Bottle o Tamoxifen
Comments
-
lynae, Although it could have been expected that I would be on an AI, my BS gave me information to make a decision. I chose Tamoxifen because I have a 10+ year history of osteopenia (currently stabilized) and did not want to chance the bone leeching from an AI. Yes, there are side effects from the T-- sometimes hard to tell the source of the brain fog but I do find it harder to concentrate than before, have to watch the constipation issue, and don't really know if joint aches and stiffness are due more to meds or the weather. That said, it is my understanding that AIs have an even worse reputation than Tamoxifen for causing joint pain...
Best wishes in Your decision making!
0 -
Lynae23,
I am post menopausal and I am currently on tamoxifen and happy so far. Except for the brain fog. I've lost weight, I don't ache, and don't have mood swings.
I've been on ALL the other AIs and was to the point of quitting altogether until my MO suggested tamoxifen. Each had its own set of side effects, but the pain, especially in my legs at night, sleep issues, mood swinfs, depression, and horrible dryness everywhere all were more than I wanted to have to tolerate for 5 years... or 10.
Beaverntx, does tamoxifen cause constipation?? I've been so plugged up, I got out the Metamucil. I have IBS and a history of C Diff, so I try to keep everything on an even keel. I stepped up my probiotics, which isn't helping.
0 -
Nancy, constipation was one of the first side effects I noticed and seems to be a problem that crops up regularly. This is entirely new. Hooray tamoxifen.
0 -
Salamandra, you are in the minority. Most breast lumps found are found by the women themselves. Not their doctors. If a woman feels that her doctor's exam, and him finding nothing, is the all clear, those women are putting themselves at risk. Know thyself! (or at least thy boobs). A woman's first best defense is herself.
0 -
lynae23,
Glad you are well.
I had a partial hysterectomy (still have my cervix, ovaries, fallopian tubes) in 2014, so it didn't make me menopausal (not even close,). I had uterine fibroids so my uterus had to go, after several other failed treatments. Chemo pushed me toward meno (or almost...not quite as of May). I am getting tested this week to see where things stand hormonally because my MO will switch me to an AI as soon as we are sure that I am menopausal. I am doing well on Tamoxifen--having gotten past constipation, dehydration-related leg cramps, sleep and other issues, So changing drugs is not what I really want to do BUT, my tumor was aggressive with high recurrence risk--depsite being node negative-- I want the best chance at keeping bc at bay. I remember that you were at MD Anderson too? I was just there for my mammo on my native breast, bone density scan and echocardiogram (both in anticipation of switching to an AI), before meeting with my MO. The labs on my Estradiol etc. have not come back yet, so I don't yet know if I will make the switch now or later. We need to be sure, otherwise the AI would backfire on me if I am not actually menopausal--actually increasing recurrence risk! I am most worried about the potential bone/joint pain because I teach! However, I going to give it a try as soon as I know that I am menopausal. If it doesn't work for me, there's always Tamoxifen to go back to (or other AIs).
0 -
My lump was found on the mammogram, and thankfully. It was less than 2 cm and towards the chest cavity on the left side in April of 2018. My gyno did not find the lump shortly before my mammogram nor did I. I am so grateful that is was found early on since it seemed like in a difficult position to find it on a breast exam. Since I have dense breasts I get the 3D images and not the regular mammogram.
0 -
Nancy, try magnesium for constipation. I find that taking it at night I am regular in the morning. Metamucil just adds so much fiber to your system, sometimes it is too much to take and can almost bind you up instead of relieving you. I don't think probiotics will help with constipation.
0 -
Lomlin, thanks for the reminder. I have a liquid calcium and magnesium combined supplement I have been forgetting to take!
0 -
Nancy, the anti-constipation key for me has been lots of walking (goal of 12,000 steps a day), 2.5 to 3 liters of fluids daily and 2 servings of dried fruit each day--found no sugar added dried figs and dried mangoes at Costco. The dried fruit counts as part of my servings of vegs and fruits daily. Trying to not add any more pills or supplements to what I'm already taking!
