Breast MRI Explained
Comments
-
Extra Credit Reading Assignment
Here is a nice summary of the physics of MRI image acquisition for those of you that are interested in the details.
0 -
Hi, I had my 6 month mri follow up last week. My results from the biopsy I had 6 months ago stated right breast benign, left breast intraductal papilloma. This follow up mri report states now both breast they found areas that increased in size. My dr said the radiologist were a little taken back by my right breast being that the biopsy came back complete benign. Surgical excision was recommended for both breast birads 4-suspicious. Also my question here is, the term type ll plateau and type lll washout. Are implied on both breast. I just want a complete understanding what that means. I know it’s MRI terminology but it seems once again their unsure and just want me to remove it from both breast.
0 -
see below for a complete understanding of Breast MRI kinetics
Type 1 curve with slow rise and a continued rise with timTemporal Resolution - Kinetic Analysis (Curves)
First we look at the initial upslope of the curve during the first one to two minutes.
This is either slow, medium or rapid.
Then there is the delayed portion - two minutes or more after the injection of contrast.
This part of the curve shows either an increase, plateau or washout.
The kinetic analysis takes about six minutes of repetitive scanning in total and can lead to three types of curve.Type 1
On the image on the left is a type 1 curve.
There is a slow rise and a continued rise with time.
A lesion with a type 1 curve has a chance of 6% of being malignant.======
Type 3 curve with rapid initial rise, followed by washout in the delayed phaseType 3
The type 3 curve shows a rapid initial rise, followed by a drop-off with time (washout) in the delayed phase.
A lesion with this type of curve is malignant in 29-77%.
This is the red on the CAD (Computer Aided Detection).=======
Type 2
Then there is the type 2 curve, which is in the middle: a slow or rapid initial rise followed by a plateau in the delayed phase, which is allowed a variance of 10% up or down.
The chance of a lesion with a type 2 curve being malignant lies somewhere between the 6% of the type 1 curve and the 29-77% of the type 3 curve.
Many physicians will biopsy lesions with type 2 curves.For non-mass enhancement, kinetics are not very useful.
If there is clumped enhancement in a breast it must be biopsied, even though there are no areas with a type 3 curve.0 -
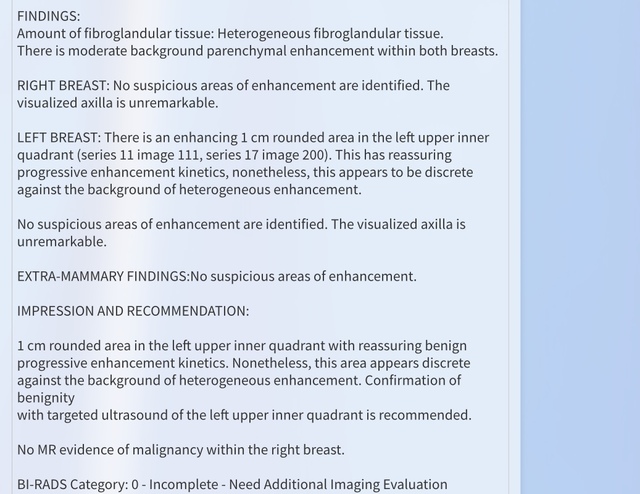
I’m confused about my latest MRI (my third this year) results. This imaging place is not as comprehensive on explanation of results.
History
40 partial Hyst borderline cervical CA 2003
ADH, CCH, Apocrine Metaplasia both breasts
Last MRI (April 18’) stated several areas of focal enhancement outer/inner lower quadrants left side- that.is why I was supposed to have this MRI and yet this report does not talk about that at all. Same type of machine GE 3
May 18’ bilateral silicone implant removal and bilateral reduction for left side rupture and 3 lymph nodes measuring 3cm+ Due to silicone
Previous MRI stated incidental finding of Sternal hemangioma.
This report doesn’t mention my nodes or sternum. I know my nodes are still large. I can feel them just the same however they list them as not noteworthy.
 0
0 -
Should I will assume your question is why didn't they mention the lymph nodes, spots of focal enhancement and the sternal hematoma again?
