BC & Autoimmune Diseases: How many? What does the research say?
Comments
-
Candy hou haven't been diagnosed yet with the syndrome you researched right? And who would give you the blood thinner? The rheumy? The MD that gives you the blood thinner should have the answers to your questions. Now you have some information so you are prepared for the Monday appointment. Maybe the MO didn't shrug you off, she just wants to wait for the rheumy's dx and his interpretation of your lab work.
Yes an Oncologist can be a Hematologist.
0 -
No I have not been officially diagnosed yet. But I have been reading up on it, a lot. And all the criteria are there. I have history of autoimmune issues already, the labs were positive, I have had a documented event of TIA. The rheumy would give the thinner from what the PCP and MO are saying with my phone calls. I don't know what the rheumy thinks of that, but the other docs have deferred to him. But if the rheumy is comfortable treating the syndrome with his other patients, are they cancer patients? The cancer is the key point. I wouldn't think twice if I didn't have cancer. Autoimmune syndrome, rheumy treats it, makes sense. But does the rheumy know the caveats of the cancer with the syndrome??????
0 -
You will find out on Monday. That is only three days away. Don't have a TIA in between time, and don't forget to ask him about the different blood thinner meds if he prescribes one. Did you go to drugs.com and read the comments on the different thinners. Also you can go to Ask A Patient snd see what they ar saying about the different meds. And ask the Rheumy if he is comfortable prescribing for a cancer patient. I would think he is. But you have the right to ask if he's had other patients. Some doctors get irritated with too many questions. Sometimes it's because of time constraints. Lots of people get irritated with questions. There's a chance you will get your answers without having to ask.
I was joking about don’t have the TIA
 0
0 -
Marijen-- I am going to look up drugs.com and ask a patient this weekend. The more I can learn the better. Thank you for a kind ear about all this, and for looking up the articles for me. This morning some time with sister going shopping.
Spoonie--- hope you are feeling better.
0 -
I was reading Ibrance Thread---I post a lot on there since I am on Ibrance as my first line therapy. There is a lovely lady named Philly who posts. She posted yesterday about having a sore throat and the end of her Ibrance cycle and was concerned so she called her onc to report it. She commented that she is "a super compliant patient and tells them EVERY single side effect". I envy her relationship with her onc. If I called my onc with side effects of my meds, they would have a field day. "Oh it is Candy again. She is looking for a problem". That is how I feel I am looked upon by my onc's office. And I don't know how to change it. I see my onc every 6-8 weeks for appts, have my questions ready for the appt to be efficient, and the only bother them by phone is if I feel it cannot/shouldn't wait until next appt. Like I said here, I fear calling them and question if I should. I hate that I don't have a comfortable relationship with them. Sigh.....
0 -
No problem Candy, I’d like to know about bleeding lesions too. It seems to me that that it would be an opportunity for cancel cells to spread. That would be horrible, obviously.
0 -
Thanks everyone for the wishes on feeling better. Today is indeed a better day, at least out of bed and on the couch, hoping to get a couple short puppy walks in later today.
Candy - That is so hilarious about your kitty and the light switch. Brilliant feline mind! I am sure I would have been creeped out too to discover the light on, all by itself with no one home!!! I guess that's a clear message that "Hey I'm home too, leave a light on for me so I don't have to hang out in the dark, would ya please?"! LOLOLOLOL.
I looked over those 2 studies that Marijen shared -- here's my take:
Basically the first one says blood thinners (enoxaparin (Lovenox) studied) are safe to take with brain METs/lesions. Blood Thinners OK For Cancers That Spread To Brain
The second one doesn't say this isn't true, instead says that there are other drugs that can interfere/block effectiveness of various blood thinners from the NOAC family (nonvitamin K oral anticoagulants), putting patients at increased risk of bleeding when this occurs. This includes drugs they looked at like abigatran (Pradaxa), rivaroxaban (Xarelto) and apixaban (Eliquis). So, this is something to be aware of and talk over with your drs if anti-coagulants are prescribed.
--------
"NOACs alone DO NOT pose a significant risk of bleeding, BUT the concurrent use of NOACs with certain drugs that share the same metabolic pathways may cause increased risk of major bleeding," said study lead researcher Dr. Shang-Hung Chang, an associate professor of cardiology with Chang Gung Memorial Hospital in Taoyuan, Taiwan."