0 -
I took a bit of a medication holiday for a couple weeks (it wasn't really planned it was just more that I just couldn't bring myself to think about taking them for a while) and just started taking everything again this past Friday. Well let me tell you, it was HELL for the first couple of days, massive muscle cramps in various places (feet, toes, calves, thighs, right/left side of my chest ... worst was when it was on my right side and went to my spine, could NOT move and screaming in pain on the couch!). Today it's not as bad, still cramps if I move a certain way, it'll now give me a warning cramp to move back to the way I was or else! I see my MO next week, will be three years now on T and they're saying 7 more years. If it weren't for these damn cramps I'd say I don't have any issue with the T, my neurologist says my brain fog is probably from a chronic B-12 deficiency which has now been corrected (that and I'm an Alzheimers med once a day which does seem to be helping).
Nancy - the magnesium really helps with the constipation, I just have it with the rest of the meds I take and have had no issues with constipation at all.
0 -
Beaverntx, I don't exercise enough... I'm lucky if I get 5000 steps a day. I don't drink enough water either. If I drank 3 liters I'd be in the bathroom all day! Lol! I have dates in the fridge that I forget about too. I really need to get back on a healthier track.
0 -
Oh and *curses the brain fog or something* my mood since getting back on the T have been horrible. DH has been almost ready to divorce me a couple of times and part of me can't blame him since I've really been difficult. Even though it's only been a couple of days I can go from happy go lucky to I'll cut you and smile while I do it. Luckily, he's been very understanding, knowing that it's part of the transition back to having these hormones in my system that it had grown accustomed to not being there for a couple of weeks.
0 -
Ah the brain fog! I’ve been off T for a month and it’s like the clouds have parted! Also, my sore joints and muscles are so much better. I see my MO Monday - not looking forward to it
0 -
Beaver, those Costco dried mangoes are the best! We love them.
0 -
Interesting studies I found regarding Tamoxifen efficacy/overall survival related to premeno women & BMI (body mass index).
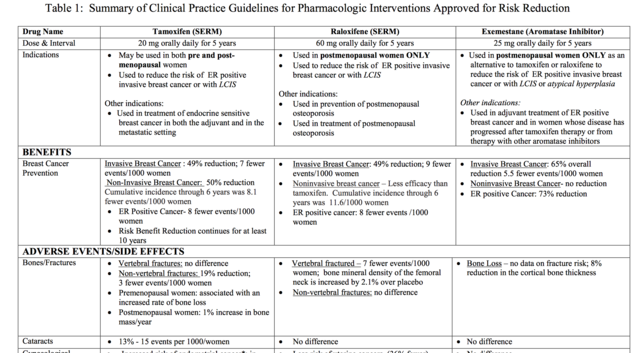
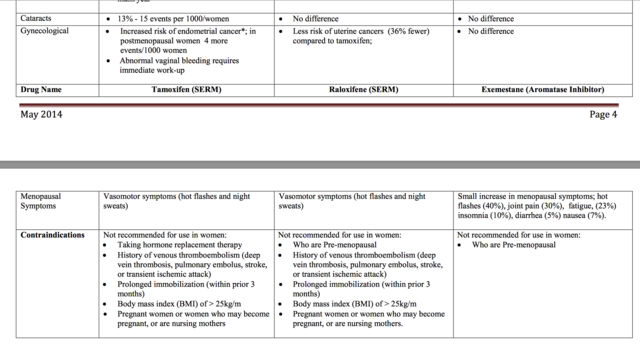
See table below -- under "contraindicated" for BMI > 25 kg/m
My MO never mentioned this, and though I am not obese, I am overweight and this is something I will be asking her about when I see her in 2 weeks.
--------
Effect of body mass index on the efficacy of adjuvant tamoxifen in premenopausal patients
2014
https://www.ncbi.nlm.nih.gov/pubmed/27061527
RESULTS:
In both normal weight and overweight patients, the baseline clinicopathologic properties and the treatment history with radiotherapy and chemotherapy were similar and no statistical significant difference could be detected. Tamoxifen in combination with luteinizing hormone-releasing hormone (LHRH) agonist was used in 33% (136/408) of the patients in Arm A and in 22% (91/418) of patients in Arm B (p<0.001). Three-year disease free survival (DFS) rates were 89% and 87% in arm A and arm B, respectively (p=0.39). Three-year overall survival (OS) rates were 99% in arm A and 94% in arm B which appeared to be of significance (p=0.028). In univariate analysis no statistical significant effect of LHRH agonist usage on DFS (p=0.58) and OS (p=0.96) was found.
