Will 30% of Early Stage (1-IIIA) go on to metastasize??
Comments
-
VLH, I usually get all my reports before the doc does.
0 -
Yikes! Another good reason to be your own advocate and ask questions
0 -
This should be encouraging for node negative, low oncotype Dx scores http://www.practiceupdate.com/C/43073/56/1/1?elsca1=emc_enews_topic-alert
Here's the text
BACKGROUND
A 21-gene expression assay (Oncotype DX recurrence score [RS]) that uses reverse transcriptase-polymerase chain reaction is used clinically in patients with early-stage, estrogen receptor (ER)-positive, human epidermal growth factor receptor 2 (HER2)-negative breast carcinoma (ER+/HER2- BC) to determine both prognosis with tamoxifen therapy and the usefulness of adding adjuvant chemotherapy. Use of the assay is associated with reductions in overall chemotherapy use. The current study examined the treatments and outcomes in patients with low RS.
METHODS
The authors reviewed the institutional database to identify patients with lymph node-negative, ER+/HER2- BC who were treated at the study institution between September 2008 and August 2013 and their 21-gene RS results.
RESULTS
A total of 1406 consecutive patients with lymph node-negative ER+/HER2- BC and a low RS were identified (510 patients had an RS of 0-10 and 896 patients had an RS of 11-17). The median age at the time of diagnosis of BC was 56 years; 63 patients (4%) were aged <40 years. Overall, 1361 patients (97%) received endocrine therapy and 170 patients (12%) received chemotherapy. The median follow-up was 46 months. Six patients (0.4%) developed distant metastases (1 patient with an RS of 5 and 5 patients with an RS of 11-17). In the cohorts of patients with an RS of 11 to 17, the absolute rate of distant metastasis among patients aged <40 years was 7.1% (3 of 42 patients) versus 0.2% among patients aged ≥40 years (2 of 854 patients).
CONCLUSIONS
The data from the current study document a 0.4% rate of distant metastasis within 5 years of BC diagnosis among patients with lymph node-negative ER+/HER2- BC with an RS <18. Patients aged <40 years at the time of BC diagnosis were observed to have a higher rate of distant metastases. Analysis of data from other studies is necessary to validate this observation further.
0 -
Molly, that link isn't working?
As for the big announcement today... The new Mammaprint study was just released. it's great news and confirms many women are being overtreated with chemo and mammaprint helps find those who don't need chemo. I personally can attest to this as I was a gray area Oncotype score (20), age 41, and grade 2 tumor. I did the mammaprint as a second opinion and 'Low risk!" yeah.
0 -
I still find this discussion fascinating and am glad it's continuing. That is encouraging news Molly50...but again, I always find it meaningless that they are touting these great statistics of not metastasizing at the FIVE year mark. It would be a lot more meaningful (IMHO) if it was 20, 30 + year mark. But I also know that information is not out there for them to give us. So I still believe that it's more of a crap shoot than they want you to believe. But it doesn't get me down.
 I'm grateful to be here and live my life with BC in the rearview mirror. I am just more vigilant, as one that has been diagnosed with BC, about keeping up on research, making healthy choices, being in tune with my body and advocating for myself with the medical community.
I'm grateful to be here and live my life with BC in the rearview mirror. I am just more vigilant, as one that has been diagnosed with BC, about keeping up on research, making healthy choices, being in tune with my body and advocating for myself with the medical community. Approaching the 6 year mark and am done with active treatment. The BCI test showed I was at a 6% chance of recurring (which is considered "high risk") and that I should continue hormone therapy for the full 10 and I decided against it. No regrets. If the % was a lot higher maybe I'd have made a different choice? I'm hoping an active healthy lifestyle helps my odds instead of popping more pills. And if I lose the bet, I'm still okay with my decision to stop. Odds are in my favor.
 0
0 -
6 percent is high risk? My oncotype of 9 gave me a 7 percent risk and my doctors all say I am low risk. I know the BCI is a different test but how is that score low risk
0 -
what is the bci test.
