Anyone ER+ PR+ opting out of hormone therapy?
Comments
-
Cmck1973, the one thing I would say is that you have to make the treatment decision that is appropriate to your diagnosis, and your tolerance of risk.
With regard to your diagnosis, the key factors that influence recurrence risk are the age of the patient (higher risk if younger), the size of the area of DCIS, the grade of the DCIS, and the size of the surgical margins.
Are you familiar with the Van Nuys DCIS Index?
Choosing Treatment for Patients With Ductal Carcinoma In Situ: Fine Tuning the University of Southern California/Van Nuys Prognostic Index
The significance of the Van Nuys prognostic index in the management of ductal carcinoma in situ
.
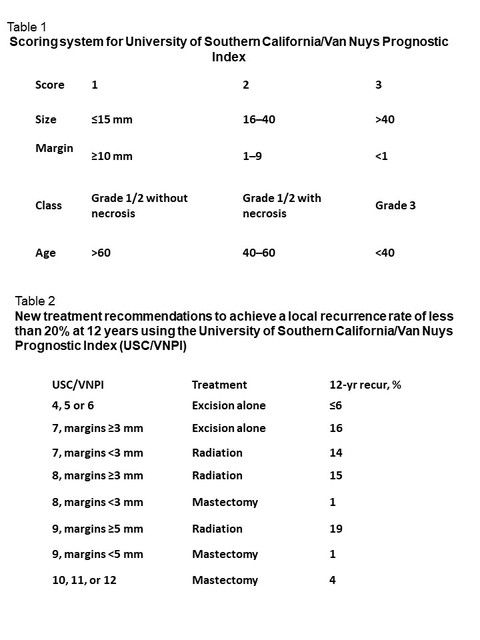
Here is a summary of how to calculate the score, and the recommended treatment based on the score. Note that the goal is to keep recurrence risk below 20% at 12 years, which does not include the benefit of endocrine therapy. Endocrine therapy would further reduce the local recurrence risk by approx. 45%. This means that, as an example, a 16% local recurrence risk would effectively become a 9% risk if the patient takes Tamoxifen or an AI. Local recurrences after a diagnosis of DCIS tend to be DCIS again in about 50% of cases, whereas the cells have evolved to become invasive cancer in the other 50% of cases. So this 9% risk equates to a 4.5% risk to develop invasive cancer within 12 years.
 0
0 -
Since I didn't mention it before .. I was 47 years old with my Stage 0.
0 -
I calculated my VNPI score to be 6 which would mean excision only is most likely a ‘safe’ bet however I could be that lucky person who is amongst the numbers who would develop the invasive recurrence, but it almost seems that person would have a recurrence regardless of adjunct treatment.
NicoleRod, You stated you had radiation, did your doctor have any guesses as to why it didn’t help? And are they certain that tamoxifen would’ve made a difference in your case? Did they test lymph nodes at the time of the initial diagnosis? Sorry for all the questions but it really helps to get details from someone who actually have go
0 -
Cmck1973,
If I may ask, what were your surgical margins? I think that is probably the most important factor affecting recurrence risk, since the nature of DCIS is that it tends to spread out in the ducts as the cells multiply, and DCIS is known to 'skip' in the ducts. It's interesting that although margin is already incorporated into the score, the Van Nuys index further emphasizes the critical nature of margins by having a different treatment recommendation for 7, 8 and 9 scores dependent on the size of the surgical margins.
Personally I might consider skipping rads with a larger grade 1 DCIS only if I had >1cm (10mm) margins, but not if the margins were smaller.
0 -
Cmck1973 No...my doctors or any doctors for that matter (I didn't have the same doctors at recurrence as I had with the first cancer) had no idea why. Like I said my husband and I feel for the vast majority of women with BC it's not a matter of "IF" its a matter of "WHEN". They are of course not certain that Tamoxifen would have made a difference as a matter of fact if you re-read my original post my MO at the time agreed with me that there was not enough evidence that Tamoxifen could make a big difference in Stage 0 , Not to confuse with Stage 1 each stage level higher is of course higher risk...but we will never know. I also like some others did not want to experience menupause symptoms and take meds if I didn't ABSOLUTELY NEED to. I feel that was stupid thinking on my part and knowing what I know now, even if I was not Stage IV right now..but if I would have been on this site when I was a Stage 0 and I would have known that if the BC did recur it tends to go to bones/organ I would have opted for the Tamoxifen and the BMX. I was naive and thought "I have a stage 0 this is all contained in the duct the doctors said I have like a 1 to 2% chance of recurrence that's nothing" That was so dumb on my part.
