Thinking about refusing chemo...anyone else?
I recently had a lumpectomy on June 25 for my IDC. The tumor that was removed for 2.8cm, grade 1 and they were able to get clean margins. They also removed 4 lymph nodes. One of those 4 came back with 4mm of cancer. My original plan was the surgery, then radiation (reconstructive surgery after radiation) and then hormone therapy because my tumor was ER+. This was my base plan because they had already biopsied my lymph node and it came back negative prior to surgery. Now, since there was some lymph node involvement, my oncologist wants me to start with 18 weeks of chemo (1 treatment every 3 weeks for a total of 6 treatments) before starting radiation. That was basically the treatment plan once he input all of my specific criteria. He did not state it, but he seemed to be on the fence about the chemo because of the fact that my tumor was grade 1, slow growing. I told him that I thought I wanted to refuse the chemo and just stick with the radiation and the hormone therapy. He said that I could do a test that would tell me how beneficial chemo would be for my particular case to prevent recurrence and asked me if I would do it first before I made my decision. He was super nice about it and said that it is ultimately my decision and he just wants me to have all of the info available before I make my decision. I said that I would, so I am waiting on those results. Now, I am wishing that I had just stuck with my original statement and got started with the radiation part of this party. Honestly, even if that test comes back with a high score that chemo would be beneficial, I am not sure I am going to do it. I have seen so many women on here that with the same kind of BC as I have that did the surgery, chemo, radiation and hormone therapy and then years later they have a recurrence. I have also seen many with the opposite. But I have also seen many that did not do chemo and they are years down the road cancer free. I just feel like if it is going to come back later, it is going to come back later. I do not feel like chemo will be a deciding factor in that. And if it does come back, I will tackle it all again. I would feel different if I had a current cancer that the only chance to get rid of it was chemo. Then I would do it. I would not like it, but I would do it. But I feel like they got all of the cancer with the surgery and the radiation will hopefully take care of any local cancer cells that could be floating around and the hormone therapy will help against recurrence. I know the chemo could possibly(not guaranteed) help with any cancer cells that may have broke away and are in other areas of my body, but for my current situation, the pros do not seem to way out the cons (all of the possible side effects) to me.
I am sure there are some people here that will not agree with my decision but I feel like it is right for me right now, however, I may feel differently when I get the results of the genomic test he is doing. I guess we will see. My question for everyone is-Is there anyone here that has refused chemo and how do you feel about that decision?
Also, just wanted to say that this forum has really been a blessing to me and I include you all in my prayers everyday! This has been the most mentally exhausting, depressing thing I have ever been through and I know you all must feel the same. Thank you all for being here and helping!
Comments
-
My situation has several differences, but also a few similarities to yours. In case it helps, here is my story:
My lumpectomy removed a tumor that was 2.0 x 1.3 x 1.2 with clear margins and my lymph node did NOT have cancer. I am stage I. My tumor turned out to be a mix of IDC and DCIS (which is sort of like pre-cancer and is stage 0)My surgeon said I was not going to need chemo. The first radiation oncologist I saw said I would not need chemo, but that she couldn't start radiation until the medical oncologist said it was OK. I opted not to go with this radiation oncologist since she didn't do "breath holding" or any other measures to protect my heart. I had also made appointments with radiation and medical oncologists w/ MD Anderson. I went to the first medical oncologist appt and she said I might need chemo and ordered the oncotype test. She said the results would take 2 weeks, but got them in about 10 days. But while I was waiting . . .
I had my second rad onc visit. Before my appointment she had the 77 slides from my surgery "re-read" - the re-reading changed my grade from 2 to 3, found lymphovascular invasion that the first pathology report didn't report and also found one area of DCIS that only had 2 mm clear margins. I really liked her and said I definitely wanted to go with her. She did not think I would need chemo so said she would ask the med onc there (this was before my scheduled appt w/ him) if I could go ahead and start radiation.