CONCLUSION:
Although BMI had no negative effect on recurrence risk, poor OS (overall survival) was observed in overweight and obese premenopausal breast cancer patients with hormone-receptor positive tumors who were treated with tamoxifen.
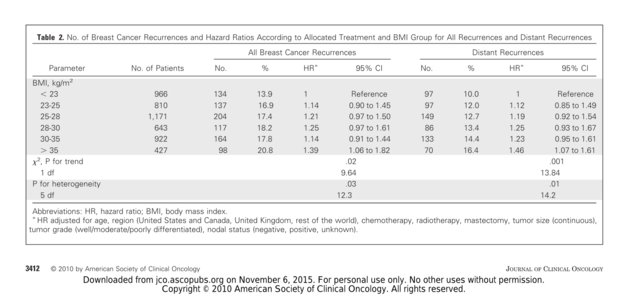
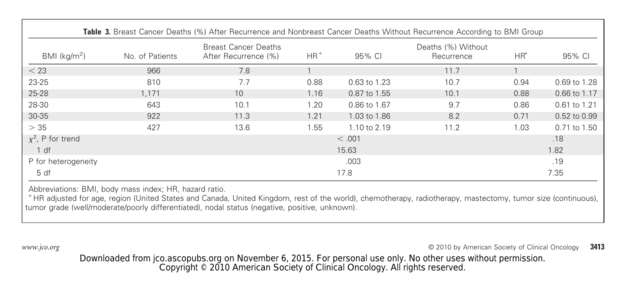
--------Effect of body mass index on recurrences in tamoxifen and anastrozole treated women
2010
https://www.ncbi.nlm.nih.gov/pubmed/20547990
Results: Overall, women with a high BMI (BMI > 35 kg/m(2)) at baseline had more recurrences than those women with a low BMI (BMI < 23 kg/m(2); adjusted hazard ratio [HR], 1.39; 95% CI, 1.06 to 1.82; P(heterogeneity) = .03) and significantly more distant recurrences (adjusted HR, 1.46; 95% CI, 1.07 to 1.61; P(heterogeneity) = .01). Overall, the relative benefit of anastrozole versus tamoxifen was nonsignificantly better in thin women compared to overweight women.
CONCLUSION:
These results confirm the poorer prognosis of obese women with early-stage breast cancer. Recurrence rates were lower for anastrozole than tamoxifen for all BMI quintiles. Our results suggest that the relative efficacy of anastrozole compared to tamoxifen is greater in thin postmenopausal women and higher doses or more complete inhibitors might be more effective in overweight women, but this requires independent confirmation.
-------
The predictive impact of body mass index on the efficacy of extended adjuvant endocrine treatment
https://www.nature.com/articles/bjc2013367
2013
Results:
In all, 634 patients (177 normal weight, 307 overweight, and 150 obese) patients were included in this analysis. Normal weight patients with additional 3 years of anastrozole halved their risk of disease recurrence (disease-free survival (DFS) HR 0.48; P=0.02) and death (HR 0.45; P=0.06) and had only a fifth of the risk of distant metastases (HR 0.22; P=0.05) compared with normal weight patients without any further treatment. In contrast, overweight+obese patients derived no benefit from additional 3 years of anastrozole (DFS HR 0.93; P=0.68; distant recurrence-free survival HR 0.91; P=0.78; and OS HR 0.9; P=0.68). The possible predictive impact of BMI on extended endocrine treatment could be strengthened by a Cox regression interaction model between BMI and treatment (P=0.07).
Conclusion:
Body mass index may be used to predict outcome benefit of extended AI treatment in patients with receptor-positive breast cancer.
0 -
Spoonie, that is very interesting I am bookmarking to ask my medical oncologist about it at my next visit (in a few months).
0 -
Yes, that is troubling because I am certain I am in that higher BMI group.
0 -
Ok yall, gonna double post this because I think this is so very important, as we all have different medical histories and we all need to be our own best advocates.
Hugs and healing....
--------
I'd been struggling with my decision to take Tamoxifen. I'd vowed to give it a shot, but now, it's off the table completely. I've been doing research on my various chronic illnesses, namely Chronic Late Stage Neurological Lyme Disease and multiple co-infections (Bartonella, Babesia, and Ehrlichiosis) and the contraindications of Tamoxifen.
