Afinitor/Aromasin
Comments
-
I feel as though it was a very specific variety of Greek yogurt, maybe Stoneman or Stonehill or something like that. I think it had Stone in the name!
0 -
Joyner, I don't remember a specific brand of yogurt, but Chobani seems to work for me. If you find out, I can try it too.
0 -
I PM'ed Pat McG to ask the question. Will let you all know.
0 -
Hi All. I wanted to pass on the report from my latest scan especially as it is good news. I have not heard directly from my oncologist yet, but if I read it correctly everything has improved. The three tumors in my spine have resolved and the ones in my liver have improved and most are not clearly apparent on the current exam. The others in nodes, etc., have also improved. There are some new suspicions in my lungs but the tech reports it is probably inflammation. It looks like A/A is working for me for now.
1 -
WONDERFUL NEWS, IntoLight! Happy Thanksgiving!!
0 -
It was Stonyfield Greek yogurt that Pat McG recommended. She swore by it for mouth sores. It is entirely possible that one brand is no better than the other, but I thought it was interesting that she was always very specific and what was working for her.
0 -
I just found Stonyfield Greek yogurt yogurt on both the Walmart and Target websites. It is apparently generally available in local stores.
0 -
Hi All. Apparently the suspicious inflammation in my lungs was the beginning of pneumonia which I found out last night after spending four hours in the ER. My onc called yesterday with her suspicions and told me to go in if I got a fever. At 8:00 I spiked a 102* fever so I went in. I understand it is all part of the SEs of A/A. I am better today. I am thankful my onc cared enough to call me ahead of time. Her simple remark on the rest of the PET scan was "the meds are taking care of the cancer."
0 -
IntoLight - congratulations on the scan results! So glad it is working!!! 🎉🎉🎉 so sorry about the pneumonia but great your MO is so proactive and you are already feeling better. What did they do for you in the ER? Any thoughts on how it came on? Just your body's reaction to the drug or something in addition to spark it? I think when I got the breakout of mouth sores I was a bit rundown and had too many glasses of wine the night before! 😳
Thank you Lynn! Will check out that brand of yogurt! Would be much better than the Dexamethasone if it works! I did start the Dexamethasone and in 3 days mouth sores were gone. Just on time to enjoy a lovely Thanksgiving meal.
 . Now have dropped to using it 2ce per day and seems to be working.
. Now have dropped to using it 2ce per day and seems to be working.Also have been using the L-Glutamine and it does help my throat. I kind of fell off the 3x per day and noticed a tinny taste in my mouth. Made sure I did the 3x per day and that tin seems to be going away!
On another note, I am I Hawaii with my parents, brother and his girlfriend. Beautiful, warm sunshine!!!!
 0
0 -
Perky, Hawaii sounds wonderful right now! So glad you are getting a handle on the mouth sores. I am keeping them under control but had a cold sore break out and it just won't behave.
No one knows how I got the pneumonia. The ER called it a "community acquired pneumonia" which is what they say when you don't catch it in the hospital. But we caught it so quick it didn't have a chance to develop much. I am feeling better from that but today I hurt from the Zometa infusion. Usually that is no big deal for me but it hit me hard this time. Even with the nurse being so kind and giving me a slow drip. I guess I shouldn't skip the Claritan the day before, but I am on so many meds right now I didn't want to add to them. When I checked into the ER, the check-in nurse said "sepsis alert" and they immediately took me back bypassing many people sitting in the waiting room. Part of it I think was because somehow I bypassed the Covid screening when the lady monitoring the door said to just go right in. The ER doc ran blood tests, took a chest x-ray and immediately started me on two IV antibiotics. They also did an EKG as my pulse was way high. Of course I had a Covid test which came back negative. I was put into a separate room instead of just a curtained partition. It is an older hospital but I get good care there and everyone is friendly and very helpful. My nurse and doctor were amazing and attentive. I have no complaints.
0 -
Well, I was back at the ER yesterday. Same symptoms but add a little chest tightness and increase the cough. The ER doc ruled out a PE and pneumonia, and other stuff like Covid and the flu. What he is thinking now is it could be the Affinitor, but there is no real way to tell. I am waiting on a call from my oncologist to try to figure out what to do. I was told to go off the meds for a few days. The tricky part is we are moving from California to Colorado January 7th. I may have to wait for a new oncology team to determine next steps as I will have to change Medicare plans. Ughh... Anyone else develop any lung issues?
0 -
IntoLight - so sorry it came back! I understand compromised lungs is a common side effect. Hope your MO has some ideas and you find a good team in CO!! Second opinions are always good!! I found a great group on FB for people living with metastatic breast cancer just in Seattle. They have been great for references to providers. Maybe there is one in CO?
I definitely feel my lungs more compromised with Afinitor. The first few days on it, I had a persistent cough. Now as time goes by, I can feel them tightening and harder to get full breaths. I do a breathing meditation practice and Qigong method for the organs. First scan and follow up with my primary Onc this week. Crossing my fingers it doesn't get worse for my lungs.
