Oncotype Recurrence and Distant recurrence scores
Have noticed many have the same Recurrence Score but different Distant Recurrence Scores. Wondering what causes the difference. I requested the raw data from Oncotype DX, hoping for answers and though it was informative, I still wonder what causes different Distant Recurrence percentages. I had assumed the lower the RS, the lower the DS
Comments
-
 0
0 -
Oncotype raw data:
Gene. Single gene score
Bcl2. 9.6
SCUBE2. 8.1
GRB7. 7.1
GSTMI. 7.3
CD68. 8.6
BAG1. 9.4
Cathepsin 12. 4
Stromelysin 3. 11.6
Ki67. 6.6
STK15. 6.1
Cyclin B1. 6
MYBL. 4.8
Beta actin 13.9, GAPDH 11.8, RPLPO 12.9; GUS 4.5, TFRC 7.2 reference genes
0 -
Rebalilly, I sent you this link via PM a couple of weeks ago, in response to the same question. Did you look at my explanation?
Topic: Oncotype DX Reports Interpretation https://community.breastcancer.org/forum/147/topic...
All Oncotype scores are associated with the same recurrence risk estimates for everyone, with two provisions:
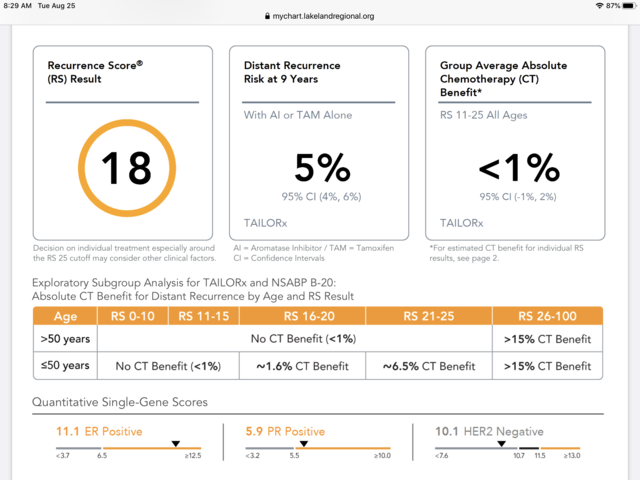
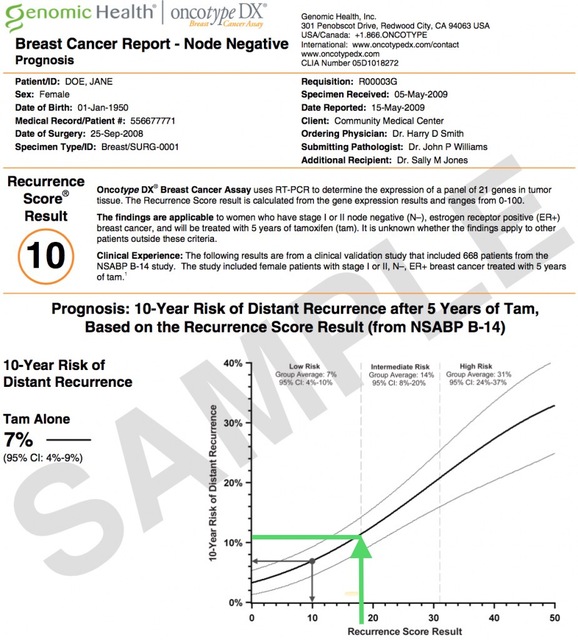
1) Node negative versus node positive - Each have their own Oncotype Score to Recurrence Risk scale. So an Oncotype 18 Node Negative will have a different recurrence risk than an Oncotype 18 Node Positive.