So, I was marked up for radiation and ready to start. I met with the medical oncologist the same day as my first radiation treatment. He actually hesitated and considered holding off on radiation, but then said I could go ahead and start and that I could do chemo afterwards if needed.
Then the day of my 3rd radiation treatment, the first med onc calls and says my score is "quite high" and that I needed chemo. I freaked out. It took me several hours to get my actual score / report.
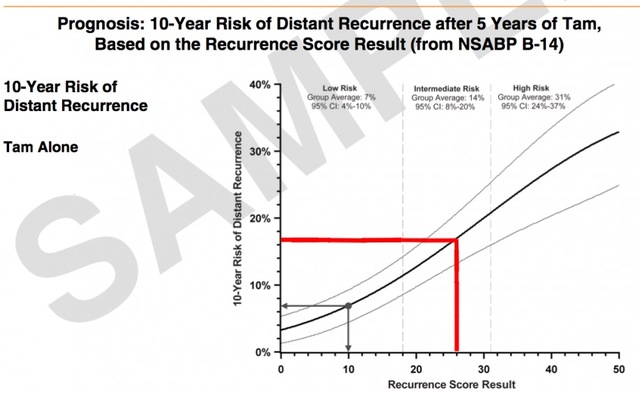
Once I got the report, then came the reading and researching. Turns out that my score is 29 which gives me an 18% chance of distant recurrence if I do the 5 years of hormone therapy. Age matters - under 50 or over 50. I am 61, so over 50. What I wrote to some friends that night was:
RS score is 1 to 100 although I don't think I've heard of anyone having less than 9 or as high as 100. Using this score and age, they figure out chance of getting cancer again if I take the hormone blocker type pills. Using this score, but ignoring age, they figure out how much doing chemo will help (sort of).
For people over age 50, a score of 25 or below has no real benefit to doing chemo. For those under age 50, the benefit for those with a score of 15 & under have no real benefit, those with score of 16 - 20 have 1.6% benefit and those with score of 21 - 25 have 6.5% benefit of doing chemo.
Now the confusing part - the box that says Absolute Chemotherapy Benefit says RS 26 - 100 All Ages and the number is > 15% At first glance, it would appear that there is a 15% reduction (or more) in chance of distant recurrence if I do chemo . . . but . . . reading the "fine print":
On the front it shows that the chemotherapy benefit for scores 0 - 15 is the same no matter the age. Then for scores 16 - 25 the benefit is much greater for patients age 50 and under. I am 61. For scores 26 - 100 they both just say > 15%
Looking at the 2nd page it goes into the two studies and the results of these studies. It says "The magnitude of the absolute benefit of chemotherapy was ~ 6% at RS 26, and increased as the RS results increased from 26-100, with an average absolute benefit of ~ 24% and a conservative estimate of > 15% based on the width of the confidence intervals."
Reading the above, it seems to say that at RS 26, the benefit is 6% and the average of the benefit from RS 26 to RS 100 is 24%. The > 15% on the report is based on the study of all people from 26 - 100 and is NOT the benefit for someone with RS 29. If the benefit increases flat line, then the benefit to me at RS 29 would be about 7 1/2% so my chance of distant recurrence is 18% if I don't do chemo and 10 1/2% if I do chemo.
Also, given that the benefit for those over 50 years is less than the benefit for those 50 or under when the oncotype score is under 26, it would seem that the benefit for those over 50 would also be less for higher oncotype scores which would mean my benefit would be less than 7.5%Sorry the above was so long, but wanted you to see the though process and also know ahead of time that if your score is above 25, the "> 15%" benefit from chemo may or may not be real.
Since then, I've done more reading and research and was able to find a site that had a graph showing approx chance of recurrence with and without chemo for the various oncotype scores. I also found a booklet that said that 26 - 30 might not be advised to do chemo depending on other circumstances.
I did meet with the second med onc again and he does want me to do chemo after I finish radiation. He did say that he understands if I choose not to do radiation. I am 75% through w/ radiation now and only have the 5 boosts left to go. I have until July 26th to decide if I will or will not do chemo.
