Catching Mets Early? Docs say it doesnt matter?
Comments
-
Wow. These responses have been fascinating. I especially appreciate the sharing of the personal stories. Thanks for continuing the conversation.
0 -
Lago - do you know if the article you posted referred to local or metastatic recurrence?
0 -
JoanQuilts I don't know for sure but the article uses language like cancer returning and recurrence after 5 years. If I'm not mistaken usually local recurrence happens before 5 years. So my assumption is metastatic but I bet your onc would be familiar with the study since it was published in the Journal of the National Cancer Institute.
There may be newer studies too since this article is from: Aug 12, 2008
0 -
Thanks Lago. I am trying to reconcile this with what my onc told me. I am being treated for Stage 1, but I am triple negative. He told me that without chemo, I had an approximately 25% of distant metastasis but chemo would cut that by one-third, bringing it down to about 15%. I don't know the time period associated with that risk but I do know that with triple negative, the risk is greatest in the first three years - perhaps that is what he was referring to and the 7% quoted in the article is, as they say, after 5 years.
All I know is that despite the fact that I had a very small tumor (9 mm) my risk of metastasis without chemo (25%) is unacceptably high. I was shocked. Even with chemo, 15% is too high. And yet, I am one of the "lucky" ones.
0 -
Joan triple negatives and HER2+ are aggressive cancers and do tend to recur early. But then like the article says they don't tend to reoccur late. Granted I'm not sure what this means for triple positive(some of us high grade some of mid grade).
Which chemo,Hereceptin, AIs and surgery my recurrence risk in 10 years was put at 14%. I wish it were lower too but it is what it is. (Without surgery only for me was 58%.
We just have to look at how full our glass is. We have pretty full mug of NED in 10 years don't we… it's just not topped off.
0 -
JoanQuilts ~ Just reading your sig line...19 years! Were you triple negative then? (or maybe they didn't "test" the same back then since HER2 was not out yet, right?) I'm assuming you were monitored very closely since then, hence the reason that they caught it so early the second time around? But like you said...even catching it early..having a 25% chance of metastasis w/out chemo is unacceptly high.0
-
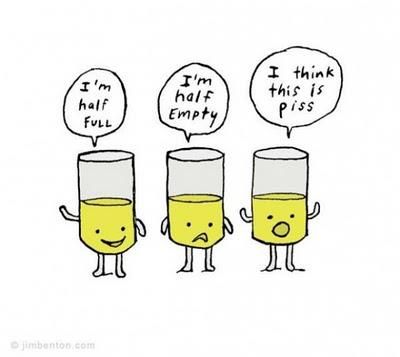
"We just have to look at how full our glass is..."
lago, that reminds me of a cartoon I saw......I usually have the 1/2 full attitude...but some days it really is just piss.

 0
0 -
OMG, that's hilarious LOL!
 0
0 -
Piss isn't that cute. (too funny)
0 -
SusansGarden - yes, to the best of our knowledge, I was triple negative 19 years ago. I was certainly ER and PR-. At the time my pathology report said they couldn't get enough of a sample to test for Her 2. So we do assume that I was triple neg then and definitely now.
The reason they call my new cancer a new primary is that the first was slow growing and this one is grade 3. While the onco doesn't think it makes a difference to my prognosis whether or not it is a new primary or a recurrence, I prefer to think of it as a new primary - I don't like the idea that &^%& could have been lurking around in my body for 19 years.
And yes, thank God for the close monitoring. A very sharp radiologist found first a DCIS in the same breast during my annual mammogram, and then the follow-up sonogram WHICH I ALWAYS GET DUE TO MY HISTORY showed a new nodule close by. Both were positive for IDC. Since it was in the same breast, which had already been radiated, I had no choice but a mastectomy and chose a bilateral. Two breast cancers in one lifetime (I'm still only 53) are enough, dontcha think?

The reason I'm so bitter and twisted (LOL - not really - I've had a reasonably good attitude this time) is because I can assure you, I had stopped worrying about metasteses somewhere around the 15 year mark. Now I have to start worrying about them again. Had I had a mastectomy way back when, I wouldn't have had the new primary tumor. But still, I don't regret it at all - the lumpectomy allowed me to keep my breast for another 19 years and at age 34 that was pretty important to me.
I'll get past this with the help of all of you! Thanks Susangarden and Lago.
0 -
I like your attitude, Joan.