Thankfully I was my own advocate because I found some very troubling things that apply specifically to my own medical history and since I know it's complex I can't blame my MO or Onc Team. They specialize in cancer, not in Lyme. But I'm disappointed that my Infectious Disease team did not point this out.
Anyway long story as short as possible....(just in case others with Lyme Disease or other immunocompromised peeps stumble upon this at some time):
According to this study, The Effects of Tamoxifen on Immunity https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902982/#R19
Tamoxifen is an IMMUNE MODULATOR (aka an immune system suppressant variant) resulting in lowered lab values such as CD4, CD57 (natural killer cells), Auto-Antibody productions (ANA, RF, etc), B-Lymphocytes,TNF-alpha, TGF-beta, and more.
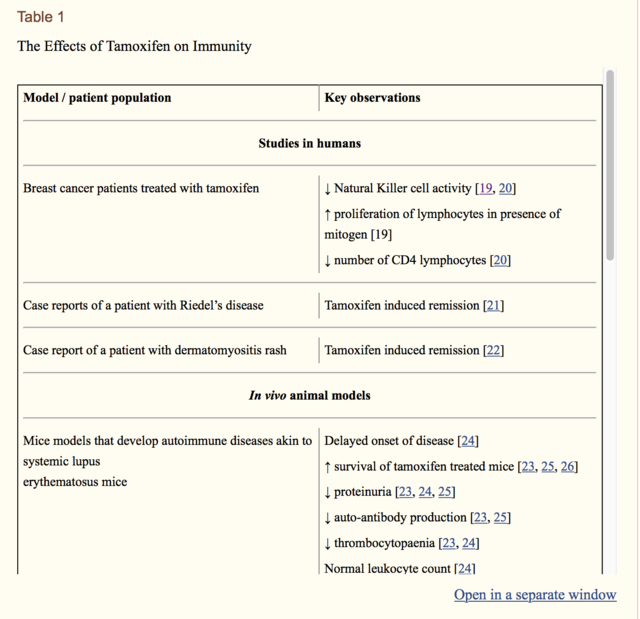
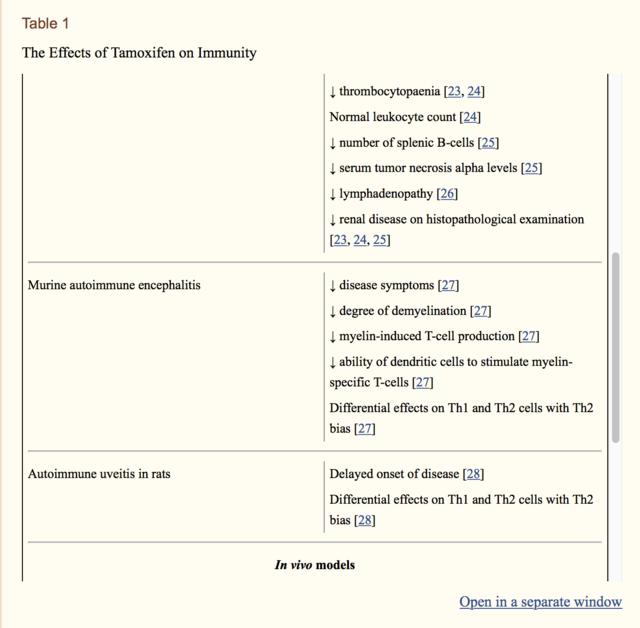
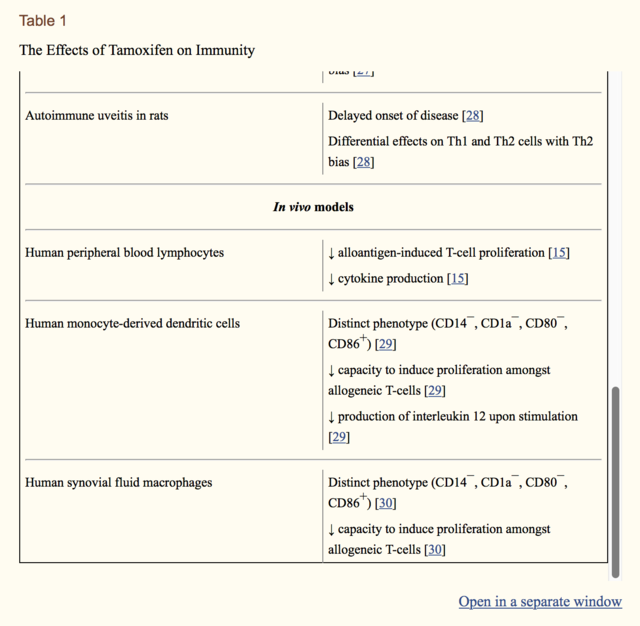
All of these are tests that my Infectious Disease team regularly monitor, because years ago they were basically non-existant levels....and yet....no one mentioned the dangers of my taking Tamoxifen and how it would affect my primary disease and my immune systems ability to fight these multiple chronic infections. Uggh.