As of right now, I am planning to skip chemo but will start the hormone therapy and do other things to hopefully reduce my risk of distant recurrence like exercise and maintaining a healthy weight.
0 -
Dorothy-
Thank you for explaining all of that to me! This will definitely come in handy when I get my score back, so I really appreciate it.
That has kind of been my plan as well. Radiation. Hormone therapy. Exercise daily. Estrogen positive "cancer diet". Supplements. Maintaining a healthy weight. Basically, anything I can do on my part to prevent recurrence.
I will more than likely begin radiation soon. If you do not mind me asking, how has that gone? Side effects? Anything that I should be aware of before starting? I am sure I will get a run down from the radiation oncologist before I start, but first hand experience seems to calm me more than just going on what the doctors tell you to expect. While I understand everyone responds differently, I think they like to sugarcoat things to keep us from being so nervous going in.
Once again, thank you for your response. I appreciate you taking the time to talk to me about it!
0 -
I was a bit concerned about side effects after seeing pictures of raw oozing burned skin on facebook, etc. I kept reminding myself that the people who were doing well were out having fun, not posting pictures.
There is a "newish" protocol for some people called "hypofractionated" -
https://www.breastcancer.org/research-news/benefits-seen-with-shorter-radiation-regimen
buried in the article it gives the % occurrence of various side effects using hypofractionated and regular radiation. I qualified for the hypofractionated protocol which is the same total amount of radiation, but more is given at each treatment so there are less total treatments.
If it is your left breast that is involved, be sure to ask what they do to protect your heart. I ruled out the closest, very nice, facility because they didn't do the "breath holding". I've read in the facebook group that some do breath holding using a snorkel like device. Where I am going, they project a picture on the ceiling that includes a rectangle. When I hold my breath, a yellow bar goes up into the rectangle and my goal is to keep the bar in the top half of the rectangle.
The 2 mm margin found on the "re-read" earned me extra boosts and the lymphovascular invasion earned me "whole breast radiation".
Start now practicing lying flat on your bed w/ both arms extended over your head for several minutes at a time. This will stretch out any muscles that need it

After meeting w/ the rad onc, I had an appt for "simulation and mark-up". The table is hard, but covered w/ a towel and they had two things for my knees & lower legs. They offered me a warm blanket to cover the bottom half of my body (left my shorts & shoes on). Once you are in position, you have to stay still for a while (but only about 15 minutes during subsequent treatments). They marked on my with red & blue markers and put clear tape over the marks so they wouldn't was off. The marks are longer than the tape and they will permanently stain whatever you put on (bra for me) after that. Then I got 6 very small tattoos. Only the last was painful and it wasn't worse than getting a shot. Different places do it differently - others have reported that tattoos are around the breast. I have two on my center line and two on each of my sides.
Each visit, I change into my "smock" (sewed for this facility by a local church - velcro front and both sides) and then wait for them to call me. Go in room, lie on table, they open smock so top is totally exposed, cover waist down w/ warm blanket, and have me raise my arms above my head. Then they position me and leave the room.
They can see & hear me and I can hear them when they want me to. They start by asking me to take a breath and hold it and then they do a regular x-ray to be sure everything is ok. Sometimes the bed then moves very slightly and they do it again. Then the actual radiation starts - two short and one longer time of holding my breath until they tell me to breathe. After that they come in, move the bed a bit and the machine moves from above my right side to below my left side so they can "shoot" the other direction. They leave and we do two short and one long again. Then I am done unless they need to remark me if tape is coming off (or gone), etc. Other than stretching of the muscle and sometimes a feeling of pulling closer to nipple from raising arms, I don't usually feel anything during radiation. One time I thought maybe I felt weird feeling during one of the longer ones but didn't happen next time.