Drugs studied that INCREASE RISK OF BLEEDING while on a NOAC: "The investigators found that bleeding risk increased significantly when NOACs were used in combination with amiodarone, fluconazole, rifampin and phenytoin -- four drugs that treat widely different conditions.The researchers also found that other drugs dampened the effectiveness of NOACs, including atorvastatin, digoxin, and erythromycin or clarithromycin." blood-thinners-can-come-with-dangerous-side-effects from Health News---------
More Info:
Anticoagulation Strategies in Cancer Patients (2019 Geoffrey D Barnes)
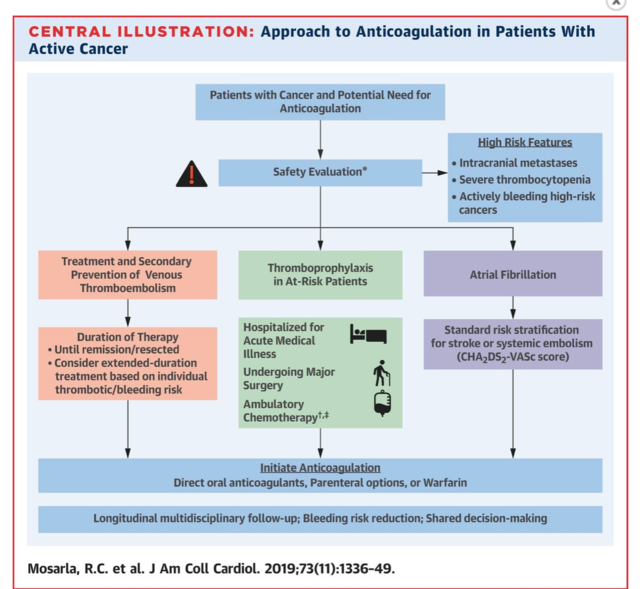
"The following are key points to remember from this review article about anticoagulation strategies in patients with cancer:
- Patients with active cancer are at increased risk of arterial and venous thromboembolism (VTE) and bleeding events. This results from cancer-specific impacts on all three elements of Virchow's triad (stasis, endothelial injury, and hypercoagulability).
- Certain cancers are associated with high or very high risk of thrombosis (especially VTE), including pancreatic, stomach, metastatic, gynecological, lung, brain, hematologic, and genitourinary cancers (excluding prostate).
- Certain cancer therapies are associated with a high risk of atrial arrhythmias (e.g., atrial fibrillation [AF]), including anthracyclines, alkylating agents, antimetabolites, interleukins, Bruton's tyrosine kinase TKIs, and immune checkpoint inhibitors.
- Historically, in patients with cancer, low molecular weight heparin (LMWH) has been the primary treatment choice for patients with VTE, while warfarin has been used for stroke prevention in AF.
- Recently completed studies in patients with cancer-associated VTE have demonstrated efficacy with edoxaban and rivaroxaban as compared to dalteparin. Subanalyses of the RE-COVER, EINSTEIN PE/DVT, AMPLIFY, and Hokusai-VTE studies also show efficacy of dabigatran, rivaroxaban, apixaban, and edoxaban as compared to warfarin. Bleeding rates with the direct oral anticoagulants (DOACs) have been variable across different studies.
- Several ongoing studies comparing DOACs to LMWH for treatment of cancer-associated VTE are ongoing and will provide further insight into both efficacy and safety of DOAC therapy.
- Use of DOAC therapy in cancer patients may be limited by potential drug-drug interactions. These include P-glycoprotein interactions (all DOACs) and CYP3A4 interactions (most strongly impacting rivaroxaban and apixaban).
- Renal impairment and thrombocytopenia are both common in patients with active cancer and may impact the safety of DOAC therapy. Using a DOAC with less renal clearance may be preferable. Avoiding anticoagulation when platelet counts are <50,000-70,000/μL is often recommended.
- Although one retrospective study of patients with brain metastases showed no increased risk of intracranial hemorrhage risk with LMWH versus no anticoagulation, it is not clear if this is generalizable to all patients with brain metastases. Nonetheless, DOAC therapy is associated with lower intracranial hemorrhage risk than warfarin broadly, and availability of reversal agents may swing the risk:benefit ratio in favor of treatment for many patients.
- Most patients with cancer-associated thrombosis will require treatment as long as the cancer is active (until remission or resection). Extended treatment may be considered based on overall risk:benefit assessment.