Really no way to know, I can only guess. Since the lymph nodes enlarged by silicone is a benign process and already reported they might have chosen to say 'nothing bad seen there' for the sake of brevity. Same I imagine with the sternal hematoma especially if it had resolved in the meantime. If you still have your ovaries you are still cycling hormonally, if the scans were done at two different points in the cycle that could explain the presence/absence of scattered areas of enhancement.
My problem with the report is they don't mention comparing it to any priors. They don't use the word NEW with that nodule whcih they maight have if they had the old studies. I would ask if they did and to which priors did they compare the present exam.
0 -
Yes I was confused with the fact that none of the previous issues were mentioned, especially considering the nodes are bothersome and I have mentioned that to them. Yes, they compared this MRI with previous MRI’s this year as well as several previous US and mammo. That was an issue because they couldn’t find my previous testing in their system intitially which caused a three week delay in getting results. It was a sternal hemangioma. Can those resolve What is your take on the description of the new area? I feel like it’s missing info. I have your MRI link you posted and it doesn’t feel like they used enough identifiers to give another dr a mental picture. I’m supposed to get to talk with the radiologist at my US but they’re backed up so I’m not sure when that will be. Thank you so much.
0 -
Hello everyone.! I recently got a breast mri done and await my results. I wanted to know if the breast mri can tell if there is anything going on in your upper back/shoulders ? Or it focuses only on the breasts.
0 -
The field of view is adjusted so that it includes the breasts, the anterior chest wall and both axillae. If it includes any portion of anything else, it is incidental. Also the imaging sequences are chosen to show breast abnormalities and may not show an abnormality in adjacent anatomy even if present.
MRI is extremely good for musculoskeletal problems but only on dedicated exams.
0 -
Thank you for the reply
 my reports came back showing I have enhancing lesions in outer quadrants of both breasts that they want to mri guided biopsy. My doctor thinks it's probably benign. I thought only masses could be biopsied? I'm trying not to panic but I am. 0
my reports came back showing I have enhancing lesions in outer quadrants of both breasts that they want to mri guided biopsy. My doctor thinks it's probably benign. I thought only masses could be biopsied? I'm trying not to panic but I am. 0 -
MRI is sensitive enough to detect DCIS before there is a mass and it is usually described in the report as "linear non-mass enhancement". There is however a fair amount of overlap of the appearance of DCIS with benign tissue enhancement during portions the menstrual cycle when hormone levels are highest. This is why exams should be timed with the cycle unless there is an obvious cancer to be dealt with.
=================
My routine was always to evaluate the MRI findings with US and compare those to the mammo. It can be subtle but on a good machine you can detect DCIS on US well enough to biopsy it even without a mass present. If there are calcifications on the mammo in that area, to me that increases the pre-test probability.
1 -
I got a mammo and usg done 6 months ago where they saw many cysts. Mammo was inconclusive because I had dense breasts. And they asked me to get mri done as screening. To give an over view I turned 30 this year and my mom passed away last year from breast ca.
I'll post my result when I read it. Right now I have only heard from my doctor who said she thinks they're benign findings most likely but I should get it biopsied. And I'm Terrified.
I got the mri done on th 15th day of my cycle. Is the mri guided biopsy also done with respect to the menstrual cycle.?
0 -
The timing of the biopsy is less critical than the timing of the diagnostic study.
0 -
One last question.. Does it matter that i took progesterone only pill (emergency contraceptive) a day or two after the mri was done. I plan to let the radiology dept know.
Thank you for responding!
0 -
My mri with contrast was done 6 months after the usg and mammogram.. Do you think they should do it again with the mri to correlate..? There was no mention to the previous usg/mammo report. The radiology report also said that I am overdue fr the mammo and usg.. And along with it suggested i get biopsy.
They found three lesions, 2 in right and 1 in left measuring a 1.2 to 1. 7cm.. Segmental, segmental linear and circumscribed enhancements. I'll be going for the mri guided biopsy in a week.
1 -
Nor do they show most Invasive lobular breast cancer which accounts for 10 to 15 percent of all breast cancer
0 -
Still not sure how to post here -- my previous message regarding Lobular cancer was not related to MRI -- I thought that I was responding to the person who talked about how many things the mammogram doesn't show.
0 -
It would only have affected the images if it was taken before the MRI.
0 -
I assume you are on the surveillance protocol (mri/mammo 6/6 months). Usually when there is a new finding(s) on the MRI it triggers a new US in an attempt to locate it/them as it is faster/easier to bx with US than MRI. Not everyone is comfortable trying to image non-mass MRI findings on US. The findings can be very subtle.