I read LOTS of posts on facebook and every time someone posted that they did NOT burn, I wrote down what they did
 I tabulated it all - Glycol Base and Aquaphor and one other that I don't remember were favorites as was 100% aloe vera gel. Most who didn't burn seemed to start moisturizing before, so I started as soon as I knew I was going to do radiation soon. The other thing that those who didn't burn did was drink LOTS of water, so I have been averaging about 10 1/2 cups of water or more each day.
I tabulated it all - Glycol Base and Aquaphor and one other that I don't remember were favorites as was 100% aloe vera gel. Most who didn't burn seemed to start moisturizing before, so I started as soon as I knew I was going to do radiation soon. The other thing that those who didn't burn did was drink LOTS of water, so I have been averaging about 10 1/2 cups of water or more each day.I didn't have anything but aloe vera burn gel and lubriderm, so used those until I got to the store. The rad onc gave me enough sample sizes of Aquaphor for one application each day during treatment and for several days after treatment. She only told me to put some of that on after radiation each day, but I did my own thing . . . It also took me a few days to get the Glycol Base because I had been told it was at CostCo, but wasn't at my CostCo and had to order it from Amazon.
My protocol has mostly been: In the palm of my hand, I mix 100% aloe vera gel (from WalMart) and whatever else I am using in approx equal amounts. I then spread it over the entire area receiving radiation so from under arm to center of body and from a little below collar bone to a few inches below breast. Ask them where radiation will come out or exit through body - some have reported burns on their backs. Mine goes at an angle from center of body to side almost under arm and then the exact opposite, so back hasn't been affected. Not sure how boosts will work yet - will find out tomorrow. Immediately after treatment, before getting dressed, I use aloe vera and a sample tube of aquaphor (bring napkins and maybe water or something to get it off your hands after applying it). Before bed, I use aloe vera and lubriderm. In the morning, I use aloe vera and Glycol Base.
I'm not sure if it is my protocol or just the way things would have been if I only used Aquaphor after each treatment, but after my 15 regular treatments (last one today), I am darker and starting to get a little red but very little discomfort - none of which is skin level discomfort. I only have the 5 boosts left to go.
Side Effects:
dry mouth - this was the first thing I noticed and I drank maybe 13 cups of water the day after the first treatment because my mouth was so dry. I think the dry mouth has continued the entire time but I don't really notice it - I think it is my "new normal" but maybe it isn't as bad. I looked at this as good as it helps me drink a lot of water.
a little bit of fatigue, but still able to do pretty much everything; some days I go back to sleep for an hour or more instead of getting up the first time I wake up. I read that it might get worse during boosts.
on & off nausea - not real bad, sort of like car sick feeling. It comes sometimes on way home from treatment, other times a couple of hours after I eat, other times before I eat. It hasn't stopped me from eating whatever I wanted and I haven't vomited. It was a bit bad on the way home today and continued for a while. I ended up cooking some crescent rolls and eating them and am fine now. I read that it might get worse during boosts.
I have read / been told by rad onc nurse that my radiated breast will end up slightly smaller and perkier than the other side. However as of now, it is HUGE - significantly fuller than my non-radiated breast. Enough that when I asked a friend a little over a week ago, she could see the difference but said that she didn't notice until I asked her to look. I'm guessing swelling will start going down after treatment is over. I've debated getting bra insert for other side, but haven't. I did wear a top w/ patterns to church Sunday so it would be less noticeable.
pain - 1) after 3 days of treatment, I used my riding mower for over an hour. I was fine doing that but woke up at 11 PM with entire breast hurting. Tried putting bra on for compression as well as different position. I debated prescription pain pill, but took one Advil PM instead a little after 1 AM. I was on computer and at 3 AM realized it didn't hurt and went to bed / sleep. I was afraid that this pain was from radiation, but it hasn't happened again. 2) Rad onc warned that I might get "zingers" like little electrical current feeling things - this happened maybe four times overall (seemingly randomly and not during treatments). 3) Sometimes I will feel a very small amount of pain for a little while - enough that I notice it, but not enough to do anything, and then later will realize that I don't feel it any more. 4) last Friday evening my nipple area (I think - had bra on, but around there) was getting occasional sharp pains. I wasn't sure if they would continue but didn't want to have trouble sleeping so took an ibuprofen w/ dinner and that hasn't happened again.