0 -
so after reading all of these posts it's almost sounds like stage IV is in the future for many. Are there certain kinds stages or other pathology that makes you more of a candidate
0 -
The BCI test is the Breast Cancer Index test by Biotheranostics and it is a genetic assay conducted on one's original tumor sample when you have reached the five year point of taking anti-hormonals. The purpose of this dual result test is to help predict both recurrence risk and effectiveness of anti-hormonal meds beyond five years. A BCI index score of 5 or below is a low risk, from 5-10 is higher risk. The scoring is independent of score types in other genetic assay tests. A score of 6 is just above the cut of between high and low risk. My result was an 8, so definitely in the high risk category, but the benefit from anti-hormonal drugs was scored low. My MO has asked me to continue on Femara as long as I can tolerate it because while the benefit is low, it is not zero and I have not recurred yet and have been a compliant user of AI drugs. I have either been lucky so far or they are providing some degree of benefit for me.
0 -
Wow, ThinkingPositve, that comment is not exactly thinking positive.
Reading this whole thread - including the many many posts that refute the subject line (NO! It is NOT TRUE that 30% of Stage I go to metastasize), my conclusion is that Stage I women reading this (this thread is in the Stage I forum, after all) should be reassured that most of them will not go on to become Stage IV.
Yes, of course some women initially diagnosed as Stage I will develop a metastatic recurrence, but the figure for Stage I is well below the 30%. The 30% figure includes all early stage invasive breast cancer, which means Stage I, all of Stage II and Stage IIIA (although some sites consider IIIA to be advanced rather than early stage).
The problem of course is that there is unfortunately no way to know who will metastasize and who won't, so it's important that all Stage I women remain vigilant and see their doctor about any lumps or unusual pains or any symptom that might be indicative of a localized or metastatic recurrence.
As for who is at the greatest risk of a metastatic recurrence, there are many criteria that suggest a higher (or lower) risk. Oncotype score... HER2 status... Nodal involvement... Size of tumor... Grade of tumor... Etc.
I encourage everyone to remember that this is a thread in the Stage I forum with a subject line that no doubt attracts many newly diagnosed Stage I women. Although the 30% stat has been explained and clarified many times over these 38 pages of posts, someone new to the thread might only read the most recent posts. So let's please be careful in what we say so as to not leave a frighteningly wrong impression.
0 -
I fixed the link. Lisey, that is great news!
0 -
I know, Susan. I wish it was longer than 5 and it doesn't apply to me because I was node positive. I too want to achieve the point of BC being in my rearview mirror. Hard to do when I am still seeing my MO every 4 months, my surgeon every 3 and waiting on recon.
0 -
The Oncotype DX test measures the risk of distance recurrence within 10 years of diagnosis.
0 -
From PracticeUpdate.com
Published in Oncology and
Rate of Distant Metastases in Women With Breast Carcinoma and an Oncotype DX Recurrence Score <18
TAKE-HOME MESSAGE
- This was a single-center, retrospective study. The authors assessed the rate of development of distant metastases in 1406 women with early-stage ER-positive, HER2-negative breast cancer who had low recurrence scores on Oncotype DX testing. Overall, 1361 patients (97%) received endocrine therapy and 170 patients (12%) received chemotherapy. Only 6 patients (0.4%) developed distant metastases over a median follow-up of 46 months. The absolute rate of distant metastases among patients aged <40 years was 7.1% (3 of 42 patients) versus 0.2% among patients aged ≥40 years.
- The rate of distant metastases over 5 years in women with early-stage ER+/HER2− breast cancer and low recurrence scores is 0.4%, although younger women have a higher rate of distant metastases.– Jeremy Jones, MD
0 -
The reason the study didn’t follow DFS for a longer interval than 5 years is that OncotypeDX has been used almost universally for only a few years now--I think it was introduced less than 10 yrs. ago and considered “experimental” by insurers for a time after that (and some national health systems such as Australia & NZ don’t cover it, and Canada’s system covers it in only selected situations--a number of Canadian women here have has to go out-of-pocket for the test, which is about $4500 USD). Expect 10-year retrospective study results in a couple of years--right now, 5 years is about as far as they can reliably ascertain. (IIRC, OncotypeDX’s RS figures may have been based on retrospective data of women who did get the test, which had not been standard-of-care for its first few years, and are mainly statistical and not case-specific).