- Hospitalized patients with active cancer are at high risk for thrombosis and should receive aggressive thromboprophylaxis as long as there is not a prohibitively high risk of bleeding.
- Patients with cancer and AF should be treated according to standardized risk stratification scores (e.g., CHA2DS2-VASc)."
Anticoagulation Strategies in Patients With Cancer (Journal of the American College of Cardiology 2019)
**there's a pay wall I couldn't get past, but here's the abstract and chart***
- "Patients with active cancer face higher risks of arterial and venous thromboembolism (VTE), atrial arrhythmias, and bleeding events.
- Historically, in patients with cancer, low-molecular weight heparins have been preferred for treatment of VTE, while warfarin has been the standard anticoagulant for stroke prevention in atrial fibrillation.
- Select direct oral anticoagulants have now been shown to safely prevent thrombotic events in recent clinical trials, and present an attractive oral dosing option for patients with cancer.
- Multidisciplinary care that accounts for individualized bleeding and thrombotic risks, drug-drug interactions, patient preferences, and periodic clinical reassessment is warranted to identify the optimal anticoagulation strategy for patients with cancer.
Abstract
Patients with active cancer are at an increased risk of arterial and venous thromboembolism (VTE) and bleeding events. Historically, in patients with cancer, low molecular weight heparins have been preferred for treatment of VTE, whereas warfarin has been the standard anticoagulant for stroke prevention in patients with atrial fibrillation (AF). More recently, direct oral anticoagulants (DOACs) have been demonstrated to reduce the risk of venous and arterial thromboembolism in large randomized clinical trials of patients with VTE and AF, respectively, thus providing an attractive oral dosing option that does not require routine laboratory monitoring. In this review, we summarize available clinical trial data and guideline recommendations, and outline a practical approach to anticoagulation management of VTE and AF in cancer."
Strategies for Using Anticoagulation Therapy in Patients With Cancer (Doyle 2018)
"What Anticoagulant Should Be Used for Patients With Cancer?As Dr. Kempton reported, the long-standing CLOT trial established the superiority of low–molecular-weight heparin over warfarin for the treatment of cancer-associated thrombosis, with a nearly 50% relative risk reduction with the use of dalteparin vs warfarin.6 The CATCH trial showed a similar benefit of tinzaparin (Innohep) over warfarin with associated reduction in the risk for bleeding.7 According to Dr. Kempton, however, the recent introduction of direct-acting oral anticoagulants has generated a great deal of clinical interest because "they are much simpler than the use of subcutaneous injection."
"Overall, in patients without cancer, direct-acting oral anticoagulants have been shown to be slightly safer than warfarin for the treatment of VTE," said Dr. Kempton. "For select patients, warfarin may still be more appropriate, but direct-acting oral anticoagulants are becoming the standard of care in this space."
0 -
Wow Spoonie! Candy, is your brain fried yet?

Candy, I have more info on Rheumatoid Arthritis and Vagus Nerve Stimulation, would you rather wait?
 0
0 -
LOL Marijen - It can be alot. Take in small doses.
 0
0 -
WOW thanks Spoonie. And Marijen please send along your info. I just got home from a day with sister and niece. Went to a couple of stores and out to lunch. I am not even going to try to comprehend all this right now----tired. But THANK YOU BOTH for helping me soooo much. I am going to chill for the evening and will reread all this tomorrow. Nothing planned for tomorrow so I can LEARN. Will post again when have educated myself !!!!! Hugs.
 0
0 -
Here you go Candy. Also look up how to stimulate your vagus nerve. There are many ways. (follow the links to be overwhelmed!)
https://www.medicalnewstoday.com/articles/325532.php
https://selfhacked.com/blog/32-ways-to-stimulate-your-vagus-nerve-and-all-you-need-to-know-about-it/One more for RA -
Baltzer AWA, Stosch D, Seidel F, Ostapczuk MS.
Z Rheumatol. 2017 Nov;76(9):806-812. doi: 10.1007/s00393-017-0309-1. Review. German.
- PMID:
- 28466181
0 -
INVESTIGATION: Google Manipulates Search Suggestions To Promote Pharma, Discredit Natural Health
https://www.greenmedinfo.com/blog/investigation-go...
0 -
So Candy, how did your appointment go today?