2) For node negative, the Oncotype-to-Recurrence Risk scale changed in late 2018 when the switch was made from using data from previous older studies to using the TAILORx study results. So everyone with an Oncotype score from before late 2018 will have different recurrence risk estimate than everyone with an Oncotype score from late 2018 onwards. In other words, an Oncotype 18 reported in 2017 will have a different recurrence risk than an Oncotype 18 reported in 2020. But all Oncotype 18s will before late 2018 will be the same, and all Oncotype 18s since late 2018 will be the same.
0 -
Hi Bessie,
You are so informative, thank-you. If you had the Oncotype before 2018 is their a way to know what your recurrence risk estimate be?
9/16 LT lumpectomy , 7mm pure mucinous, ER 95%/PR 95%, HER-2 neg, Grade 1, Stage 1, neg noded
Susan
0 -
Susan, here is a sample report reflecting the pre-2018 (pre-TAILORx) results. This report is for a 10 score but looking at the graph, it appears that an 18 score would have equated to an 11% 10-year distant recurrence risk, assuming 5 years of Tamoxifen (I added the green lines to show an 18 score on the graph).
 0
0 -
Hi Bessie,
Thank-you
Susan
0 -
Any chance you have a sample 10 (or similar) score for the post 2018 results? In 2016 my oncotype of 9 translated to a 7% risk but wondering what it would be with the new results
0 -
why does oncotype only talk about nine years? Why not 10? And what happens after nine years? Are we just supposed to follow the line on the chart in my case for a woman over 50? I don't get it.
0 -
Kathy, sorry, I missed seeing your post. Here is a chart from a post-TAILORx report, showing the results for a 10 Oncotype score.
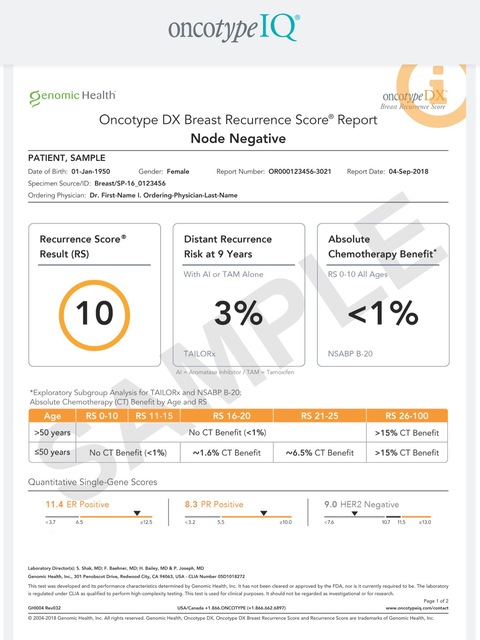
SpringDaisy, the reports indicate 9 years because that was the duration of the research study, or at least the period for which they had the most complete/reliable results. There are other studies that look at longer term recurrence figures, or that provide information on the percent of recurrences that happen during the first 5 or first 10 years post diagnosis vs. longer term. But this information is difficult to come by, simply because of the time and effort involved in following the same patients for such a long period of time.
Here is a graph that shows, for each major subtype of breast cancer, the cumulative incidence of recurrence over time. ER/PR+ / HER2-cancers, the blue line, continue to recur as far out as 20+ years (250 months). But 50% of all recurrences for this subtype happen within 5 1/2 years (65.95 months, as shown in the chart) and if you follow the blue line upwards, it looks like about 80% of recurrences occur by the end of year 9 (108 months).
 0
0 -
Bessie, Thank you for the information. I will find out my number on Tuesday. I have stage 1A and it's the positive, positive receptors and negative HER2. I will be getting radiation and taking an inhibitor I don't know which one. Do you know if the graph accounts for radiation and pills? I am 67. Should I assume I only have years 9 years to live? Actually it looks like it could come back in five years.
Also Bessie I keep reading about stage one if it’s not gone into the lymph nodes or other breast that survival rate forfive years is 99%. And I have read 10 years is 84%. Have you come across these numbers?
0 -
"Should I assume I only have years 9 years to live?"
Oh my goodness, NO!