0 -
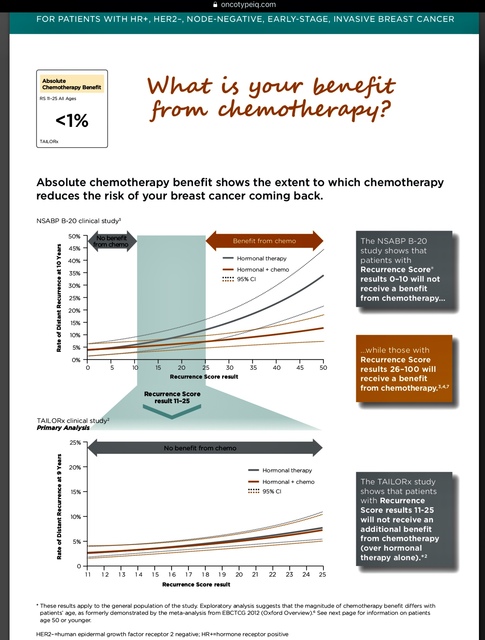
Dorothy & jenni, the problem with the current Oncotype results is they are a combining apples and oranges. Or more specifically, they are using the results from the 2018 TAILORx study for all scores up to 25, and then they are flipping over to the older smaller earlier studies (NSABP B-14 and B-20 and one other I can't remember)for the scores of 26 and higher.
The reason they have to do this is because an arbitrary decision was made in the TAILORx study to evaluate results for a "chemo + hormone therapy" group vs. a "hormone therapy only" group only for Oncotype scores up to 25. The expectation was that somewhere in the range of Oncotype scores in high teens or low 20s, a benefit from chemo would clearly emerge. Therefore everyone in the study who had an Oncotype score of 26 or higher was given chemo in addition to hormone therapy. There was no "hormone therapy only" option for those with a score above 25.
Well, surprise. For patients in the study aged 50 and older, the results showed no benefit to chemo up to and including the Oncotype 25 score. This means that the benefit of chemo kicks in somewhere above this score, but where exactly? That information is not available from the TAILORx study. Therefore what the Oncotype people have done is gone back to using their old data for scores of 26 and higher. The problem is that the recurrence lines from the two studies don't connect. If there is zero benefit to chemo at a 25 score, how can there be a 6% benefit to chemo at a 26 score? And if the metastatic recurrence risk, either with or without chemo, at a 25 score is 7%, how can it jump to 16%-17% without chemo at a 26 score? It does not compute.
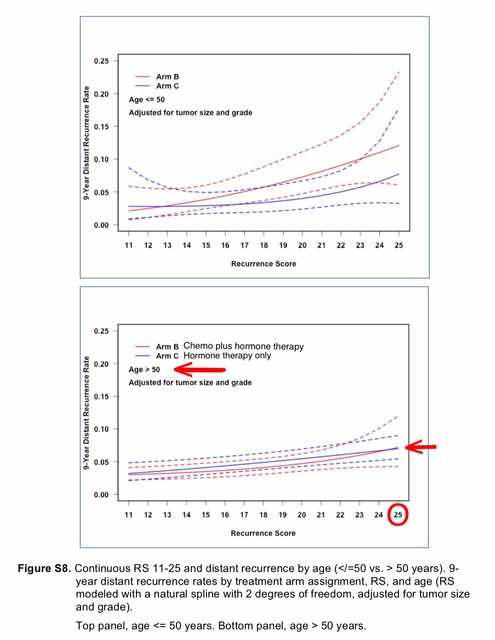
Here are graphs of the results from the two studies. First, TAILORx and second NSABP B-14.