0 -
Bessie. Sorry I sounded that way but at times it's very hard to think positive. With my stats I worry and I guess I am at more risk than others. I wonder about all things that I was told "don't focus on this don't focus on that. No Oncotpye because it probably will come back high". But wasn't that what I did chemo for? Plus I look at this topic being for stage 1 and I am stage 2 so I immediately think things are worse for stage 2. There are days when I think I am going to be fine and it will not come back. But then a few days later I think different. I guess I should be thankful i am currently ok
0 -
thanks Beesie...I was just about to cry..I am debating chemo with an onco type of 20 but with LVI...trying to decide in this intermediate gray zone is hard! My MO even said the LVI gave him pause!
0 -
Lmencken, are you going to get the mammaprint? You'd be a perfect candidate.
0 -
Whatever the percentage chances of individual recurrance, some people will worry more than others. And since alternating hope and fear is part and parcel of this disease for many, developing mental survival skills is the key to leading a normal life with bc
0 -
Lisey, it looks like good news for many women including yourself avoiding chemotherapy
0 -
lisey..no idea..should I ask? Would that help with my decision?
0 -
>>Whatever the percentage chances of individual recurrance, some people will worry more than others. And since alternating hope and fear is part and parcel of this disease for many, developing mental survival skills is the key to leading a normal life with bc<<
Spot-on, Traveltext! Our cancer centers offer us all sorts of complementary mind-body therapies and programs, but no instruction in mental crisis-survival skills in general. That needs to change.
0 -
I'm stage IIB and I don't worry about this. I pay my oncologist to do that. I'm posting my infamous speeches. I think they are needed right about now:
SEAT BELTS:
You don't assume you will get into a car accident every time you get in your car. You do put on your seat belt and drive carefully. Same with breast cancer. Eat right, maintain a healthy weight, exercise, and take your hormone therapy (if prescribed). No reason to think you are going to get mets until you actually have a symptom.SHIT HAPPENS:
Some people win the lottery and become millionaires too but do you really think that's going to happen to you? Shit happens. Sometimes good shit, sometimes bad shit, but most of the time shit doesn't happen. Don't assume shit is going to happen to you.WHAT IF'S
Remember the word "if" is in the middle of the word "life" for a reason. As long as you have life you will always have "what ifs". It's your MO's job to worry about those cancer "What Ifs"BTW I still haven't won the lottery
0 -
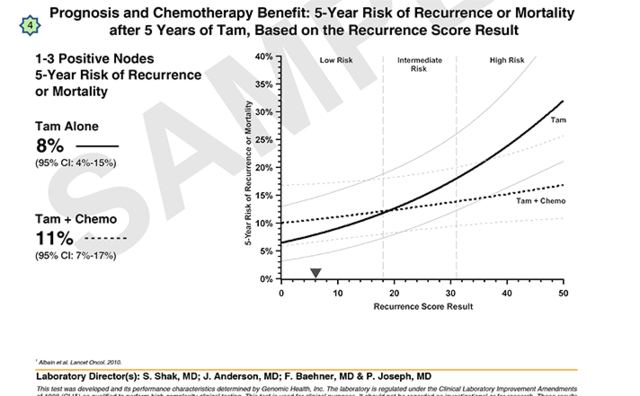
I just wanted to point out a key difference between the type of recurrence risks included in the node-negative ("N0") versus node-positive (1-3 positive nodes) Oncotype reports.
The nature of the recurrence risk estimates provided by OncotypeDX for invasive disease differ depending on whether it is a node-negative report or a node-positive report. This is because the validation studies used to establish the relationship between recurrence risk and Recurrence Score were completely different studies, the study follow-up periods were different and the clinical endpoints for recurrence were different.