"Actually it looks like it could come back in five years."
No, you are misunderstanding the chart. The chart is saying that of everyone who will have a recurrence, 50% will have the recurrence within the first 5 years, and the other 50% will have the recurrence after year 5. What the chart also shows is that approx. 80% of those who have a recurrence will have it within 9 years after diagnosis. What the chart does not show is what percent of patients will have a recurrence. That figure depends on the specific diagnosis. As for your question about treatment, while the chart doesn't specify the treatment, I think it's fair to assume that patients have had the recommended treatment, whatever that might be (it will be different depending on the diagnosis).
You will be getting an Oncotype score. Take a look at the Oncotype chart in my previous post. That chart shows the recurrence risk for someone who has a 10 score on the Oncotype test. The metastatic recurrence risk at 9 years is 3%. Then, taking the information from the second chart that shows that for ER/PR+ / HER2- cancers, approximately 80% of all recurrences happen within the first 9 years, this means that in the period beyond 9 years, i.e. past what the Oncotype chart is showing, this patient has less than 1% additional risk. So a patient with a 10 Oncotype score has a lifetime risk of recurrence of only about 4%, with 3% risk over the first 9 years and 1% risk after that. I don't know what your Oncotype score will be or what your risk will be, but with a Stage IA cancer, the odds that you will pass away of something other than breast cancer - hopefully peacefully in your bed when you are very old - is extremely high.
As for the node negative survival rates of 99% at 5 years and 84% at 10 years, yes, I have seen figures similar to that. But the 84% is an average of all patients who are node negative - some may have very aggressive cancers. Your risk is based on your pathology, not some average of everyone. The Oncotype test will provide the risk figures that are specific to you.
0 -
Bessie, thank you so much. I will find out my score on Tuesday so I will write back to you then. You are a lot more knowledgeable than I am. So if you don't mind maybe you can do my math for me!
0 -
I heard back from my doctor regarding the oncotype Calculator. When I got my score I was a bit surprised it had a 12% nine year distant recurrence. Then people on this page, Bessie for one, told me about a Calculator! doctors can use for women over 50 to lower that score because of my age 67. So he told me today, my 12% went down to 7% with a 95 confidence interval of 5 to 10%. So that makes me feel better. I am starting radiation Monday. I kind of forgot what the 5 to 10% means though. If they have a 95% confidence level than what is the 5 to 10% for?
0 -
Springdaisy, that's great news!!
The "95 confidence interval of 5 to 10%" means that there is a 95% certainty that your recurrence risk falls between 5% and 10%.
So while the average risk for someone with your Oncotype score and your age/tumor size/tumor grade is 7%, the range of results is 5% and 10%, with 95% of patients (with your pathology/stats) falling into this range.
0 -
thank you Bessie. Iused to be better at these math problems! But it is good.
0 -
I also have an oncotype score of 18, for mucinous breast cancer, 2.5cm, hormone positive, her neg, no lymph nodes but I am 40... Chances of them recommending chemo are ....????
0 -
Glevitan, the thing is that Oncotype was validated with mostly IDC patients, so we really don't know just how accurate it is for other subtypes, do we? So if you have ILC or mucinous, in my opinion your oncologist should pay a little more attention to clinical factors like lymph node status and Ki67 and not rely just on Oncotype. Age 40 and 2.5 cm I would lean toward more aggressive treatment, whatever that would be for your subtype. Probably ovarian suppression added to tamoxifen or OS + AI because it seems that the benefit of chemo for ER+ premenopausal women in their 40s with scores in your range is probably in its induction of menopause. (Verify what I say with your onc.) See the TAILORx trial results.
0 -
Thank you, yes I'm very borderline for everything as ki25% but lymph node negative... Also regarding tumour size in mucinous carcinoma the actual real tumour size is usually smaller than the measured size as it is pumped up with mucin cells. I guess I will find our soon enough from the oncologist anyway.
0