0 -
Hello to all. I just started on A/A today. I was on Xeloda for about 22 months previously. I only had Mets to liver and breast before November 2021. Now I have progression in my lower spine which I hope to have radiated to ease the back pain. I have the prescription steroid mouthwash and plan to use it as recommended. It's always unnerving to start a new line of treatment and posts about A/A seem a bit frightening. With the exception of the initial IV chemo I did 4.5 years ago, my treatments/SE's have been very manageable. Big thanks to all those who are posting on this thread.
I wish you all a peaceful and joyful Holiday Season0 -
kc54321- I was on a afinitor for about 10 months and did very well on that. I did use the mouthwash four times a day for eight weeks and didn’t have a problem with mouth sores so I would definitely recommend that. I did have some swelling in my feet occasional scalp sores but my counts were a lot better than on the Ibrance and my hair was a lot thicker and the leg cramps and neuropathy were better some people have some issues with their blood sugar and with their cholesterol.
I hope you get a good long run on it.
0 -
Kc54321,
I will start Afinitor/Aromasin first week in January 2022.
I lasted 4 months on reduced Taxol due to toxic effects.
Diagnosed liver mets 10/2016:
Adriamycin/cytoxan NEAD
Ibrance/Letrozole PROGRESSION
Xeloda PROGRESSION
Taxol TOXIC SIDE EFFECTS
Aromasin/Afinitor
0 -
I spent five days in the hospital with lung issues and came home Sunday night. The best diagnosis is pneumonitis from the Afinitor. I am up and can walk to the baathroom by myself now. My oncologist has kept me on the Aromisin for now since I respond well to anti-hormonals. More later...
0 -
SandiBeach, I didn't want to scare you since we have totally different reactions to drugs. I had four years on Ibrance, one year on Xeloda, and started A/A in September. I have no idea where I am headed next since we are waiting for me to recover right now. We are planning on moving out of state once I recover so I will have a new oncology team and situation. In the meantime everyone is taking good care of me and I am feeling stronger all the time. I am on oxygen but feel like I should be able to wean off it fairly quickly as I feel improvement already.
0 -
Sandi and IntoLight, I feel as though we've been in the trenches together for a while. Sandi, good luck with A/A, and please post your reactions. I may be following you shortly. I had a cutaneous (skin) metastasis a couple of weeks ago, so I'm likely to be leaving Xeloda after 35 months. I'm doing a telehealth meeting with my onc today to discuss options....what a Christmas present.
Sending love to you both. Good luck, Sandi, and get well, Into Light!!
Lynn
xoxox
0 -
Lynn,
So sorry to hear that you may be leaving xeloda. Aren't skin metastases your sort of "signature" that a treatment could be failing for you? I'm curious -- why can't they just remove the skin metastasis and/or treat it with radiation rather than move on to another systemic treatment?
I hope you and you MO can work something out.
0 -
Nkb and Sandibeach - thank you for your posts. I’m only on day 4 of A/A and so far so good. I know it’s early but I’m keeping up hope that I can squeeze out at least 6 months on this line. Fingers crossed!
IntoLight- I’m sorry to hear about your recent hospital stay. I hope you feel better very soon. Thank you for sharing your experience.
Take care everyone.
~Kc
0 -
Bev...you must have a memory like a steel trap! Yes, just after Ibrance/Faslodex stopped working for me in late 2019, I was put on Xeloda. Within a week or so, a cutaneous metastasis (shown to be lymphatic) showed up on my scalp/upper forehead. It was excised by my dermatologist, but Xeloda seemed to finish it off. Nothing more heard of that one. My onc said at the time that since I was, and am so far, bones only, the skin met was a good way of determining that my current regimen had stopped working. He noted that tracking progression in bones only is so difficult.
Xeloda worked for 35 months, and this latest cutaneous metastasis (single lymphatic lesion, as before) is a sign that I need to change treatment. The final biopsy reports that the lesion is 100% estrogen positive, rather than the triple negative the first tiny sample was reported, in error we believe, to be. My Richmond onc (an excellent general oncologist) recommends that I move to AA next, but we'll wait to get the recommendation from "on high" from my breast cancer specialist at MSK.
I am to have a teleconference with her on 1/6. I'm so relieved by the receptor status of this recent lesion!! Also, my local onc says that she has had many BC patients who continued to do well after a skin metastasis, unlike what is reported online (2 weeks to 50 months survival, with a median of 5 months!!).
Merry Christmas and peace to all-
--Lynn
0 -
Lynn,
Don't know about that steel trap, but certain things just stick with me.
You didn't respond to whether or not radiation would help? Did you discuss that one before with your previous skin metastasis?
So happy that the lesion is estrogen positive. That is good news.
Good luck on the teleconference with your MSK doc. Merry Christmas to you, and everyone else on this thread who celebrates. And peace to us all.
0 -
Lynn - so sorry about the skin lesions and I do hope that local treatment can be used and you can continue Xeloda. It is nice that you still have an oral treatment as an option and hopefully will hold you until some of these treatments than seem really close to approval are available.
Are you Her2 low ? You can look at the path of your original biopsy - about 50% of people are and that may open some possibility of ADCs like Enhertu.
Let us know the thinking of your MSK MO.
Hope you are having a lovely holiday.
