, the relative benefits and risks of continuing tamoxifen therapy must be weighed. Factors to help in the decision, include noninvasive tests for hepatic fibrosis (platelet count), imaging of the liver and, in some instances, liver biopsy. Other approaches short of stopping tamoxifen therapy include nutritional advice and weight loss, abstinence from alcohol, and possibly medical therapies for nonalcoholic steatohepatitis (which are currently investigational and have not been shown to be specifically helpful in tamoxifen induced fatty liver). The possible development of serious hepatic fibrosis and portal hypertension can be assessed noninvasively by serial determinations of platelet count, but may require liver biopsy to document."
Tamoxifen induces hepatotoxicity and changes to hepatocyte morphology
https://www.spandidos-publications.com/10.3892/br.2015.536
"Clinically, patients who accept the endocrinotherapy are instructed to reexamine their liver function every 4 months due to its hepatotoxicity. Numerous research and clinical studies have illustrated clearly that TAM causes the inhibition of mitochondrial β-oxidation and subsequently leads to macrovacuolar steatosis (21,22). The early symptoms were characterized by the presence of a single, large lipid vacuole within the cytoplasm of the hepatocytes (23)."
"In conclusion, the present data showed that a relatively low concentration of TAM (6 mg/kg/day) for a short time treatment (2 weeks) would cause hepatotoxicity and change morphology at the microscopic and ultrastructural levels. Although the liver function may compensate or reverse the injuries gradually, the damage that occurred in the short-term TAM therapy has been shown. Thus, there is a necessity to obtain measures for monitoring liver function and protection at the early stage of the TAM endocrinotherapy, prior to apparent and undesirable clinical symptoms occurring. Furthermore, as DNA damage also occurs at this early period without clear clinical symptoms, which in the long-run increases the risk of hepatocarcinoma, exploring alternatives for TAM in long-term clinical endocrinotherapy is required."
Liver Injury Induced by Anticancer Chemotherapy and Radiation Therapy
https://www.hindawi.com/journals/ijh/2013/815105/
Death due to liver failure during endocrine therapy for premenopausal breast cancerhttps://www.tandfonline.com/doi/full/10.3109/0284186X.2010.484813
"In the tamoxifen product information, liver-related side effects are listed and it is recommended to perform periodic liver function tests, although in clinical practice blood tests are no longer performed routinely during follow-up for women with early breast cancer."
"Young women, in particular between ages 26 to 35, seem to be—for yet unknown reasons—more frequently affected by acute liver failure, and the use of antidepressants (metabolized primarily via liver enzymes CYP 3A4, 2D6, 2C19), other potentially hepatotoxic drugs (e.g. acetaminophen-type analgesics and NSAIDs), and alcohol are more frequent in younger breast cancer patients than generally presumed and reported. We therefore advise physicians to pay special attention to patients treated with endocrine therapy for breast cancer who have concurrent depression and who potentially or actively consume hepatotoxic drugs and alcohol. Such patients should have their liver function monitored and liver imaging should be performed if indicated."
The Association of Nonalcoholic Steatohepatitis and Tamoxifen in Patients With Breast Cancer
https://onlinelibrary.wiley.com/doi/pdf/10.1002/cncr.24374
A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer
https://pdfs.semanticscholar.org/3aa1/d236d38c20f3a9377dea6f9d5ad8235221c6.pdf
G.L.O.W.N. - Tamoxifen
https://www.glowm.com/resources/glowm/cd/pages/drugs/t002.html
"Effects on lab test results
• May increase BUN, calcium, and liver enzyme levels.
• May decrease WBC and platelet counts.Special considerations
• Tamoxifen acts as an antiestrogen. Best results occur in patients with positive estrogen receptors.
• Adverse reactions are usually minor and well tolerated. They usually can be controlled by dose reduction. ALERT Serious, life-threatening, or fatal events associated with tamoxifen in the risk reduction setting include endometrial cancer, uterine sarcoma, stroke, and pulmonary embolism.
ALERT Serious, life-threatening, or fatal events associated with tamoxifen in the risk reduction setting include endometrial cancer, uterine sarcoma, stroke, and pulmonary embolism.  ALERT Discuss the potential benefits versus the potential risks with women considering treatment to reduce their risk of developing breast cancer. Benefits of therapy outweigh risks in women diagnosed with breast cancer.