jenni, while the fact that your tumor was grade 1 might help keep your Oncotype score down (grade is not directly counted in the score but genetic elements of the tumor that effect grade are), the fact that your tumor is PR- is going to automatically lean you towards a higher score. PR is a significant factor in the Oncotype calculation, and in the TAILORx study, I believe only 5% of those with PR- tumors ended up with low scores; the rest were divided between intermediate (18-25) and high (26 and higher). Add to that the fact that you had 1 positive node and a 2.8 cm tumor (larger than the average, I believe), and I think you should prepare for a high score. Hopefully that won't be the case, but it's better to be prepared than be shocked, should the result come out higher than you expect.
Edited to correct Oncotype ranges
0 -
Bessie, continuing on with the great information you shared . . .
Please take a look at this https://www.oncotypeiq.com/en-GB/breast-cancer/healthcare-professionals/oncotype-dx-breast-recurrence-score/interpreting-the-results click on Node Positive under "Explain to Your Patients". This opens up a document and I found page 6 of this document to be enlightening. I can't post images here, so can't post it for you to see without having to follow the link.
0 -
Dorothy, that chart on page 6 is a perfect example of the apples and oranges comparison.
The top chart shows a significant difference between the orange (hormone therapy + chemo) and grey (hormone therapy only) lines at a 25 score. But when you shift to the bottom chart (which uses the newer TAILORx results), that difference is gone and suddenly at a 25 score, the orange and grey lines are right on top of each other. Also notice that the grey line, hormone therapy only, represents about a 12%-13% metastatic recurrence risk on the top chart, but only about a 7% metastatic recurrence risk on the bottom chart.
The problem for the Genomic Health people is that with the TAILORx results, while they know more about the 18-25 scores, they now have a huge and obvious gap in information for the 26-31 scores. Those scores used to be "intermediate" but were reclassified as "high" for the TAILORx study. Now the question is whether those scores are really Intermediate, or are they high? Genomic Health are using pretty and complicated charts to hide the inconsistency in the data. But the inconsistency is right there on the page.
1 -
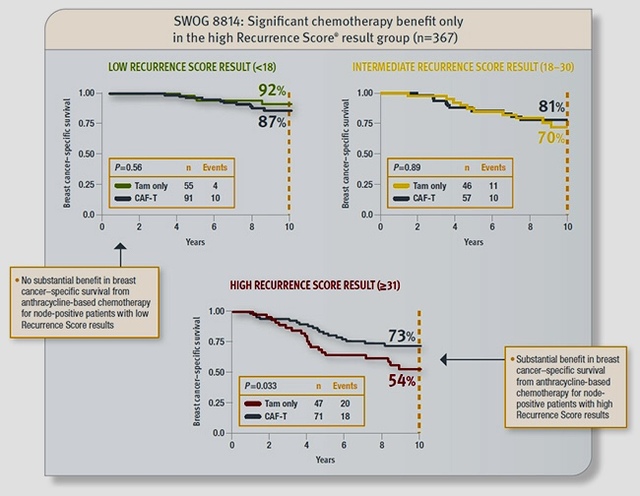
The page says it is the SWOG 8814 clinical study - but the results are similar and show increased benefit as the score gets higher. I found it interesting that chemo actually seemed to have a negative impact for really low onco scores. I wish it went out 10 years.
0 -
Dorothy, sorry, my mistake. I know you are node negative so I was looking at page 6 of the Node Negative report, not the Node Positive report.
This is the page 6 I was referring to from the Node Negative report, which subtly suggests that the data on the bottom chart flows from the top chart, when in fact the numbers are completely disconnected. This is the chart/data that is relevant to you, since you are node negative.
Following is the page you were referring to, from the Node Positive report. Since Jenni is node positive, this is the chart that is relevant to her situation, once she finds out her Oncotype score.
