If 93% survival rate at 5 yrs - why do the 7% perish?
Comments
-
Voraciousreader - Did the dx of "mucinous carcinoma" appear on your final path report? I have never heard of that sub-type, and see that it may require a second opinion to catch.
0 -
Divecat - The cartoon you posted sadly sums up the "learning curve" that one faces after the diagnosis is made . . . . Tailored treatment for the myriad of BC sub-types is needed, and they cannot get there fast enough as far as I am concerned.
0 -
wendy....yes and yes. Mucinous BC is very rare and frequently requires further pathology investigation to confirm diagnosis.
0 -
I was just thinking about this recently because I was bothered by the status quo that so many of our measurements during cancer treatments are done by sampling.
We sample some lymph nodes to draw reasonable conclusion but not factual conclusion. The judgement is helped with imaging the area but imaging technology has limitations. We sample some parts of the breast tissue for final pathology report. This step focuses more on the suspicious/biopsied areas. The whole breast tissue is not made into slides/examined. Some patient might have a tiny coexisting breast cancer with worse prognosis hidden and this second locus is not found out by the lab. She might receive a "lighter" or not entirely targeted treatment plan as a result. If there are already circulating tumor cells, she might find out years down the road that despite the double mx and chemo, she has mets that are a completely different subtype (ER status etc).
0 -
I agree KayB -
It's disheartening to think we may have mets at diagnosis because no surveillance is done... we wait until we're symptomatic.
I was told no surveillance because outcomes are the same.
0 -
Jilly59,
I understand that, in a way, it is disheartening to think that one could have mets without knowing, but imaging (the primary means of surveillance) is not without risk due to radiation exposure. I say this as someone whose met (yes, singular) was discovered 6 weeks after a IIB dx, during an unrelated PET scan. I fully understand that knowing my met is there, before it ever became symptomatic, will not change the outcome. I will simply know about it, and live with that knowledge, for a longer period of time. BTW, my onc is so concerned about radiation exposure, even at stage IV, that I am now going to annual PET scans, unless symptoms develop. It all seems rather counter intuitive, and from my perch, rather surreal.
0 -
in the not too distant future, blood tests will be able to discover recurrences. They are already recognizing progression of metastatic disease before imaging finds it. While still in its experimental stage, blood tests will become the primary diagnostic tool, usurping imaging...
0 -
"in the not too distant future, blood tests will be able to discover recurrences."
That will be good. Are circulating tumour DNA (ctDNA) tests readily available to determine metastatic progression now?
0 -
My niece was dx with eye cancer 2 years ago. She had clear scans but some sort of blood test she had done showed that it had indeed metastasized. She had two options: Wait and see where it shows up or do chemo.
There is testing that exists.
I am not a fan of radiation. I was fearful of mammo's and had my first at age 54 (all clear)...one year later I had IDC that I discovered myself.
0 -
travel...Blood tests that identify progression were recently discovered by Sloan Kettering but are not yet available. That said, Sloan Kettering is among the many places that are excited about "liquid gold," which refers to blood biopsies. Hopefully soon, blood marker tests will be extremely reliable and will be used for the masses. Recently, when I visited the Rare Breast Cancer Lab at Sloan, the researchers themselves have been stunned not only by their own discoveries that are happening at a quicker pace, but are also enthusiastic regarding the discoveries of other researchers at other locations.....
0 -
I talked to my MO recently about these newer tests that capture circulating tumor cells in the blood amongst other things. She said they don't know yet what to do about this information - clinically speaking. Let's say you are being monitored by these tests and they show increase in circulating tumor cells. Your level of anxiety will go up. If you are already on anti-hormonal pill there isn't much else they can do, right?
0 -
muska..thanks for that bit of excellent logic.
If, like me (and you) cancer has made it to the nodes, who knows where else it may or may not have made it to? So, best just let the anti-hormone pills go to work and monitor yourself for met symptoms.
As people say everywhere on BCO, BC is just a crap shoot. So I really believe it's best to just move on as best you can, and be alert but not alarmed.
0 -
muska....for those patients who have metastatic disease, the researchers and clinicians ARE using the blood biopsy in practice. They have identified progression before patients became symptomatic and before it could be identified on imaging! What that translates into is the ability to change treatment more quickly and hopefully give those patients more time.
0 -
The problem with survival statistics is that it makes the assumption that the sample population is suffering only from the disease under comment. Age related survival statistics show how crazy this is. Because one has cancer that does not stop one from having an accident or dying of other causes. The UK actuarial life expectancy tables show 89 for women - for each person living beyond that age one must have died before that age so the business of survival is complicated and not worth losing sleep over. Basically you are either here or not!
0 -
Voraciousreader, I wholeheartedly agree that these discoveries are great. Are you saying they are routinely used to monitor stage IV patients and adjust their treatment plans?
0 -
I hate to continue to take this thread "off track", but the last few comments warranted a post.
I've written a bit about Liquid biopsies / circulating tumor DNA (ctDNA) tests. These new blood biopsies are the future for a variety of reasons. At the moment, they are being used for advanced stage cancers.