~ Susan
0 -
Informative if disturbing thread. The thing that stays with me is the idea that we are statistics/outcomes...as I said before I don't like the use of the word "probably" by my MO and I think it was barsco who heard the word "usually" from her MO. Those are casino words, not medical treatment words. It also bothers me that "outcomes won't change" would be considered a reason to delay treatment when it would mean QOL for so many women. Finally, the idea that treatment is so unbelievably uneven...I didn't know this woman that so many of you loved and admired, but the fact that she didn't have access to the care that would have prolonged her time or made it better just breaks my heart. I wonder if more care, and better record sharing among doctors might make a difference in this fight.
0 -
Joan I'm with you. sounds like a new primary to me. You beat this once you'll beat it again. I know several who have. Don't blame you for wanting to keep your breast at age 34. I got married (1st & current DH) 3 months before my 34th birthday.0
-
What we need to keep in mind is that when many oncs don't scan after tx, they don't say, "No scans ever". What they say is "Scans if there are symptoms". One of the reasons is the very high level of radiation in the scans, and that's no small worry.
What is terrible about Mary's case is that she didn't get scans or tx despite serious symptoms. That's what's tragic.
Leah
0 -
I wish to second and underscore with an explanation mark what Leah just said. The tragedy is that our sister was not given a proper work up after she became symptomatic. In Dr. H. Gilbert Welch's book, Overdiagnosed he discusses how unnecessary much screening is. However, when people are symptomatic, that's when diagnostic testing is ABSOLUTELY NECESSARY.
0 -
I think a correct statement to make is that routine scanning / screening for symptom-less mets has never been proven to increase survival in enough people, to justify the cost. And it would be a huge cost -- just think of all the BC survivors there are.
I also think there is a middle ground between scanning symptom-less women, and waiting until your pain and symptoms are completely unbearable. I think most primary care docs and oncologists will agree that any sort of unusual, persistent pains in a BC survivor warrant at least a follow up visit with your oncologist. I've heard a "two-week" rule to be helpful; you shouldn't wait forever, but don't run to the doctor with every little ache and pain.
There is also something in epidemiology called a screening effect. It's kind of a "we make survivors" effect. So you catch a cancer diagnosis, either initial or recurrence, a year early with screening vs. just watchful waiting or symptom-waiting (e.g. waiting until you develop a lump or medium pain). Post-diagnosis survival time increases, statistically. Hurray? Maybe. Or maybe you would develop cancer (or die) at the same time, with an extra year tacked on FROM THE BEGINNING -- with the additional psychological and medical burden of being a cancer patient. Now if you can statistically prove that an agressively screened group lives as a WHOLE longer when compared with an unscreened group, THAT is medically significant and very good news indeed.
Also, be aware of where bone mets do and don't go. They generally will go to the torso: spine and ribs and hips -- those areas are worrisome with persistent pain. They don't go to fingers and toes -- that is much more likely to be joint pain or arthritis.
0 -
I have bone mets with no symptoms at all. Ribs and sternum, don't feel a thing. But I do think that the fact they found them now when they are still smallish and contained to the bone and I've started treating them now is much better than if they had been found after there was an issue such as pain. Given more time to grow and spread to organs with no treatment would, I believe, shorten my life span.
0 -
Are there women out there who don't ever progress to mets after the initial diagnosis? Or is it inevitable that if you are young enough when diagnosed that it will eventually come back and get you?
0 -
My SIL was dx'd with BC had a bi-lat mastectomy no chemo and no rads.....she is still just fine. That was over thirty years ago. It does happen that after treatment everything is fine but it can just as easily not be.................it really is a crap shoot.
0 -
It sometimes feels that way JG - I feel as if I am always edging closer to recurrence. But then I had a localised recurrence 10 years after my first (allegedly) benign lump - so I know how this bugger can sneak back up on you years later.
My aunt was dx-ed at age 35. She is the size of a small rhino, is now diabetic and has always been alcohol dependent. She has been cancer free for 40 years. My dear friend who was a professional sportswoman (no cigarettes, no booze, slim and very fit) was dead within 2 years of diagnosis. Crap shoot it most certainly is.
0 -
jgbarlett I think that's the jist of the article I posted earlier. Most women seem to think mets happens more often than not. Once you pass the 5 year mark your chances of recurrence goes down and even further after the 10 year mark… but some will recur after those time periods, but the number is much less than those who don't. BTW there is a woman in my building that is a 35 year survivor.
I had the very same question about a year ago… I think we all wondered that at one time.