0 -
Marijen, Spoonie, and Jaycee----- First of all THANK YOU SOOOOOO MUCH for being my virtual friends and helping me out so much. I know you truly care. You looked up articles for me and listened to my rants, and I appreciate it more than you can know. I logged in to BCO to give an update and I see Marijen has already posted to check on me. Oh My Gosh. I love you guys.
So...here it is.... the update.
First I was really scared of the appt. Of course, I went by myself. I go to all appts by myself. That is the way it is. I prayed while I was waiting for the doc to come in the exam room. Yes we think I have Antiphospholipid Syndrome. As per protocol---yes protocol since I have been reading about this syndrome for the last week I have learned that--- we will redraw lab tests in 3 months to verify. If still positive then, then Yes diagnosed with the syndrome. We think it is already diagnosed with my history of autoimmune issues, but that is protocol. THEN, the treatment would be up to the onc !!!!!!!!!!!!!! per the rheumy. He said my case is "complicated" with the cancer and the syndrome. Normal protocol is to use warfarin/Coumadin, but with the metastatic cancer bleeding can be a problem.
Oh my gosh. The PCP deferred to rheumy. The onc deferred to rheumy. Now rheumy defers to onc. I WANT the onc to handle it. The more I thought about it, while reading all the articles you guys have posted, I think the onc/hematologist SHOULD be in charge. But good grief the passing the buck.
So.... now I see onc July 24 as my regularly scheduled appt (after scheduled CT scan). And I plan on discussing all this with her then. She had better plan to set aside some extra time for my appt. Plan to retest labs in 3 months and see rheumy in 3 months to follow up. And I will continue to use baby aspirin ( I prescribed myself ).
Got to go for now, sister calling.
0 -
Hi Candy,
Nice update! I hope your Rheumy was impressed with your knowledge. When you get back I am curious about something - on the Antiphospholipid Syndrome. Did you bring it up first or was your Rheumy already considering it? You have a lot on your plate. Keep a close watch on those liver mets! How is your Ibrance working so far? (you might have posted this elsewhere).
0 -
Marijen--- Yes rheumy was considering the syndrome and brought it up first. Then we discussed the cancer and all the things going on. I have not seen rheumy since Spring 2018 so he was not up to speed with everything so I had to fill him in. Also, he has so many patients ( goes to 2 offices during the week ) I know it is hard for him to keep things straight. I felt that way before the cancer when I saw him for the autoimmune issues. I felt like I was a new patent every time I came in. Had to review my case with him each visit. And that was before the cancer. So I definitely was worried about him handling all this. I wonder if he could handle the complexities.
I didn't tell you I asked him to send a note to onc about his findings and recommendations. He said he is not obligated -his word- to send a note, but I asked him to anyway. I thought that way the onc could have evidence that he wants onc to handle this.
About Ibrance, next CT later in month to see if liver mets is still controlled (has been).
0 -
Your Rheumy does a report of your visit right? Your MO access that information? Or are they at two separate clinics? Candy it sounds like you are really on the ball with all this and it’s a good thing that your are. Do you know what caused your Antiphospholipid Syndrome? Phew! Such a long word! I see something can trigger it, like viruses, bacterial infections, other things.
0 -
Yes the rheumy does notes for his patient charts. But different computer system from MO and PCP. All 3 different systems that don't flow together. Cause?---- good question. I don't remember reading about viruses, etc causing it. Will have to review info. I just read it is an autoimmune disorder and can affect people with other autoimmune disorders of which I have 2 and an eye condition that is similar (connective tissue disorder). Don't know how long I have had it as we have never tested for it before. I did have a blood clot in 2017, but don't know if this was the cause since we didn't test for the syndrome at that time.
0 -
I was just curious on the cause. I think medications can be a cause. I just searched the syndrome plus causes. Why don’t you get a copy of the Rheumy’s report and give it to your MO. That way you won’t have to count on him to send a note.
0 -
Thanks for sharing the good update Candy. It sounds like things will be complicated juggle but hopefully the drs will come together a bit to help give you the best outcome in all of this. Keep us posted on how your MO appt goes later this month. Thankfully it's not too far away and that at least while you wait, you have a plan in the works with your Rheumy for this syndrome.
I'm curious too, like Marijen, on how the AntiPho Syndrome came about. I know for me, my Chronic Lyme Disease triggered my genetics and gave me my lovely "best frenemy" Chronic Inflammatory Response Syndrome where my body never knows how or when to turn off inflammation. Makes life reaaaaaaal grand. I'm on the frontlines, literally, of new medical frontiers. Ugggh. Hopefully your Syndrome is more well known and researched.