0 -
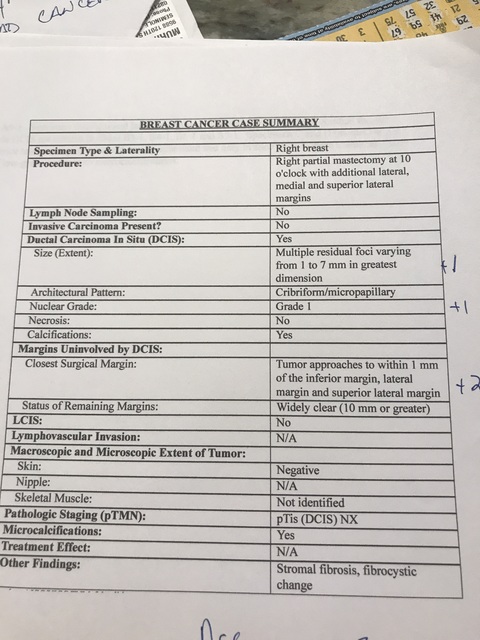
my report is a bit confusing, it says for most of the margins it’s widely clear but the closest margin is within 1mm
 0
0 -
Cmck,
My thoughts, as a fellow patient with no medical expertise, but based on having been on this site for 13 years.
1. Your DCIS is grade 1. That's good and signifies a lower risk to develop invasive cancer.
2. But it is multi-focal. "Multiple residual foci varying from 1 to 7mm in greatest dimension"
3. And you have 3 tiny margins. "within 1mm of the inferior margin, lateral margin, and superior lateral margin" I may be wrong, but I think that usually there are 6 margins that are identified and measured; you have extremely narrow margins on 3 - that's significant.
As I see it, combining points 2 and 3 puts the risk that you have residual DCIS in your breast to be very high. With close margins, it's always possible that some DCIS remains in the breast beyond those margins. And because you have more than one area of DCIS, multiple foci rather than a single defined area of DCIS, the risk is even greater that there could be additional foci of DCIS sitting in your breast beyond those 1mm margins. All this means that your recurrence risk could be quite high.
Until a particular research study came out a few years ago, 2mm was considered to be the minimally acceptable margin, and a re-excision would be done if margins were not at least 2mm (some surgeons would insist on at least 3mm). Radiation Oncologists would refuse to do rads unless margins were at least 2mm. This changed with the release of this research, but it always concerned me, because earlier research clearly showed that margins of less than 2mm resulted in a significantly higher recurrence rate.
The medical community is also not fully on board with this research, as this 2018 PubMed abstract shows: Margins in breast cancer: How much is enough? https://www.ncbi.nlm.nih.gov/pubmed/29338088 Note that a minimum 2mm margin is recommended for patients with DCIS who undergo a "lumpectomy and RT" (radiation therapy).
One option to consider is re-excision surgery. If no more DCIS is found, then you will be left with nice wide margins and there will be less risk in passing on rads. And if more DCIS is found, you will know you made the right decision
0 -
hi Beesie!
I met with the radiation oncologist today and he said exactly what you said above. He says if I refuse radiation then I need to go back to the surgeon and try to obtain better margins. Problem there is that it could find more and still not get clear margins and then I’m left with the decision of a Mastectomy. Sigh....I’m so frustrated. I wish I could just make a decision and be at peace with it
0 -
Well you know my opinion...double mastectomy hormone suppression...
0 -
Cmck,
I appreciate that you are worried about what re-excision surgery might find, but if you have more DCIS in your breast, don't you want to know? You can find out now, or you can find out in a few years when you have a recurrence - and by then, the cells might still be DCIS (it's to your advantage that your DCIS is grade 1) or it's also possible that the cells might have evolved to become invasive cancer.
Keep in mind that radiation reduces recurrence risk by 50%, which means that if you do still have a larger focus of DCIS left in your breast (i.e. more than just a few rogue cells) your recurrence risk might be quite high even after rads.
Re-excision surgery is usually an easy, quick surgery. As I said in my previous post, a re-excision will either provide you with nice wide surgical margins, giving you the opportunity to pass on radiation if you really want to do that, or it will remove DCIS that is still in your breast, which could lead to an invasive recurrence if not surgically removed.