ALERT Discuss the potential benefits versus the potential risks with women considering treatment to reduce their risk of developing breast cancer. Benefits of therapy outweigh risks in women diagnosed with breast cancer.
• Clotting factor abnormalities may occur with prolonged tamoxifen therapy at usual doses.
• Variations on karyopyknotic index in vaginal smears and various degrees of estrogen effect on Papanicolaou smears have been seen in some postmenopausal patients. May increase serum thyroxine concentrations and may be explained by increases in thyroxine-binding globulin.
• Initial adverse reactions (increased bone pain) may be a sign of good tumor response shortly after starting tamoxifen therapy.
• Monitor WBC count, platelet count, and periodic liver function tests results.
• Monitor serum calcium levels; hypercalcemia may occur early in therapy in patients with bone metastases."0 -
Hi all, I know this is an old thread, but I believe Tamoxifen has affected my liver too.
I only started taking it in March this year, and all my liver functions tests were normal back then. In June I had a hysterectomy, and during the surgery my surgeon noticed a nodule on my liver that she didn't like the look of. So I had an MRI of my liver done, and the nodule did not show up, but it did show I had a diffuse fatty liver, and more blood tests were recommended. I had the Liver panel blood test last week. It showed my AST and ALT levels are both high. The ALT went from a normal 20 IU/L to 81 IU/L in the space of 5 months. I have an appointment with my MO next week, and will be taking all the tests I had done with me. I'm just wondering if anyone else had elavated liver enzymes along with the fatty liver, and did any of you stop taking the Tamoxifen?
0 -
My pcp follows me on labs every 4 mo. In Sept back for lipid panel and cmp. I have nafl. The enzymes go up and down. T is said to be a possible contributing culprit but I'm not worried about it since when my cholesterol improves so do my liver enzymes. Diet is big. I can't stop taking it with my profile and luckily no terrible ses. Can't tolerate AIs.
0 -
Well, crap. I guess I have to give up taking Tylenol to be on the safe side (not that it does much good on joint pain). Since I can't take other NSAIDS and I have arthritis everywhere plus other muscle pain, this is really going to ruin any quality of life. I guess starting drinking is out of the question, too?
0 -
My liver enzymes increased while I was on Tamoxifen. Once I switched to Arimidex, they stabilized. But Arimidex caused significant bone loss despite the fact that I take calcium supplements and do lots of weight bearing exercise. Choices..
0 -
don't think tylenol effects liver enzymes. You can't be so "safe" that your quality of life suffers. As said, there needs to be balance.
I don't know your situation Alice, but I went years on arthritic knees. Only my right one wasn't bad. Felt bad because I was heavily compensating on it. My back with arthritis was worse because my knee was out of alignment as well. After my left knee replacement and now 4 mo out, should have done it sooner. Just being able to walk normal has really improved my overall discomfort as well.
0 -
Arista928, my urologist warned me about Tylenol causing liver damage. I had a kidney removed last year due to cancer, which is why other NSAIDS are off limits. I don't know if Tylenol affects liver enzymes, but it does have a negative impact on the liver in general. If Tamoxifen also has a negative affect, taking both cannot be good. I've had a hip replacement, so I know how great joint surgery can be. Unfortunately, two of my friends who have had knee replacements have NOT had improvement, which makes me wary of that particular surgery - besides being sick of surgery after three last year.
0 -
surgeon is critical for result of joint replacements as well as doing the difficult painful rehab. I worked for 2 joint replacement surgeons who all they have ever done and do are hip and knee replacements. Dearborn and Sah are contracted with Washington Hospital Center for joint replacement here in Fremont CA. People travel from all over the nation for them. But if you don't keep on track with PT then you won't have good results. Knee replacement is harder and more painful rehab than hip.
0 -
I just read everything in your thread and completely agree. I am currently suffering from NASH following 9 years on 20 mg of daily Tamoxifen use. After completing the standard 5 years my Oncologist said new studies show that an additional 5 years on it has shown to increase percentage of non reoccurrence rates. I THOUGHT I was tolerating the drug well and opted to stay on it. All throughout my chemo and even after in my maintenance visits my oncologist would say my liver enzyme levels were slightly elevated but never gave me cause to worry. Just said lose some weight. That was nearly impossible on Tamoxifen. All this to say an ultrasound and liver biopsy show I now am suffering from liver damage and my liver is severely scarred. Oncologist refused to say it was the Tamoxifen but it was the first thing he said to STOP immediately. Wish I knew this before. Wish he had checked my liver w an ultrasound before continuing the extended use. Trying to detoxify my liver but have been told it will take years. The information in your articles that you attached were extremely valuable and informative.. thank you!