Oh, and I'm so glad some of the info was helpful. Wish there were more I could do, like get in a mini sub movie style and go fight those liver mets face to face. Since I can't, well I can sure Google a few things instead.
 0
0 -
Thanks marijen and spoonie. I was first diagnosed with autoimmune issues in 2014 at the age of 44. But I think I had issues waaayyy before that. Not going to rehash my history from childhood, but things have been "off" with my health my whole life. And in hind site I think my immune system has had problems all along. We found the issues in 2014 by asking my PCP to do some labs after my eye doctor diagnosed an illness that is closely related to other autoimmune issues. I told the PCP I thought there could be other issues, with my history and also a cousin with Lupus. We did the tests and they were positive and that opened the door to the rheumatologist visits and the diagnosis'. What really causes any of the autoimmune issues???? Genetics? - family member with Lupus. Environmental?? An illness somewhere in my history?? Does anyone really know what causes autoimmune issues.
I did read a medical journal article about an Aromatase Inhibitor causing a case of Antiphospholipid Syndrome in a lady. I am on an Aromatase Inhibitor. But I have the documented history from 2014 of autoimmune disorders. So which came first the chicken or the egg.
Getting a copy of the rheumy's report sounds good. I can make sure onc gets copy AND I can read it myself. Interesting.
Chronic Inflammatory Response Syndrome--- I am going to have to read up on that. A lot of the autoimmune disorders are cousins to each other. And if a person has 1 they can have others. In 2015 we found a thyroid nodule. Thyroid issues can correlate with autoimmune issues. And I wonder if I have IBS (another autoimmune issue) but I have never been to a GI doc to have it diagnosed. Neat that you are "on the frontlines... of new medical frontiers". How did you get to do that? I would love to delve into my conditions, genetics, and how my body responds. I think it could be untapped territory to be able to study why the body responds the way it does to the autoimmune issues and then to have metastatic cancer.
Good discussion.
0 -
Spoonie--- Read your link. Wow. You have had a lot to deal with also. How long have you been dealing with this? Who do you go to for your treatment?
Hugs.
0 -
Hi Spoonie and Candy,
I read your link too Spoonie, sort of, because it's a lot to digest and figure out. Way too complicated. Why no bananas? It's so much to deal with when we have all these different diseases/variables going on at the same time. How do you manage?
And the same for Autoimmune, Candy. I have two thyroid nodules since radiation, fibrosis in one lung from radiation, and now I'm being told I have radiation neuropathy, i.e. my whole body hurts. Candy, you are entitled to all your reports. You need to have them to keep track of things and do your own research. They don't give you reports through a portal? Doctors rush through things and don't tell you everything but what they don't tell you should be in your reports.
Looking forward to hearing about your MO visit later this month!
0 -
Hey ladies, just home from appt with MO and my first Zoladex injection and am wiped out from the travel. Need to rest and recharge and then will get back to you all in more depth.
As to the front lines comment, I meant that since this syndrome is in its infancy (first diagnosed patients began emerging in late 2000s I think), and I was a patient of one of the very first doctor's trained by the doctor who started it all rolling, Dr. Ritchie Shoemaker. So while there are tons of patients, when I was first dxd, there weren't. So i'm used to trailblazing lol. This guys short story on The Mighty is a lot like mine ins some ways--- https://themighty.com/2017/01/lyme-disease-and-chr... (I have the two dreaded genotypes, relapses/remissions, and was also dxd on 3 different occasions with Multiple Scelerois however I do not have MS, I have Chronic Lyme and Chronic Inflammatory Response Syndrome plus a whole other page of dxs. Also including my allodynia which sometimes leaves my sheets hurting my skin sooo bad that it feels like razors.. Uggh. It's a lot. I'm working on a post about some of the labs (inflammatory markers) that I have found studies showing a link to cancer growth...I will be curious to see if others have info to post about it too.
If anyone wants to read more about CIRS....https://www.survivingmold.com/docs/Berndtson_essay_2_CIRS.pdf (might be easier to process IDK)
Ok off to bed for me and to rest. I'll be back.