========
My routine was to sit down with a cup of coffee, lock the office door, and review all the images for that patient to see if there are any landmarks in the breast that can be seen on both MRI and mammo that might help me find the new abnormality on US. During this review I would occasionally find something that correlated with the abnormality itself like a few calcifications that would otherwise have been "below threshold" on its initial reading.
I often reference the parable of the 'Blind Men and the Elephant' when discussing complicated cases that were read/performed by many different radiologists/at many different imaging centers. At some point in time one person needs to review all the studies all at once and put together one impression and from that the most appropriate recommendation(s).
0 -
Love the parable DJ....puts great perspective on the process...thanks for posting!
 0
0 -
jessie123 et al
Nevertheless you bring up an important issue.
======
NB: The following is a long caffeine fueled rant that contains opinions along with facts. Viewer discretion is advised.
The concept of whether something can be seen on a particular study or not is important in all of imaging not just breast but is particularly important in breast imaging.
The first important concept to understand is looking at mammograms is like looking at fingerprints. They are unique to you. Your mammogram looks different from your neighbors. You can remove the names and mix them all up but you will be able to separate each person's exam into neat little piles. Not so with chest xrays, cat scans of the bodies and heads etc. Unless there is a glaring abnormality they can look nearly identical. This is why it is easier to find an abnormality on all those other exams and why I feel it is more difficult with mammograms
If an abnormality that exists within the breast is not reported it either was a) not visible in the images b) present in the images and not seen or c) present in the images, seen, and felt to be normal/benign. A is related to the physics of the modality, B is a problem of perception and C is a problem of interpretation.
These are 2 of my favorite adages to quote to radiology residents regarding B and C:
The first is: "You see what you look for, and you look for what you know". This is very old and I am not sure who originated it but it speaks to the value of the radiologist's experience in a particular type of imaging. Regardless of the intellect of the radiologist, one who is involved in reading all modalities perhaps with a non-breast subspecialty, cannot possibly read as many mammograms per year as someone who reads nothing other than breast imaging. The rad who reads more studies sees more cancers and misses fewer cancers than someone who reads fewer.
The second is: "One old film is better than 2 old radiologists" which speaks to the value (necessity) of comparing the new studies to ALL the old studies not just one or two years worth of the same modality but ALL the old studies. There were many many instances of biopsies that I had to cancel when a mass was seen on a mammogram that appeared to be new when it was present on a study from 8 years ago that no one bothered to check since most only go back 2 or three as a routine. Also there are cases called normal when a finding appears to be stable over the past 2-3 years. You go back 6 years and see it wasn't there at all and you realize this thing has been growing very slowly over the past 5 years. ( I am the author of this quote).
This brings us back to lobular breast ca. After a while as a radiologist you have in your mind's eye the appearance of the abnormalities you are looking for. This works for many studies but it can be a hindrance in breast imaging. If you are looking for a roundish mass with spiculated borders on every screening exam you will miss lobular ca as it does not grow that way. Many of the lobular ca's that I have found have merely been areas of nondescript breast tissue that were new from the prior study either as an isolated patch of tissue or an area of fat density on prior exam that has now been "filled in" with normal appearing parenchymal tissue density. You would really have to know what you were looking for and compare with many prior studies to make the call.
This is the reason behind all those people being called back for an "asymmetric density" because sometimes that is your only clue to the presence of a lobular carcinoma. The vast majority of time it isn't but no one wants to take that chance.
Here is a scenario I have seen a few times over the years. Let's say there is a small, subtle lobular ca on a baseline screening exam in otherwise symmetric appearing tissue on each side read as normal as part of a routine morning of 100 screening exams that needed to be completed before lunch. The recommendation is come back in a year. So she comes back in a year, or if her PCP goes by the USPSTF recommendations, she comes back in 2 years and now there is an obvious mass/asymmetric density that is called back and eventually shown to be a lobular cancer. You pull out the baseline study and there it is, a small density right there where the mass is now, showing that it was visible on the initial exam.
So did the baseline mammogram demonstrate the cancer or not? Did the radiologist miss a potentially deadly cancer or did they read the study appropriately?