----------
Immunomodulatory effects of anti-estrogenic drugs
2012
"Tamoxifen, which functions as a competitive partial agonist-inhibitor of estrogen at its receptor, has been widely used for more than three decades for adjuvant endocrine treatment in breast cancer. Currently, other effective drugs for endocrine therapy include raloxifene, different aromatase inhibitors (particularly third-generation agents) and luteinizing hormone-releasing hormone agonists. In recent years, a growing body of evidence suggests that these drugs can also act as immune modulators by altering the function of various leukocytes and the release of different cytokines. Moreover, there is evidence that anti-estrogens may prove to be beneficial in the treatment or prevention of some autoimmune diseases due to their effects on immune function."
https://www.deepdyve.com/lp/de-gruyter/immunomodulatory-effects-of-anti-estrogenic-drugs-tyQYutFafl
"Inter- estingly, various anti-estrogenic drugs have also been demonstrated to affect the immune system. The immunomodulatory effects described thus far include alterations in the fun- ction of lymphocytes, macrophages, monocytes and dendritic cells as well as effects on cytokines. Additionally, anti-estrogenic drugs have exhibited some immune modulations related to autoimmune disorders, possibly leading to other uses."
-----------
There is ABSOLUTELY no way I will take Tamoxifen knowing this.
For some people with Psorasis, SLE, MS, etc, and other auto-immune disorders this would be a help I'd imagine since it would settle their immune system down a bit and keep it from over-attacking their bodies.
However, for me, that would be a nail in the coffin as I need mine to fight as hard as it can, every day.
I will take this report and other reports/labs to my MO to show her how this will impact me in a huge way.
I know that Tamoxifen "may" reduce my risk of recurrence or future BC by 40-50%, but I CURRENTLY fight and treat these diseases every single day of my life. If I let these run rampant I will die...not if but just a question of when.
At one point in my life, about 10 years ago, when Lyme was wreaking havoc in my system and no one would treat me, I couldn't walk due to muscle weakness, bedbound 24-7, was losing the physical ability to talk, short term memory was non-existent, was sufferring myocarditis which nearly put my heart out of commission, pain was off the charts, QOL non-existent, and much more. My brain was sufferring deterioration and inflammation that was similar (words on my MRI's and was wrongly dxed with MS) to that seen in Demylenation Disease, showing damage in multiple areas of the white matter and progressing.
I have worked soooooo hard to get some semblance of a life back and my labs in range, no way I will risk throwing that away for a "maybe".
Soooo yeah...Tamoxifen is a no for me and basically.
IMO, should be off the table for any that are immunocompromised or battling chronic, life-altering system-wide infections. Not a doctor obviously, but wow, just another piece of the pie that shows we HAVE to be our ADVOCATe, no one else will do it for us.
Do your homework everyone. It is so critical.
0 -
Ok, according to the CDC, regarding getting live vaccines, those on immunosuppressive drugs (look at picture, last line...tamoxifen is noted....although stated it is LESS immunosuppressive than others...still considered immunosuppresive), should wait 3 months before getting a vaccine after stopping said drug, and waiting at least a month before restarting the drug after being vacinated.
I'm sure my MO never mentioned this to me....SMH.
If the CDC considers being on Tamoxifen to be immunosuppressive, that seems like something our teams should be informing us of.
