Asymmetrical area on one breast?
I recently had a diagnostic mammo and ultrasound of one breast for a lump. Nothing was seen in the area of the breast lump but one of the images showed an area that the radiologist wanted more images of so they repeated the 2 original images and then a spot compression before sending me off for the ultrasound, which found nothing. When I asked the tech why more images were needed she said that the radiologist mentioned that perhaps there was some overlapping tissue and he wanted a clearer picture and yesterday when I spoke to the doctor's office it was referred to as "an area of asymmetry" and now I need to go in for a mammogram with contrast. After more reading about possible causes of an area of asymmetry on one breast, I did see that overlapping tissue is a possibility but the extra images and mainly the spot compression should have resolved that so I'm really worried as to why I am being sent for the mammo with contrast.
How concerning is an area of asymmetry? I thought perhaps the mammo with contrast was to investigate the lump that wasn't seen on mammo or ultrasound but from what I was told it is for a better look at the asymmetry in another part of the breast unrelated to the lump. Having just watched my mother take her last breath a few months ago because of breast cancer, I am more than freaked out at this point.
Comments
-
Golden
As you may know, a mammogram looks a bit like an ink blot test, that is, fairly symmetrical from one side to the other. If there is an area of breast tissue density on one side that does not appear near the same part of the other that is called an asymmetry. If it were a mass they would have said mass and described its appearance. Once an area of asymmetry is detected it is compared to the previous year's study to see if it is new or if this is just the way your breast tissue is distributed. Did they have your prior studies for comparison? If so I have to assume this is a new finding and worth the additional imaging. If this is your first mammogram, additional views are commonly obtained.
The standard followup is a set of compression images to see if it is overlap. If it does not resolve with those an ultrasound is performed. If the ultrasound does not demonstrate any findings one needs an exam as a tiebreaker which in the case of your facility that's a mammogram with contrast. Since no discrete mass was seen, that lowers the probability that the asymmetry represents invasive ductal carcinoma, however it is more difficult to exclude invasive lobular carcinoma as this can present as only a new asymmetric density. Can you post your reports here for us to see?
My thought is they are going the extra mile on your imaging because of your family history, I assume you told them of your mother's recent passing from the disease and how that affected you. Let us know how the next exam turns out.
0 -
GoldenGirls,
I can't give you any better understanding or advice than DJMammo. Try to stay as calm as possible, and not go too far down that "what if" road; it only causes anxiety, frequently for no reason. Follow up, and post your reports here for help understanding. Good luck!
0 -
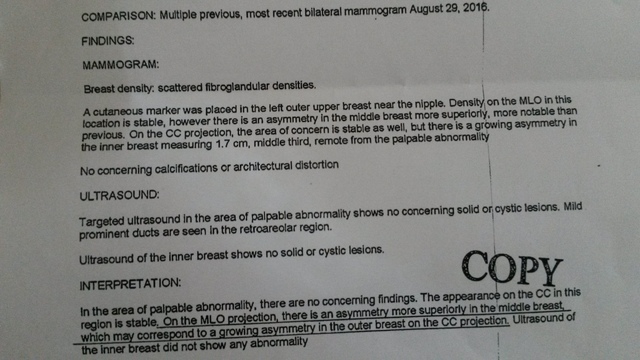
DJMammo -- I was finally able to get a copy of the report from the diagnostic mammo and ultrasound and am now more concerned than I was before seeing it for myself. The mammo with contrast will be this coming Monday.
 0
0 -
GG
It is encouraging that nothing was seen on ultrasound.
Let us know how the mammo with contrast turns out
0 -
My immediate concern after seeing the report was ILC because of the new asymmetry and the prominent ducts. I have a question - Can changes in body weight cause new asymmetry? I had lost just over 20 Lbs since my last mammogram (and gained back 7 in the couple of months following my mom's death). I wondered if this could have something to do with the changes. Maybe I'm just grasping now. lol
0 -
GG
The short answer is yes, in general if one loses a lot of weight specifically fat, the breast which contains a fair amount of fat will decrease in size accordingly. The fat interspersed between the more dense fibrous and glandular tissue will decrease in volume and the dense areas will be closer together simulating an overall increase in breast density.
As to whether or not it is specifically related to the new asymmetry? It's possible. Did the rad reading the study have the history of weight loss at the time ?