I encourage you to visit the thread, "Blood test detects tumor DNA mutations in real time" and read the supporting media articles about the technology.0 -
muska...not routinely, yet....but yes, researchers and clinicians are collaborating in using liquid biopsies to identify progression of metastatic disease. It is making itself known out of the labs and into practice.
Furthermore, in the not to distant future, blood markers will tell us who will need closer screening and who will not which will ultimately lead to the end of population based screening.
0 -
Voraciousreader, I fully agree with you - again. All I am saying, is that NOW clinicians don't know what to do about this scientific data because they don't know how to TREAT. Most of the treatment is still a shoot in the dark. E.g. anti-hormonal pills that most of BC women take. Anti-hormonals are prescribed ad-hoc: let's try one, if you progress we will try another. In the absense of reliable treatment knowing what cells are circulating in the body of a particular woman may not always be in the best interest of that woman.
0 -
muska... The statement you make could be said about most diseases and disorders. Have you ever been to a dermatologist? Often they will prescribe one treatment and if that doesn't work, they will try another, then another and another....
That said, cancer detection and targeted treatments are improving dramatically. Clinicians are depending more and more on blood evaluations...
0 -
Voraciousreader and all interested in this topic: I am as excited as everybody else about the new tests, maybe even more excited because it gives me reason to hope my two daughters will one day have better treatments available if they need them. But I live in the NOW and looking at the treatments that are available NOW, I see they are not very different from what was done two-three decades ago. Let's take my case as an example. I had surgery + chemo + radiation + hormonal treatment. I greatly benefited from improvements in these treatments, e.g. better and less intrusive surgical techniques, excellent anti-nausia drugs, much better and more accurate radiation equipment, more choices for hormonal options, however the underlying treatment approaches have not changed. Again, I am very greatful for the treatment that I received but in essence, it was not significantly different from what was availalbe two dozen years ago or more. I would say that most of the achievements are driven by breakthroughs in technology that facilitate diagnosis but new treastments are lagging.
Back to the new blood tests: I am stage 3 and as such I am in a gray area where they are not sure what to do or what to expect. If you ask me whether I want to have this new blood test done and see how many cancer cells I have circulating in my blood - I don't think so unless I have a clear plan what to do about this information. And I don't think our health care providers know what to do about this information yet. I am not sure the researchers fully understand or know how to use that information. Until they figure it out, I may prefer to enjoy life without knowing how many cancer cells I had in my blood two months ago compared to now. I reserver the right to change my position though :-)
BTW, I would not compare oncology to dermatology where trial and error approach is widely used, after all cancer is not an exzema, we deserve better..
0 -
muska...many of the blood tests were not available a decade ago. Today, targeted therapies are available based on the results of blood tests.
Herceptin, a targeted therapy has been a game changer in fighting breast cancer.
A big change during the last decade and what is driving treatment decisions are tests like the OncotypeDX test. Two decades ago, oncologists knew they were overtreating patients. Now, many patients can forgo chemo thanks to the OncotypeDX score.
The biggest advance that is on the horizon is what Eric Topol, MD refers to in his book, The Creative Destruction of Medicine. That is, clinical trials will be and ARE being based on more "onomics." No longer will patients and their clinicians have to figure out how a clinical trial relates to individuals because the trials are based on large sample populations. Instead, cinical trials will be and some currently are so individual based that data can and is being evaluated more quickly. No need to spend hundreds of millions of dollars on trials lasting a decade or more.
And my example of dermatology, it merely is one example of how medicine works. Kayb does a great job of explaining the science behind how medical treatments are decided. Simplifying how oncology vs dermatology decisions differ is not the point. Instead, the point is that medical decisions are based on evidence based medicine and ethics. Most people would not want a treatment that might be unnecessary and come with long term side effects. I know I would want my clinician to give me the best treatment they deem necessary for ME. Each day, clinicians with the help of researchers are doing a better job at giving us more personalized medicine.
You and/or clinician may believe that the medical community doesn't know yet how to synthesize the data into realtime treatment decisions. IMHO, I have already seen at Sloan Kettering how a liquid biopsy pinpointed a metastatic progression before a patient became symptomatic and well before imaging identified the progression. The clinicians were able to change the patient's treatment and her survival has been extended. That progress is happening NOW. We deserve better and are receiving it.
0 -
Kayb - what are the details of your diagnosis? I don't see a profile under your comment and I am always jealous of people who don't care for further testing. On the other hand, I think it may be lot easier for a DCIS patient (maybe you?) to decline testing than someone in stage 3 where every little pain is a huge reminder of a possible threat. Nis
0 -
I've read the 10-year-old Susan Love's Breast Book and the 12-year-old Cancer for Dummies. The picture they paint is much grimmer than today's. Love barely mention BRCA. That Dummies didn't list TC as a chemo regimen was what alerted me to look at the copyright date.
0 -
Hope I am not intruding here, but as far as I know, any BC that is not metastatic is "counted" as an early stage cancer for the sake of statistics. That would include "locally advanced", whether stage 3A, 3B or 3C. Sometimes 3B and 3C are dealt with separately, for example when selecting patients for clinical trial. But when they are doing studies on treatments, prognosis etc, they usually just refer to stages 1, 2 and 3.