I posted quite a few other studies that link Tamoxifen to various affects to the immune system, if anyone would like to read them they are here. https://community.breastcancer.org/forum/78/topics/868242?page=2#idx_56
Immunocompromised Travelers
Duration of Iatrogenic Immune Compromise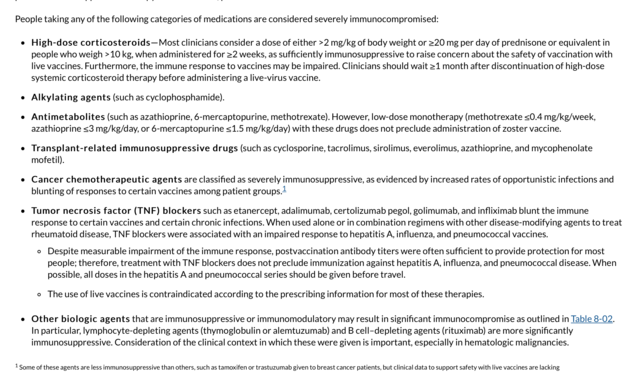
"The period of time clinicians should wait after discontinuation of immunosuppressive therapies before administering a live vaccine is not consistent across all live vaccines. For cancer chemotherapy, radiation therapy, and highly immunosuppressive medications (exclusive of lymphocyte-depleting agents and organ transplant rejection prophylaxis), the waiting period is 3 months. For lymphocyte-depleting (alemtuzumab and rituximab) agents, the waiting period is ≥6 months, although many experts believe the waiting period should be ≥1 year. For steroid regimens considered immunosuppressive (see above), wait 1 month. Zoster vaccine is exceptional and may be given 1 month after any highly immunosuppressive agent, although many experts advocate waiting ≥1 year for anti– B cell antibodies and other lymphocyte-depleting agents. For agents not considered highly immunosuppressive (see Table 8-02), consultation with the prescribing clinician (and possibly a hospital pharmacist) is recommended to manage individual patients and estimate degree of immunosuppression. No basis exists for interpreting laboratory studies of immune parameters to evaluate vaccine safety or efficacy. Restarting immunosuppression after live vaccination has not been studied, but some experts would recommend waiting at least 1 month."
0 -
Are there many live vaccines that people still get? I'm on the waitlist with my GP for Shingrix, but that's not a live vaccine. And my flu shot wasn't live, either. I was more concerned during chemo than I am about tamoxifen.
I'm sorry for your Lyme disease difficulties and illness complications, Spoonie.
0 -
Excellent post, Spoonie!
0 -
I'm not a physician, but if Tamoxifen is an immunosuppressant, then it has very little of that effect in me. Not only am I taking Tamoxifen but also Xeljanz for my alopecia areata. --a well-known immunosuppressant that was developed for rheumatoid arthritis. I just took a full set of blood labs and show no signs being immuno-compromised. In fact, my numbers looked so strong that I am wondering whether I need to increase the Xeljanz dose in order to get the drug to work!
0 -
Runor -- Thank you!

PrincessButtercup -- I'm not sure about live vaccinations. I haven't been able to get a vaccine for years due to my immune system stats. ETA, I did Goggle live vaccines and apparently there are still quite a few, including the nasal flu vaccine.
CDC https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/prinvac.pdf"Currently available live attenuated viral vaccines are measles, mumps, rubella, vaccinia, varicella, zoster/Shingles (which contains the same virus as varicella vaccine but in much higher amount), yellow fever, rotavirus, and influenza (intranasal). Oral polio vaccine is a live viral vaccine but is no longer available in the United States. Live attenuated bacterial vaccines are bacille Calmette-Guérin (BCG—not currently available in the US) and oral typhoid vaccine."
I mainly added that post from the CDC in order to demonstrate that if the CDC has posted it that should be an additional big flag to patients that there is indeed a significant factor seen on our immune systems (even if we do not feel it or see it thru symptoms) with Tamoxifen.
And I totally agree, that others like ScrafGal and for yourself, had sound reasons to be less concerned over Tamoxifen.
Everyone is so very different, coming into the cancer dx and afterwards, not to mention genetics and other factors. Chemo wasn't an option for me, so Tamoxifen was supposed to be my treatment course. My QOL was poor coming into this new "world". Maybe others have great QOL and haven't dealt with years of chronic, life disabling issues. That's wonderful and I'm grateful that others have that experience.