0 -
Thanks for answering. I really appreciate the insight.
No. I didn't think to mention it and doctor who ordered the mammo in the first place was one I'd never seen before so she wouldn't know I'd lost weight.
0 -
it can help when the rad is comparing old and new studies
0 -
Thanks! I will definitely mention it on Monday when I go in.
0 -
My doctor's office finally got the report from the CEDM and instead of telling me over the phone what it said like they normally do, I was instead told the doctor wanted to see me. They booked me an appointment for Monday. Naturally, I got upset and asked for details and after being placed on hold was told that there was "nothing worrisome" but the doctor still wants to see me. When I explained my anxiety (you kind of have to when you break out into a sobbing mess) she told me the doctor will call to talk to me by the end of the day-- also not the norm for this doctor's office. If there was nothing worrisome seen why would the doctor want to see me and talk to me? This has been such a long and stressful wait and now I'm more scared than before.
0 -
Good for you for pushing to get answers rather than be stressed out all weekend. Now, try your best to practice deep and even breathing and employ your best distraction strategies while you wait. Your questions will be answered soon. Good luck!
0 -
They gave me Bi-rads 3 and the area of concern, though there was some mild uptake, was hardly noticeable. Two radiologists looked at the images and believe it's benign. They also mentioned that these most recent images were more comparable to my diagnostic mammo results from 2012 as opposed to the one I did last month that found the asymmetry. They recommend spot compression mammo and ultrasound in 6 months but said that if I am still concerned about the original palpable lump that was not seen on any of the tests then I can get a referral to a surgeon.
My doctor and the radiologists seem very confident that there is nothing sinister going on so I may hold off on seeing a breast surgeon. I was pleased to FINALLY have my concerns for high-risk screening addressed and am being sent for a genetic assessment.
I feel relieved... not as relieved as I was hoping to, but certainly more at ease than the past month. Will relax... until the genetic assessment anyway. lol
0 -
Here's the report:
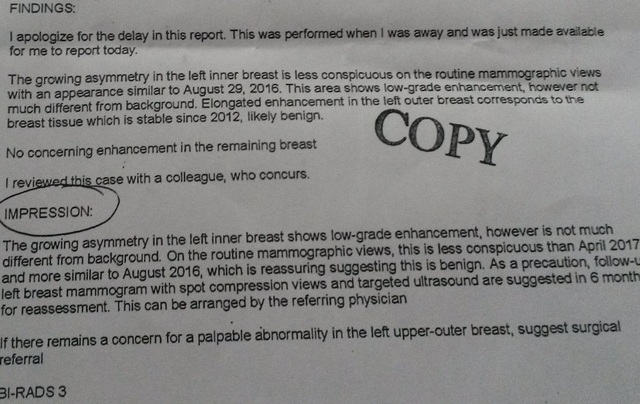 0
0 -
GG
So far so good! Keep your follow up appointment for imaging. If the lump is still a problem at that time make sure to remind the tech to place a skin marker on it again.
0 -
Thanks! Any idea what would cause this growing enhancement? I'm guessing overlapping tissue wasn't the cause if it was still somewhat visible on the CEDM. Could monthly changes or my "manhandling" of my left breast while constantly checking on the lump I felt (not seen on mammo) have caused some kind of swelling that could be seen on the mammos? I did manage to mostly keep my hands off my breast while waiting the two weeks for the CEDM. lol
0 -
GG
None of the breast centers I worked in offered CEDM so I have no practical experience with it, only what I have read on occasion. I cannot speak to its sensitivity or specificity. Personally, I primarily depend on Ultrasound to tell me if what I am seeing on the mammogram is "real" and the nature of its borders and internal structure
Opinion: There are two possibilities when nothing is seen at ultrasound: 1) there is actually nothing there 2) there is something there that is extremely subtle and so big that it will not fit in the field of view of the ultrasound an is thereby not detected. Number 1 is the usual answer.
I used to tell my residents "One old film is better than two old radiologists" when it came to interpreting a study with prior exams. Together with the negative ultrasound I am encouraged by the comment made about the similar appearance of the breast in 2012, a period of 5 years. We usually call things stable after 2 years.
Once again don't let me deter you from getting the follow up that was recommended but perhaps you should worry a little less. I have learned over the years you cannot say 'always' or 'never' in medicine and nowhere is that more applicable than breast imaging. Keep us looped in.
0