 0
0 -
Marijen- I have a portal for my PCP, but not for the MO or rheumy. And even for the PCP portal, it only shows certain things---med list, problem list of diagnosis', vital signs flowsheet. It does not have access to doctors notes. So any narrative notes the doc writes after he sees me for an office visit-or letters to another doc- is not placed in the portal. So to get a copy of the letter I want the rheumy to send to onc, I would need to ask in person for a copy. And I would LOVE to read the notes my MO does after our visits. Of course, when I ask the MO my list of questions each visit I jot down the answers during the visit. But it would be interesting to read her notes she dictates into the chart---compare and see if she has any other thoughts she is placing in my chart.
0 -
Candy, in that case, you can contact Medical Records at each facility and request all your records. That is the law and your right. All you have to do is fill out a consent form. Shame on them for being so backwards. Egads! That would make me nuts.
0 -
Ok I need to vent and get advise from my friends on here. I will probably cross post to several threads to get several ideas from you all.
I had my MO appt this morning ( last seen 2 months ago ).
I discussed my positive results of blood test for an autoimmune condition that can increase the risk of blood clots-- What I had posted about before on this Thread. She was upset. She said she treats the cancer and it is the responsibility of the rheumatologist that ordered that test to treat this. I was wanting her - hematology/oncology - to handle it all. She said she was able to, but would not since she did not initially order the test. She treats my cancer only. OH MY GOSH !!!!!!!!!
Everyone is passing the buck with this. My PCP wants the rheumy to handle, the rheumy wants hematology/onc to handle, and onc wants either the PCP or rheumy to handle.
I am about to say forget it. NO ONE WILL TREAT IT AND I CAN JUST HOPE I DON'T HAVE ANYMORE BLOOD CLOTS IN THE FUTURE.
What do I do???
0 -
Candy, I hate to say this but this is how medicine works now. I wouldn't post this on the Ibrance thread because there, everything is happy happy. The onc practice I go to and most of my other practices are OWNED by one of the hospital corporations in town, There are two. 90% of medical practices and facilities are owned by one of them. Their object is to make money. That's all. My MO told me that on Wed, when I used to have all my appointments, there are two big meeting that she is required to go to. All days, including Wed, when several hours of her time is taken up by these meetings, she is required to see some number of patients. I forget the number she told me. She told me this when I asked her why she always ran so far behind on Wed. The hospital corporation dictates what she does. She can probably take longer and I know she does but still, the time pressure is there. Insurance also dictates what doctors can do now. My former MO told me he spends 90% of his time dealing with insurance. He is a jerk so he was probably exaggerating but that was what it felt like to him. Telling. For older doctors, this is not what they signed up for. For younger doctors, they maybe knew but not just how bad it has gotten. Your MO has chosen to react as she has with you. I appreciate her honesty. She is telling you up front what she will and will not do. Most doctors don't do that but still proceed according to the rules. Then you get all kinds of nice surprises. I'd like to be giving you better news but where I live, this is how it is. There are a few independent doctors but they have to fight to survive. Most practices have a "method" to make extra money, like a way to do "procedures." Those are the money makers. My neurologist has an MRI machine. His first suggestion is that I have one. No RX without an MRI. His NP told me that last time I tried to get neurontin. I declined. You might want to find out how the economics of your MO's practice works. Who owns them? Who dictates what they do? Might not help but I like to know. Maybe there is an independent practice where you live.
0 -
Candy, I thought your appointment was July 24 and wondered why you didn’t post. So it seems to me that since rheumy sent you for the test and rheumy dx’d your problem but you need another test to confirm. Then rheumy should treat. Also maybe MO is restricted like Jaycee says and/or MO doesn’t want the responsibility where rheumy knows better. When is your 3 month follow-up? And does rheumy know you are taking baby aspirin? I wonder if that will affect the test? I looked up your dx and you could also go to a neurologist...
0 -
Jaycee--- Hahahaha you saw I posted already on the Ibrance Thread. My MO practice is owned by our local hospital (corporation).
Marijen- Yes appt was 24th but I got a call the day before saying that something came up and they had to reschedule my appt. I think the onc CAN handle but WILL NOT due to being aggravated with PCP/rheumy for ordering tests and then backing off from treating and saying onc can do it. All docs know I put myself on baby aspirin until this can be resolved. None of them PRESCRIBED it. Yes I can go to neurologist. I just hate having too many cooks in the kitchen. Makes more sense to me for hematologist/oncologist to take care of cancer and clotting issue both. But what do I know???!!!!!!
0