0 -
Bev and Nkb, I apologize for the long delay in response. I took some mental time off over the holidays but have been busy with BC issues, anyway.
I had a PET scan Tuesday, and the results weren't too bad. I had feared visceral metastasis, but so far, still bone only (except for the cutaneous mets and a periclavicular node a year or so ago). Increased FDG uptake/avid focus in left clavicle, and I'll see where that goes. Maybe spot radiation there??
Re skin mets questions:
Nkb, my receptor status has always shown 0 HER2. My original path report from 1991 cannot be found. I developed MBC 26 years after my initial diagnosis. All I have it my memory that I was ER+, PR- and if checked then, HER2-. However, per a Foundation One test in 1/19, I have the ERBB2 S310F genetic alteration, and my local onc has always noted that Herceptin might be worth trying when running out of other options.
Bev, regarding radiation for the skin mets, at least for the one in 2019, that was not discussed. The path report said that it was lymphatic in source, and all docs involved said that removal had "cured" that particular lesion. I don't believe that MSK expressed an opinion on that.
I'm waiting to talk with MSK at 11 this AM to get her recommendation, which I will surely follow. I'm going to ask if the fact that Xeloda has kept this bone-only for 3 years, except for that lymph node and the skin mets, might mean that I could safely remain on Xeloda, perhaps even with the addition of something else, until the next progression. I read somewhere online about Xeloda with Letrozole being used when skin met appeared.
We shall see. I hope that you two and all others had a nice holiday-
Thank you!
0 -
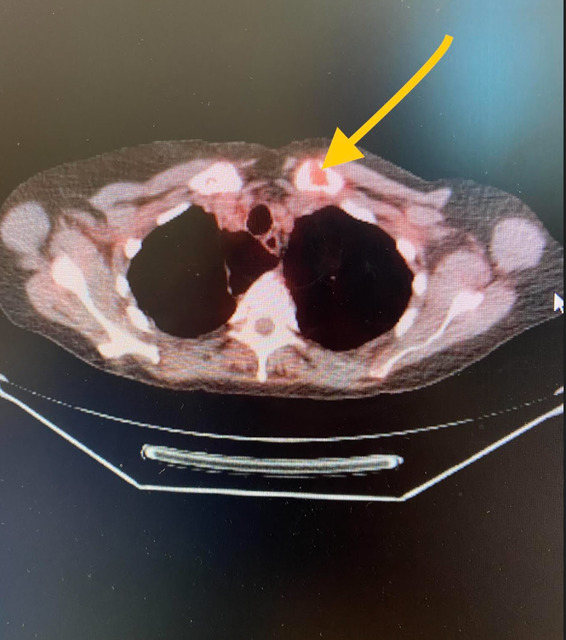
I emailed my RO at Sarah Cannon here in VA (she reads PET scans herself and had a degree in Chemical Engineering before becoming a doctor. She is affiliated with the hospital where the PET was done and thus has access), and she said this:
"The spot is actually where your collar bond meets the breast bone. We could definitely treat there since it's really the only area of active disease".
She sent me this graphic from the PET. Encouraging.
 alt="" style="width: 442px; height: 498.959px;">0
alt="" style="width: 442px; height: 498.959px;">0 -
Lynn,
I'll be curious to know what MSK says.
Your graphic did not come through.
Re your mutation, I have the exact same ERRB2 mutation. I am currently on xeloda and neratinib. I don't think that neratinib is that widely used (trade name: nerlynx) but you could ask your docs about it and see what they say. As of my last scan, that combo was holding things stable. I've talked with my doc about other HER2+ drugs, and she dances around it, but she bought into the neratinib for whatever reason.
Hope this helps.
Bev
0 -
Thanks, Bev. Will ask! Trying the graphic again. I was trying to use a .pdf.
 0
0 -
Joyner- great picture! I am glad that they can radiate that one place and perhaps you can stay on Xeloda longer. Will be interested to hear what MSK says.
I am getting a PET next week and am very nervous since my Tms are inching up. I have no more oral treatment options per my MO. I did have a spot on my R hip radiated 6 months ago and it resolved it. there were a few tiny spots on L hip last PET, but, low grade - if that is all they see maybe I can have more spot radiation.
0 -
Nkb, my meeting with MSK was essentially very positive: she said that my PET was essentially unchanged and that the uptake in the clavicle was relatively minimal (SUV 3.2 to 3.9). I have shoulder pain, which I believe to be a rotator cuff issue, and she said to see my orthopedist to confirm that and to be sure not referred pain from the clavicle spot near my breastbone. If referred pain, we'd do spot radiation for the pain but otherwise she said no need to chase that down. Ultimately we agreed that I would stay on Xeloda, which she noted had done a great job of keeping me bone only for 3 years....hooray! We are to be very vigilant and do PETs every 3 mo, which I do anyway. She expects that any change would be increased activity in my bones first rather than a jump to a visceral organ. We'd make a change to AA if we see an uptick in bone activity.
Let us know about your PET next week. My tms had been up some, too, and I forgot to ask about that. BUT, the scan didn't show trouble. Hoping yours won't, either!
0 -
great news Lynn
0