Yes, it could happen that the margins still aren't clear after the re-excision, but when it comes to cancer cells (or pre-cancer cells, if you prefer that definition of DCIS) in your body, personally I don't believe that ignorance is bliss. People have colonoscopies so that pre-cancerous polyps can be removed while they are still harmless, thereby averting a diagnosis of colon cancer. A few years ago, I had a small mole removed - I'd had it all my life but it had started itching. To my dermatologist's surprise, it turned out to be a pre-cancer and she said that it was good that I'd caught it when I did, before it became cancerous. I understand not wanting to over-treat a low grade DCIS, but I think you'd agree that it's better to be dealing with a pre-cancer than an invasive cancer. That's the opportunity you have now. If you adequately and appropriately treat this diagnosis, you hopefully won't have to deal with a more serious diagnosis down the road.
I admit I'm surprised that your breast surgeon didn't immediate suggest a re-excision upon seeing your pathology report. When I was diagnosed 13 years ago, that would have been the recommendation from most every surgeon.
0 -
I’m a little annoyed that the surgeon didn’t suggest it. I really didn’t understand when I met with him, he made it sound like all the margins were great. Now I’m healed up from the original surgery and have to go through the healing process again. He’s also a bit of a condescending ass so I can only imagine how he is going to feel about me telling him to give it another go.
I know I sound like a whiner and I should be extremely happy that it is only a precancer but it’s frustrating to hear them tell me its no big deal and act like these treatments are equal to laser hair removal when I know there ar
0 -
I understand your frustration. Knowing that your situation is favorable compared to most doesn't mean that you don't have to deal with the uncertainty of the diagnosis, the after-effects of surgery and in your case, an ass of a surgeon. We want to trust that we are getting the best advice and full information from our doctors, and it is disappointing (to say the least) when a doctor does not provide recommendations that are consistent with current standard of care.
When you see the surgeon, bring along a hard copy of the PubMed article I linked in my earlier post and a copy of this article from the Journal of Clinical Oncology, detailing the consensus guideline on margins for DCIS, which happens to be 2mm.
0 -
I've not read all of this thread in detail but just wanted to weigh in that a re-excision is not a big deal. I needed one in 2016 (at the time I read it is very common--something like 25-40% of lumpectomies require one), so when 2018 came around, I told my BS to "go big"--really. I wanted HUGE margins. Let me also reiterate something I've posted often re: hormone suppression. I was having a general chat with my BS at a follow-up appt last year and we got on AIs (my 2016 DCIS was ER-/PR-, so that was not part of the conversation back then). While he's not an oncologist, he does know a LOT about BC. He said AIs give the biggest bang for the buck--that if he had a female relative who was refusing it, he'd grind it up and put it in her oatmeal. I've found that *for my dx/tx*, several of the recurrence predictor tools show that the AI is more effective in preventing a recurrence than chemo. While I continue to be less than thrilled about the SEs (just read an article yesterday about estrogen and brain function--oy!), I truly believe it is an important tool to prevent recurrence.
0 -
"He said AIs give the biggest bang for the buck--that if he had a female relative who was refusing it, he'd grind it up and put it in her oatmeal." Well, if that breast surgeon was my relative, he would be banished from my life. And my MO, whose area of research interest is the side effects of cancer treatment, would probably give that BS a big slap or at least a good talking to.
I fully agree that AIs and Tamoxifen are very important drugs that can be life saving, and in certain cases (early stage invasive cancer ER+/PR+ diagnoses) can be the most important treatment in the arsenal, but that is not a blanket statement that can be applied in all situations, and we need to be careful to consider differences between invasive cancer and DCIS - this is the DCIS forum. These drugs do come with side effects, some that affect quality of life and some that can cause serious health problems, and so the benefit of AIs and Tamoxifen have to be accessed relative to the risk faced by the patient.
Endocrine therapy provides 3 benefits:
- Reduction in local recurrence risk (by approx. 45%)
- Reduction in distant recurrence risk (by approx. 35%)
- Reduction in risk of development of a new primary breast cancer in either breast (by approx. 50%)
For someone who has a BMX for DCIS, with clear surgical margins and with no major high risk factors (such as being BRCA positive), the risk in the first category is only 1% - 2%, the risk is the second category is virtually zero, and the risk in the third category is only 1% - 2%. NCCN treatment guidelines recommend against endocrine therapy.
For someone who has a lumpectomy for a DCIS, the risk in the first category can be as low as about 5% or as high as about 50%, depending on the size and grade of the DCIS, and the surgical margins. While here again there is virtually no risk in the second category, the risk in the third category can be quite high - anyone diagnosed with invasive cancer or DCIS one time is at about double the risk of the average women to be diagnosed again, with a new primary in either breast. So a careful individual assessment is the best approach to determine whether or not endocrine therapy is an appropriate treatment.