0 -
You are right. I was told to follow up after my 1st usg and mammo. And get a baseline mri due to family history and as I had many cysts abd dense breasts. And you're right that was done at a different center. I got the mri after 6 months without the usg and mammo. Should I ask them for it to correlate? I wud like to get usg guided biopsy if that's simpler

I'm scheduled for a vaccum assisted mri guided biopsy b/l of three areas.
Thank you for the insight. There was a time when I wanted to pursue training in radiology but now I'm in pathology. I think "You see what you look for, and you look for what you know" holds true in pathology also. Thank you fr replying once again.
0 -
Yes radiology and pathology are very much alike. We both make our diagnosis based upon what something looks like and are therefore subject to variations in perception from day to day and from doc to doc. (Do pathologists also use the term "Aunt Minnie"?)
0 -
Thank you for the reply... And I'm sorry fr reporting late. My biopsy result came back normal. I'm still very new to reach the aunt Minnie level.
I do have fibro cystic and dense breasts.. So there will be more screenings and possible biopsies according to my breast surgeon. My mother's 1st death anniversary is approaching soon. And I am as lost as ever.
I'm almost afraid to ask out loud here.. Before the biopsy I asked the radiologist if he saw anything on the chest wall as I have burning pain in my clavicle and shoulder joints and upper back off and on. He came after a while and told me he saw some symmetrical inflamation on both sides of the sternoclavicular joint and asked if I had arthritis. I told him I didn't.
This wasn't reported on the breast mri BTW. My appt with thr breast surgeon is in March to come up with a plan on how to screen etc.
0 -
I've been in the high risk screening group for a few years because of extremely dense breasts and fam history (mom and sister had bc)....last week I had my first breast MRI...previous mammograms showed no problems.
I was able to see a preview of the report and the images...and even though I work in the medical field and understand that images are not a diagnosis, I'm worried about what I read and saw. I am seeing my BS next week and I know we'll review the report...but 5 days feel very far away right now.
All I know for sure is this...There is "a suspicious appearing irregular enhancing mass", multiple scattered foci (bilaterally) and an area of non mass enhancement almost 2 cm...
If it was just the mass I would know what the plan is... biopsy and wait for the results, but what about the "foci" and "non mass"?
I've tried so hard the last few days to not overreact and stay calm but its getting harder each day.
I'm also afraid I'll be overwhelmed at my appointment so I want to write things down. Any ideas or suggestions on what specific questions I should be asking my surgeon?
1 -
Sarah1975_TO
It would be helpful to see the report in its entirety. Findings on MRI are strongly dependent on context for making a diagnosis. They are also compared with a patient's prior Mammo, US, etc.
That being said, the description of the mass is self explanatory. If it was used properly, on breast MRI "foci" are defined as small round white spots 5mm or less in size. On MRI normal breast tissue is basically composed of large aggregates of "foci", but if seen isolated in the fat, and asymmetric from the other side they catch our eye. Could be normal tissue, could be an extremely early mass. At that size its too small to tell due to the level of spatial resolution on MRI. Likewise non-mass enhancement can be normal or early DCIS.
0 -
Hi Djmammo. I recently had an MRI to check if there were any areas of concern on my breasts besides one 5mm cancerous spot (which I am scheduled to have surgery for in a few weeks) The MRI showed no other suspicious findings, which I am happy about. However the report states "The imaged portions of the chest and abdomen demonstrates bibasilar aterlectasis". I saw this on my report on the portal, my doctor never mentioned it. Do I now have to worry that there is a problem with my lungs?
0 -
That doesn't necessarily mean there is lung pathology present. It can happen on MRI and CT scans related to lying on your stomach or back, and not taking in a huge breath and this kind is seen at the lung bases (both lower lobes). Some abdomen scans with are done with the breath held out, and its really prominent on those. That being said, you should check with your doc just to make sure.
0 -
Djmammo, I am currently weaning from breastfeeding (3mo postpartum). I have found two dimples in my lower left breast. Clear US and 3D Mammogram. How long before I could get a accurate MRI reading should I wait before scheduling one?0 -
For screening mammograms (no mass felt) we usually postponed them 6 months, not sure what the current recommendations are for MRI. If you call the MRI center they should be able to tell you. If there is a mass or a suspicion of cancer, we don't recommend waiting.
0