0 -
Thanks otter:)
The leaping goat is here for awhile:) makes me smile and so happy if it does the same for anyone else!0 -
I like it too but I thought it was a little lamb
0 -
I love the little critter, whatever it is, and it definitely makes me smile! Sproing!
Going back to the "probably" topic: Recently I was looking back through my reports and reread my breast mri that was done before surgery. "There are several small areas bilaterally that are PROBABLY benign." Wha?? Well, that's comforting.
I met with my tax attorney last week to do taxes, and his wife had been diagnosed around the same time as me with Stage II on one side and stage III on the other - at the same time. She had MX on one side (I guess the III) and a lumpectomy on the other.
I guess if you live a long time and die from something other than BC, you beat the odds. Greenfrog - with your aunt's other health issues, she likely will fall into this category. Your friend's story is so sad, though.
0 -
Some metastatic cancers seem to be more responsive to treatment at an earlier stage than at a late stage and therefore survival times can be prolonged the earlier it is caught.
http://jnci.oxfordjournals.org/content/102/7/456.full
A distinctive subset of MBC patients who are most likely to gain substantial benefit from an intensified multidisciplinary therapeutic approach is represented by "oligometastatic" disease, which is characterized by solitary or few detectable metastatic lesions that are usually limited to a single organ. This population of "potentially curable" stage IV disease is estimated to be 1%-10% of newly diagnosed MBC patients (6). The existing guidelines (National Comprehensive Cancer Network [NCCN] Clinical Practice Guidelines in Oncology, European Society for Medical Oncology [ESMO] Clinical Recommendations) list surgery, radiation, and regional chemotherapy as possible therapeutic options in patients with localized metastatic disease (7,8).
The European School of Oncology-Metastatic Breast Cancer (ESO-MBC) Task Force addressed the management of these patients in its first consensus recommendations, stating: "A small but very important subset of MBC patients, for example those with a solitary metastatic lesion, can achieve complete remission and a long survival. A more aggressive and multidisciplinary approach should be considered for these selected patients. A clinical trial addressing this specific situation is needed" (9).
I got the aggressive and multidisciplinary approach, achieved complete remission in Feb. 2008 and am hoping for a long survival.
0 -
SusanGardens - Thanks for starting this thread. I've just read all the posts and appreciate the dynamic conversation.
Heidihill - I'm so glad that you've done well with your aggressive,multidisciplinary treatment. The article you linked was so comprehensive and informative. I pray that you fall into that percent that achieves long term NED.
My MO does absolutely no radioigraphic or tumor marking screening for recurrance quoting what so many of you have said. Hum, does the info in this article make me wish I had regular screening or does it only pertain to women diagnosed St IV from the start?
0 -
JG: ABSOLUTELY there are women who never progress to mets. I believe the majority of women who are diagnosed with bc never progress.
0 -
MJL... Your points are EXACTLY the ones that Dr. Welch makes in his book...... Spot on!
0 -
The screening "making survivors effect" that MJL talks about is what intrigues me and seems to be one of the reasons behind the docs saying "finding it early doesn't matter". (This is also discussed in the History of Cancer book)
example 1) Find mets early (w/out symptoms) in 2012 ...treat for 5 years and die in 2017.
example 2) Find mets later (after symptoms) in 2016..treat for one year and die in 2017.
#1 survived mets for 5 years...while #2 only survived mets for 1 year? Not really.
But would you rather live 5 years knowing you have mets or 1 year? Like someone responded earlier...maybe it would be nice to know earlier so that you could stop "going through motions" and do the things you wanted to do? I understand and try to "live life to it's fullest"..but my practical side feels that it is different than knowing your time on this earth is shortened. I certainly would pull some money out of retirement and take more vacations!

I realise there is no way we can know any of this for certain and that there are rare specific cases that are caught early and remain NED. I personally think our best hope is the genetic mapping of cancer to find individualized treatments as it becomes more and more obvious that cancer is not a "one size fits all".
Thanks again for sharing and philosophizing with me. I always loved that class in college.
~ Susan
0 -
"But would you rather live 5 years knowing you have mets or 1 year?"
The way I look at it, I would rather have 5 more yrs with my family & friends than just one more yr. I know that it is the same amount of time really, but there is the illusion of having lived longer with mets and having those extra yrs. Also, knowing that I have mets has not only changed the focus of my life, I have definitely noticed a change in the outlooks of my DH, DS as well as extended family and friends.
0