I just wanted others to have the chance to be informed, since it seems drs don't bring this factor up to their patients, and IMHO that's not a fair presentation, especially to those that have multiple health issues on board.
ScrafGal -- Tamoxifen is an IMMUNE MODULATOR (aka an immune system suppressant variant) demonstrated in multiple studies since the 1990 to lower lab values such as CD4, CD57 (natural killer cells), Auto-Antibody productions (ANA, RF, etc), B-Lymphocytes,TNF-alpha, TGF-beta, and more. These labs are not run on a typical CBC or blood count, to my knowledge. They are very specific labs to measure the activity of an immune system. I understand that you have RA and are on meds for that, so am I as I have Sero-Neg RA, but even so, my Rheum dr doesn't run these tests (that are lowered by Tamoxifen) when he runs my labs. He only ran the RF ANA and such when I was dxed and every so often afterwards. Maybe this is different for you. I'm very glad you don't feel any SEs due to the immune aspect of Tamoxifen. That's good news.

----------
Below are screenshots from my thread, and the other studies/info that demonstrate the effect Tamoxifen has on the immune system.
There's also whole book on it....
Tamoxifen: Beyond The AntiEstrogen
I won't paste all the tables of info that are in this book, but if immunity and immune response due to your medical history is of any major daily concern, then I would bring this up to your ONCO team for a discussion.



 0
0 -
Cross posting here:
Lower-Dose Tamoxifen Reduces Recurrence Risk, Toxicity Incidence in Breast Cancer The use of low-dose tamoxifen was shown to significantly reduce the risk of new and recurrent disease following surgery in women diagnosed with breast intraepithelial neoplasia but it did not cause more serious adverse events compared with placebo.
0 -
I think that we all have to weigh the pros and cons of tamoxifen for our own situations. I'm finding the side effects to be challenging, and there are days when I look at that bottle of pills and have to force myself to open it. I also think that we don't go from surgery/chemo/radiation to feeling normal in just a few months. I'm back at work but definitely still struggling. But I'm taking the tamoxifen because the risk of recurrence without it is too scary for me. I'm not worried about getting vaccines, since neither of the ones I needed/will need this fall (flu and Shingrix) are live. And since I have asthma, I always get the flu vaccine. I've had the flu before, and don't wish to repeat that!Hoping today is a better one for everyone.
0 -
You're exactly right PrincessButtercup - we all need to way our own circumstances vs the information at hand and risks and make the decision that's best for us and that will give us peace going forward. Wishing you the best on your journey.
 0
0 -
Fellow asthmatic here! Got my flu shot 1 month post chemo for the same reason...the last time that I had the flue, about 15 years ago, I literally thought that I might die...Never again!
0 -
Spoonie, I'm sorry you have so many health conditions to balance -- it can be hard when one med has side effects that affect the other!
Re: the flu vaccine, as mentioned above it is not a live vaccine. The article Spoonie posted was referring only to live vaccines from my reading. Most flu vaccines used (aside from nasal spray) are not live. . https://www.cdc.gov/flu/about/qa/misconceptions.ht...
Hope everyone remains flu-free this winter! We all already have enough to deal with! :-)
0 -
I am asthmatic and only had the flu shot once in 2009, never again. Too many chemicals in the body, need to limit them, my choice no shot. Thankfully have not gotten the flu. I really don't like taking pills, and on top of that I don't like taking pills to band aide side effects from pills.
0 -
I met with my MO today. I’ve been off Tamoxifen for 5 weeks and feel better than I have in over a year. Chemo did indeed put me in menopause - haven’t had a period in 15 months. She did say it could come back.
She said my options were going to an AI, which would include bloodwork every three months. She said SEs could be joint pain, but guaranteed my hot flashes would get worse and that concerned her, because they are bad now.
She said my other option was to not take anything. She stressed my tumor was small, low grade and because of my TN tumor I had the big guns chemo and radiation.
We went over my recurrence risk and I’ve decided to not take anything. She supported my decision wholeheartedly, saying QOL is so very important and I was having a very hard time. She obviously said if I change my mind to get in touch
I feel so relieved to have made a decision. This is right for me.
0