0 -
Dear azshbaro,
Welcome to the BCO community. We are so sorry for what you are going through and glad that you reached out and found some helpful information here. We hope that you will stay active and connect with others. Keep us posted on how things continue for you. Let us know if we can be of help in your navigation around the boards.
The Mods
0 -
Same thing happened to me. On tamoxifen for 1 1/2 years. Mildly elevated ALT. Abdominal ultrasound shows fatty liver. Triglycerides doubled in past year. Primary says not a cause, oncologist says definitely is. Disconcerting..
0 -
Excessive Tylenol can kill you via liver failure. https://www.fda.gov/consumers/consumer-updates/acetaminophen-avoiding-liver-injury for example. Tylenol has a smaller non-toxic dose range than many medications.
0 -
I have fatty liver but I am fat. Triglycerides are high. I think the only way to know if it's the T is a culprit is to keep everything the same and stop T. I know it takes awhile to get out of the system.
I just had labs today and triglycerides are higher. But I haven't been taking Lovaza which is rx strength amino acids that helps lower it. I don't want to be on cholesterol meds for fear of additional ses.
0 -
I was diagnosed with a fatty liver in March 2018 then breast cancer in Nov.2018. My doctor told me to reduce carbs in my diet. My ALT level has been mildly elevated, but it hasn't been tested since I started Tamoxifen. I also had a knee injury prior to starting radiation and was on Tylenol and Ibuprofen routinely which can also elevate your ALT. My next liver function lab is in Dec. My primary put me on pravastatin 20mg on M-W-F its supposed to be gentle on your liver. I try to not take any Tylenol. I have reduced Ibuprofen to only one dose if necessary. I have never been a pill taker, but now I take a lot of supplements. I like Sports Research brand from Amazon because usually its just one pill a day and goes on sale frequently. I take their Omega-3 fish oil and Krill oil. I take Costco's 300mg CoQ10 and buy Extra Strength Nature Made Magnesium there. I recently added Milk Thistle with 80mg of silymarin. I am hoping all of this will help, but only time will tell. I started the Livestrong program this week.
0 -
pravastatin is an newer and expensive statin but I have heard very good things about it.
After chemo I had Fatty liver and developed insulin resistance ( my A1C went into the 6.0 range) I was able to lower my liver enzymes by adding greens and cruciferous to my diet ( Broccoli sprouts, Kale, spinach, coleslaw) I also upped all my vegetables and fruit to the 10 a day range and cut my fat intake and leaned out the protein.
After doing that I still couldn't drop any weight or lower my A1C so now I am working on that along with Cholesterol. Please post an update on pravastatin because I am hoping it won't cause muscle aches and many of the other side effects associated with statins.
0 -
Hi exercise_guru, I was worried about the side effects of the pravastatin/tamoxifen and talked it over with my doctor. So far so good with only taking it 3x a week. I am trying to eat healthy and exercise. My daughter's friend lowered her A1C with the keto diet, but that isn't a real healthy diet long term. I will post again when I get my results. Good luck to you!
0 -
During my last visit to see my MO, I actually saw her Nurse Practitioner. I brought up the fact that I had been diagnosed with fatty liver disease and that my liver enzymes were elevated, and asked if it could be the Tamoxifen. She said "no" very dismissively. When I pointed out that my enzymes were normal before I started taking Tamoxifen just 5 months earlier, she agreed there is a 5 % risk of liver side effects. "We don't do blood tests here anyway, you should get your primary care to recheck it" she said. So I asked "what was the blood taken for not 15 minutes before my appointment?" pointing to the bandage still on my arm for effect. "Oh" she said. She looked up the order, and guess what? Along with the usual CBC, and CMP, was a liver function panel! It's almost as if the MO is checking the liver enzymes as there are known issues! Who knew? Well the nurse practitioner didn't! I won't be seeing her again.
0 -
My pcp does my labs right now every 4 mo. Last week was cmp and lipid. She's aware of what T can do so she checks it.
0