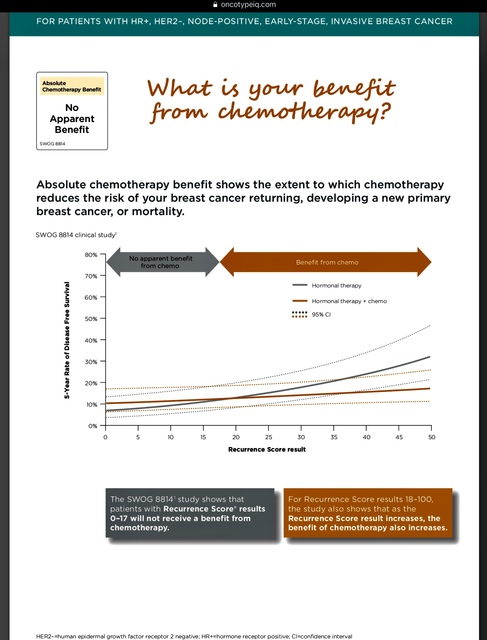
Here is another chart using the SWOG 8814 study that consolidates low, intermediate and high Oncotype scores:
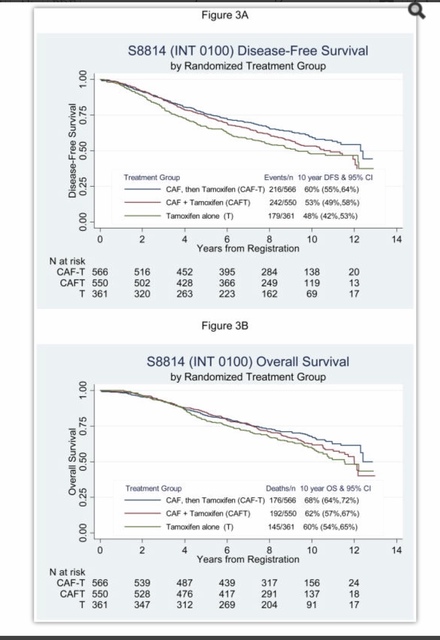
And here is a link to the SWOG 8814 study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3140679/ plus an interesting chart from the study, which doesn't reference Oncotype scores but compares results for the 3 arms of the study:
 0
0 -
Thanks Beesie! I've been looking & looking at info trying to get a good grasp of the chance of distant recurrence for my case. I have seen the bottom chart on the page 6 for negative nodes that you posted, but somehow never saw the top chart. I used the positive node page 6 because I figured my chances were the same or better than that. Unfortunately, I am grade 3 (and the things that made me grade 3 gave me the higher onco score) and have / had lymphovascular invasion even though my node tested clean. This graph doesn't show anything really different from the other research I've done, but it is nice to see something else that agrees
 0
0 -
Dear, I suppose you underwent OncotypeDx genomic test for reaching the conclusion of whether or not to go for chemotherapy. i am yet to begin with my chemotherapy journey but i have a friend (i met her during my visit to oncologist) who underwent this test and her score was 23, so she did not have to worry about the chemotherapy and underwent two rounds of radiations. she is doing well now, but i really cant predict about the status 5 or 10 years down the line. if you have underwent this screening test already then i believe you should patiently wait for the test results and once it is out then you can sit down with your doctor and draft a treatment plan which is most suited for you. I wish you need not to fight this demon again ever. Good luck
0 -
To jenni--nobody here is going to judge your decision. I love your well-thought-out, rational approach. I have no doubt you'll get your testing results back and make the decision that's right for you.
And I have to give yet another shout-out to Beesie. I don't say it often, but you are a tremendous resource for so many women on this forum. I'm so impressed that you always take the time to do the research, post information, and ask key questions. I'd like to think I won't have any more decisions to make, but it's good to know there are smart women out there helping the community if I do.
0 -
Thank you all so much for your help and research that you have posted here. It is going to be really helpful once I get my score back.
Dorothy-Thank you for such a detailed account of your experience so far with radiation. That was exactly everything I was wanting a first hand account of and I appreciate you sharing!
1