Also, all cases of inflammatory breast cancer automatically get classified as 3B. Because inflammatory BC is particularly difficult to treat, this inclusion tends to make stage 3 prognosis (which includes A, B and C) look more grim than it actually is for those with non-inflammatory cancer.
0 -
muska - I share your point of view of living in the NOW. I agree about the improvements in technology compared to the slow progress made in treatment protocols. NCI as mentioned has now funded clinical trials for "drug" treatments determined by a patient's genetic profiles. These studies and approvals will take years for eventual access by patients......
0 -
I too, am saddened by all the technology being developed to "find" breast cancer. So what? All that would mean to me is that I'm going to find out I'm going to die a little sooner. As far as genetic profiling to treat cancer, meh. Being pro-active to diminish your risk certainly doesn't work, so I'm having a hard time understanding what the big deal is in making any difference when it comes to treatment. We have what we have to treat....that's not going to change anytime soon. All it's doing is giving insurance companies an excuse to weasel out of paying for treatment and denying life insurance applications. It's totally beneficial to them to genetically profile everyone and deny coverage based on it, to treat breast cancer, not so much. I'm obviously missing the big picture, but one more "advance" in breast cancer that translates into me "knowing sooner" is gonna make me barf. They're all so busy worrying about whether or not they could, that no one is stopping to think about whether or not they should. It's akin to throwing a dog a bone so they shut up. "Here, were not going to cure it so take this and quit your bitching". A serious waste of breast cancer research dollars, imo.
0 -
Actually I just deleted my post a second ago. It's kind of redundant to other posts I've made, nor did it have anything to do with the original post. Appreciate your response though.
0 -
Kayb - sorry I lost track of this conversation. Thank you for sharing your experiences. All of what you wrote makes perfect sense to me. I am following in your footsteps, except for not yet having fully let go of the fear of recurrence. I have noted, however, how the process of letting go is happening and how fear seem to dissipate as a function of time. I have looked for scientific literature on this but did not find anything interesting. I do see it in my recent responses to "newbies" and is a definite theme among the "oldies" in this forum. Every time I read "you will be fine, just keep walking," my eyes go to the date of diagnosis and invariably see those hope-FULL comments coming from those who either had it fairly easy (no need for chemo, low oncotypes, etc) or time has helped them forget. As for scans, while they don't stop cancer recurrences, they might help catch them sooner. And I feel deep pain in my heart when stage IV sisters describe how they wished they had been followed more closely. Hugs, Nisa
0 -
There are triple negative and her2 in that figure I suspect. Plus the figure drops to 50% at 30 years due to late reoccurrences
0 -
Whoa, we need to be careful with that "50%" stat because it's going to scare a lot of people, and it's simply is not accurate for women who are diagnosed today.
It is true that the current SEER database does show 30 year survival - for all invasive breast cancer, including both early stage and advanced (but not including Stage 0) - to be just under 50%. But this survival rate is based on women diagnosed prior to 1985. In the 30 years since, there have been many advancements in treatment that have significantly impacted long-term survival.
For example, Tamoxifen was approved by the FDA for use for metastatic cancer in 1977. It started to be used on an unofficial/ad hoc basis for earlier stage BC in the late 80s and early 90s. Wide usage for early stage BC came after that. So the survival benefits of Tamoxifen in the mortality stats will only start to show up around the late 90s and early 2000s.
AIs were approved for treatment of invasive cancer only in 2005. Herceptin was approved for women with advanced breast cancer in 1998 but was only approved for those with early stage diagnoses in 2006. The SEER database that is currently available has 10 year survival data only for those diagnosed in 2004 or earlier, which likely means that the data is yet to show much of the survival impact of these drugs on early stage women.
Meanwhile, the survival data at 10 years through to 20 years, and even 25 years, is showing significant improvement for those more recently diagnosed (but still diagnosed more than 10 years ago), which would suggest that over time, we can expect the 25 year and 30 year survival data to also improve significantly.
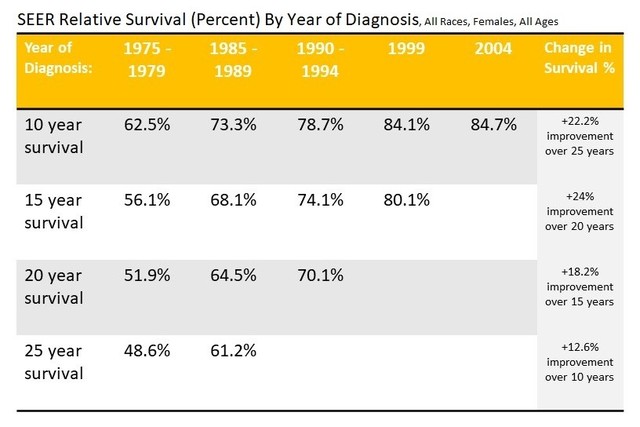
Here is a link to the SEER database: SEER Relative Survival (Percent) By Year of Diagnosis, All Races, Females, All Ages
0