For someone who has invasive cancer, regardless of whether they have a MX or a lumpectomy, there will always be a risk in the second category; a risk of mets is of course the greatest concern after a breast cancer diagnosis and for this reason, endocrine therapy is pretty much always recommended after an invasive cancer diagnosis. That said, for low risk diagnoses - small, non-aggressive invasive cancers where the risk of mets is in the single digits or even low single digits - many MOs will be perfectly fine if a patient decides to opt out of taking endocrine therapy or if she tries endocrine therapy but quits because of the side effects. It's a matter of individual risk and risk tolerance.
What it comes down is it that deciding to take, or not take, endocrine therapy is a personal decision, weighing the benefits of the drug vs. the risks and side effects from the drug, with consideration to other health issues the patient might have and the patient's risk level and tolerance of risk.
0 -
Sorry--didn't mean to throw my BS under the bus. I'm sure he was tailoring his comments to my diagnoses. I've had three, going back to ALH 10 years ago, and he was my surgeon on all of them. He retired late last year and I really miss him.
0 -
Ingerp, with 3 progressively more aggressive diagnoses and with you still having both your breasts, I'd grind up an AI and put it in your oatmeal too.
 0
0 -
Ingerp thank you for the reassurance regarding re-excision. I literally just texted my husband and said I am going to tell them that I want to go that route first so hearing that it’s not so bad is a good thing
0 -
Re-excision really is not bad- very quick and very easy recovery. A safe option.
0 -
Cmck1973, have you had the discussion yet with your surgeon about the re-excision? I'm wondering how he reacted.
0 -
Hello -- I'm going to jump in here, having skimmed this topic fairly well. THANK YOU to butterfly3 for asking these questions and to all who have contributed and posted links -- I have quite a few that I posted in new tabs to read at length, probably download for future reference. Beesie, you are a nation treasure!
A little about me -- I am a trained researcher. My PhD. is in psychology, but I worked on medical research in grad school, then did my best to coordinate care for my husband during his final illness, with the blessing of his internist at the VA (who faxed me all the labs, etc. so we could make decisions together.) Additionally, this is not my first cancer rodeo; lost a kidney to upper tract urothelial cell carcinoma (which is typically bladder cancer) in 2011 and read medical journals on that topic for several years.
As you can imagine, doctors either love working with me or are very threatened -- I prefer not to work with the latter. I just got my dx two days ago. I think it will show up below. My ER+/PR+ was 100%. I'm 66, 21 years past menopause, no HRT ever, and am about 30 pounds overweight. I also have moderate osteopenia, along with multi-level degenerative disc disease.
The main reason I logged in tonight was to see if there were any discussions about choosing a surgeon, but I think I know what I need to do, especially having read about so many factors that need to be taken into consideration when developing a treatment plan. My primary told me she didn't know much about the surgeon doing most of the breasts at our local hospital, but assumed she was OK. Here's what the surgeon's bio on the hospital website says:
Dr.____ practiced general surgery and hand surgery in Ventura, CA, from 2012 to 2015. She enjoys having a "bread and butter" practice focusing on hernias, breast pathology, gallbladder disease, acute surgical diseases, as well as carpal tunnel syndrome, trigger fingers, arthritis and tendon issues.
Her residency was in hand surgery. She also does colonoscopies. Her office referred me to the "cancer care team," which is a couple of nurses at the hospital (love nurses, but not sure how much they can do within this system.) The person who made my appointment said "The nurse will talk to you about that," when I asked about choosing an oncologist.
Dammit, I want a boob doctor. I want a doctor who has always been focused on, and passionate about beating breast cancer and never dreamed of a residency in any other specialty. I am less than an hour away from a teaching hospital where care is coordinated across disciplines for people with breast cancer diagnoses. This may be "just' DCIS to some people, but it's my DCIS and I want the best possible outcome for myself. Am I correct in assuming most here concur with me?
Not happy to be here, of course, but since i am, looking forward to learning from this group.
0 -
slh I don't know where you are but 10 years ago when I had ALH, my GYN referred me to a breast care practice with three breast surgeons. I know they were all good and I stuck with the one I originally had through my subsequent DCIS and IDC. (Loved him! Unfortunately he's recently retired.) Isn't there something similar where you are? A practice that just does breasts? If you're saying the closest is an hour away, it might be worth it for the surgery. And would your rads would be there too? That gets a little tougher, with treatment five days a week.
0 -
I, too, have been working with specialists. I cannot imagine being treated for my IDC by a general surgeon. My breast surgeon did an amazing job with my lumpectomy, my MO is the head of oncology & hematology, and my RO is similarly well qualified (and also a breast cancer survivor).
If you don't live near specialists, you might consider putting up with the inconvenience and expense of traveling so you get the best care.