===> Specifically, both graphs in the node-negative report provide "10-year risk of distant recurrence after 5-yrs tamoxifen."
This is 10-yr risk or suffering a distant recurrence (incurable metastatic disease).
===> In contrast, the graph in the node-positive report provides a "5-Year Risk of Recurrence or Mortality after 5 years of tamoxifen'"
This is a 5-yr risk of recurrence or mortality, and appears to include both local and distant breast-cancer recurrences, new primary breast cancer, or death due to any cause, whichever came first.
Sample Node-Positive (1 - 3 N+) report: http://breast-cancer.oncotypedx.com/en-US/Professional-Invasive/Ordering/ReadingTheReports/Node-Positive1-3Report.aspx
"Clinical Experience: The following results are from a clinical validation study that included 367 patients from the SWOG 8814 study. The study included post-menopausal patients with N+, ER+ breast cancer who were randomized to either tam alone or CAF chemotherapy followed by tam (CAF-T). The endpoint for this study was disease-free survival (time to local or distant recurrence, new primary breast cancer, or death from any cause) and 5-year risks are presented. (1)"
I am a layperson with no medical training. Patients who received a node-positive report should verify this against the content of their personal report and discuss the nature of the 5-year recurrence risk provided with their medical oncologist to ensure receipt of accurate, case-specific expert advice.
BarredOwl
0 -
KBeee..can I ask what your onco type was? Why did you do chemo?
0 -
lago, love your post!!! Thank you all for the great posts!!!
0 -
Am I reading this right? In the sample report there is higher risk of recurrence WITH chemo (11%) versus no chemo (8%)?
0 -
Yes, Cubbieblue, for the reasons Barred Owl stated above. They’re talking apples & oranges. The OncotypeDX graphs for node-negative patients measure estimated 10-year mets-free survival risk for patients getting either tamoxifen alone or tamoxifen+chemo. The ODX graphs for node-positive patients measure estimated 5-year recurrence (not distinguishing between local & mets) and survival risk (mortality from all causes, even getting hit by a bus), period, for patients getting either tamoxifen + tamoxifen+chemo. I think the difference is due to ODX only relatively recently being used for node-positive (1-3 nodes) patients, and that node-positive patients may a bit sicker in general (statistically insignificant, IMHO), be less able to tolerate any life-threatening risks of chemo (or may be likelier to have other health problems that might kill them independently of cancer). Notice that even with the lowest score there isn’t that much of a difference between chemo+tam and tam alone--about 2%. BUT notice even this slightly paradoxical result diminishes the closer to 20 you get, and disappears (the graph lines cross) at ODX scores above 20--starting there, the survival benefit from adding chemo becomes more dramatic the higher the score, just as with node-negative patients.
Why they measure only 10-year mets risk for us node-negatives, rather than disease-free survival, recurrence of any kind, and "mortality from all causes" risks at 5 & 10 years, is beyond me. But I’m not even an amateur scientist.
0 -
Hi cubbieblue:
On page 37 of this thread, jojo9999 asked a similar question about the lines crossing over in the lower range on the graph, and I answered her in great detail. (I suspect no one read it).
The short answer is:
Please note the additional lines on the graph reproduced above from the node-positive report are "confidence intervals."
I would caution people against possible over-interpretation of the cross-over in lines on the graph on the node-positive OncotypeDX report. This graph is based on the results of one particular validation study conducted in node-positive patients. Overall (not broken out by specific nodal status), there were 146 patients with a "Low risk" Recurrence Scores (RS < 18), including 55who had received tamoxifen alone and 91 who had received the CAF-T regimen (chemotherapy, followed by tamoxifen). As explained below, there was a low event rate, and large confidence intervals in the Low risk group, so there are some limitations inherent in these results. Very roughly, a confidence interval is a type of statistical indicator of the reliability of an estimate.
For a detailed discussion, with reference to the interpretation of results from the published validation study, see my complete reply here:
https://community.breastcancer.org/forum/108/topics/812929?page=37#post_4784284
BarredOwl
0