0 -
Are you in California??/ If so got o Dr. Laura Kruper...City of Hope she is amazing. Did my double mastectomy. She is the Chief of Surgery there and does breasts all day everyday.
0 -
I'm in Oregon, and there is a guest house at the hospital for patients more than 30 miles away, where I could stay for consecutive days of radiation. I'm going to call my insurance company now to make sure they will cover it, then my PCP's nurse.
0 -
sih you should go with the specialists! I actually had a BS at a breast center close, but like you I wanted the whole package so decided to go an hour and 15 away. Just because I was looking at stage 1 didn't mean I shouldn't have the best team. I had a BS, a PS an RO and an MO. And all my MO does is BC. I had IORT (interoperative radiation) so I would only need 15 treatments of radiation, I actually drove each day. The drive wasn't bad and I really just wanted to sleep in my own bed. Remember you have time to make an educated decision. As my BS said this is an emotional emergency not a medical emergency. Good luck to you, we are all here to help support you in your decision.
0 -
Thank you, Ingerp, edj3, and Mymomsgirl! Actually, my Medicare Advantage Plan doesn't cover the hospital I want to go to, but there is another one in Portland that is very good, and I've spoken with their breast cancer navigator. Two of their surgeons are survivors, and one of those had her surgery done by a third surgeon. Wow, huh? All of the surgeons have completed fellowships in surgical oncology, one in breast cancer oncology specifically. And they offer all this, as any breast cancer center should!
- Oncology social workers assist patients and their families, through counseling, support, and referrals as appropriate. A social worker is available in the hospital or through an outpatient appointment.
- Nutrition consultation with an oncology-certified registered dietitian to provide education on foods to help with symptom management.
- Pharmacy navigator to review your medications and address medication issues.
- Massage therapy by a certified oncology massage therapist, to help with relaxation, stress management, symptoms and side effects.
- Expressive arts therapy and classes provide activities that promote healing, creativity and community.
- Stress management provides support for coping with the emotional aspects of the cancer experience.
- Cancer groups, education and movement classes for patients and their families. We offer a range of free classes and groups to help you through diagnosis, treatment and recovery of cancer. These provide education, activities and emotional support.
According to her nurse, my PCP said she wants me to use the local surgeon but that, of course, it is my choice.
So, I talked to the local cancer center nurse and agreed to keep the consult and interview the hand surgeon turned breast surgeon. When I go see the BS in Portland, it will cost me another $50 copay for a second opinion, but at least I won't be second guessing myself later. I will be polite and professional, but will probably ask the question that got me an out of network referral from Kaiser 8 years ago: "If your mother were sitting where I am today, would you want her to have surgery here, or be treated by the team at Legacy?" Y'all say a prayer, and I'm not being facetious, that this young lady has a learning experience from being interviewed by Dr. H., which will assist her in the future.
Suzanne
0 -
slh good for you! Keep us posted.
0 -
Well, the doc was personable and answered my questions about the switch honestly. Her radiologist hubby got a job here and she didn't have the network here to get someone in plastics or ortho to back her up and cover her patients, so she did the "bread and butter" general surgery until the primary breast surgeon here got ready to retire. She's done about 50 lumpectomies and 30 mastectomies, including in med school. She also wants to rush the surgery. I have three oral surgery appointments between now and July 26, and she wants to work me in between June 27 and July 11 or to ask the oral surgeon how quickly after the last surgery I''ll be healed enough for the anesthetic. I'm 66, grade 2 and they took out most of the microcalcifications with the vacuum-assisted core biopsy.
My biopsy was absolute hell and I'm wearing a bra 24 hours a day; which lessens but doesn't eliminate shooting pains. Just being back at this hospital reminded me about my 3 previous ER visits and an urgent care visit, and every experience was horrible. I told her I was thinking about Legacy and she encouraged me to get a second opinion there. I can still do radiation locally if I want, and Dr.L wants me to meet one of the ROs before surgery.
So, I'm going to write my PCP through the patient portal and ask her to send the path report and referral to Legacy.
0 -
hi Beesie. Thanks for asking, i have not logged in here in a while. I met with the surgeon on June 27th and he questioned my decision to decline radiation and he asked if the radiologist had given me any recurrence data. When I told him that the RO was concerned about the close margins, he seemed to get offended and stated the margins were clear just not widely clear. He never even suggested a re-excision. I will not be returning.
I’ve decided to go the alternative route and am not going seek any further standard medical care.
0 -
Just wanted to mention did anyone see the post on this site the woman who is 30 years old had INSITU cancer and now few years later its back stage 4.....
BMX...best way to go.
0