Single Hormone Receptor Positive -> ER+/PR-/HER2-
Comments
-
i am 11 1/2 years out with ILC PR- and worry as much as I did since day one. I have a math degree so I see things in some studies that others may not. Yes in my looking I see that PR- doesn’t usually occur after 10 years. But the graphs don’t always show this. I believe IDC Grade 3 PR- doesn’t occur after 10 years. From what I read IDC PR- usually is high grade and has a high KI so it stands to reason it would occur earlier.,,before 10 years. ILC is usually grade 1 or 2..some places do not even grade ILC. It grows slow and is more likely to occur later. The PR- from what I can see does not increase the grade or the rate at which it grows. from my readings ILC PR- is worst then ILC +. ILC is worse than IDC
0 -
From my readings IDC PR- does not usually occur after 10 years. IDC PR- is usually high grade and has a high KI which would make it more likely to occur before 10 years. PR- does not change the grade or KI for ILC. So far I haven’t been able to find any research in what is changed other than it seems to be bad. Some PR- does occur after 10 years..from what I can see. Probably has a low KI...slow grower...like most of ILC...so I am still very worried at 11 1/2 years out
0 -
Well, that was depressing for us ILC people, but I'm glad I read it. May convince me to get on that awful AI.
0 -
 JudyO
JudyOWell that was fun reading. Not sure I understand all the figures except the fact that ILC Er+ Pr- have the worst prognosis.
I dont understand statistics very well.
There are threads in the ILC forum that show that some women with ILC can have complete pathological response to chemo. And we know via Big 98 trial that AI work better than Tamoxifen for ILC.
I am still happily (maybe foolishly) going along with the idea that my PR- tumour was aggressive and the chemo would have done its job. Also happy with the thought that I am on an AI and that will also do its job. I dont ever intend to stop taking it, unless I have to. And as larger PR- negative tumours tend to reoccur before 10 years, ILC or not, I will feel more confident once I get past 10 years.
It must be exhausting still being worried 11+ years later. I feel for you. I am 4 years out and pretty tired of worrying about it all. It's so soul destroying (I am referring only to myself here). Maybe they will find something that works for ILC tumours sooner rather than later, now that they have finally officially admitted that ILC is a different beast than IDC.
The Lobsig is a step in the right direction.
0 -
There is also another ILC stage 3 er+ pr- lady who popped in on her 15th year past diagnosis in the stage 3 forum.
I couldn't figure out if the study took Chemo and Anti hormonal use into consideration. It only mentioned surgery and radiation specifically. I assume women would have had chemo or hormonal therapy or both but there was no mention of how it was included or excluded. So I just dont get how they work these things out.
I am going to just ignore that study. It can't help me either way.
Here's to many many more cancer free years for you JudyO.
0 -
trinigirl50...thank you so much for your kind words. I am a very nervous worrier...so this has been a very long bad thing for me. I wish someone could pull out a crystal ball and tell me I am done with this. I had 2 scares this summer. I flunked a colon guard test and was told I may have colon cancer. The nurse who called me about the results was not well trained. She told me it was almost certain I had colon cancer. After a colonoscopy ..I get them every 5 years but this was only 2 1/2 ..and all was good...I asked the doctor...he said so many are false positives...Then I had a bad back. Oncologist said with 7 positive nodes we need to look into this. MRI was done and all was okay. My Uncle died recently after 19 years out with prostate cancer...and my sister's girl friend just had ILC come back at 15 years...SO being a worrier I was put into high drive. I agree with you that after 10 years we may be good. Couple of things...PR- luminal B has some that have a low KI that have a good prognosis...may be us....and I would think with all the nodes positive it wouldn't wait so long out to recur... also I put faith in arimidex...I had chemo and then 10 years of arimidex...my onc took me off at 10 years...since it was really bad on my bones and can be hard on your heart...There is a girl out 15 years on the ILC thread with PR- she has a large tumor but only one node...so I worry about that...I do remember a girl when I was dx that was ILC PR- with 3 positive nodes who didn't do chemo because her onco testing was so low...so I do believe both of us have a good chance of being around a long time....Judy
0 -
I totally get you. I hurt my shoulder attempting to ski. Tumour markers went up: MO sends me for bone scan and CT. The next year I overdid a walkathon, hurt my hip and lower back pain, I diagnosed myself with bursitis: tumour marker went up, MO sends me for CT and bone scan. Next year I get some kind of stomach bug. TMs go up: I get sent for endoscopy and colonoscopy.
Now my neck is stiff and hurting. I know it's my arthritis, my whole family gets this pain and stiffness in neck (mother and father, brothers and sisters). What do you want to bet my TMs are gone up again. At least by now my MO knows they fluctuate, so maybe it will just be an MRI of the neck this time.
All of these things make it really really hard not to panic. But...
I am pretty sure I am going to be here to see my son into adulthood. That's 8 years from now. And then I am aiming to see a grandchild, which is more like 25 years from now. Why not?
Re many positive nodes, the thinking nowadays (if I read it correctly) is that having many nodes is not indicative of reocurrence of mets per se, it is more indicative of the aggressiveness of the initial tumour (which is indicative of reoccurrence). So I dont freak out too much about the number of nodes I had anymore.
At any rate I cant change anything so I am doing my best to keep busy and when I start down the dark tunnel I go binge watch something like The Office.
My great aunts were: 106, 98, 94 and the youngest died at 84. My sister and I are aiming for our 90s.
0 -
Think you are right about the nodes...my onc told me my tumor was aggressive since it hit the nodes...but then I wonder about the grade 1 of my tumor ..always those questions My breast surgeon thought my tumor was very slow growing and had been around for a while..was that why it was in the nodes???Judy
-1 -
I think so, it was probably there for a long time. Many women die of old age with undiagnosed breast cancer because of how slow some tumours can grow. I think I had LCIS about 15 years ago, I couldn't get milk out of my left breast to breastfeed my son. I didn't think much about it. Then I had mammogram and US every year because of dense breasts and they always showed 3 small supposed benign fibrodaemas in my left breast that didnt change over the years.
In 2013 I did feel a small pea like lump that moved around. I had mammogram and US but they said it was nothing. In 2014 I decided to go on HRT due to horrible perimenopausal symptoms. That was a big mistake. Literally 2 months later my breasts got bigger (both) but in another 2/3 months I noticed my left breast was really swollen and odd looking. And then the nipple flattened. I got another mammogram and US but they still said nothing to be seen. I demanded a biopsy and it was agreed because of the changed shape of my breast (I could actually see that my skin was being pulled in). I think I had an initially slow growing tumour that I fed with the HRT, and it went berserk. My breast was small so it had no where else to go but to my nodes. I was extremely lucky to have got it when I did.
Or extremely unlucky to have fed it depending on your point of view. I consider myself lucky.
Anyway, that's my story.
I might have still developed ILC 20 years from now, but I think the HRT is what changed mine to become so aggressive. Who knows? I am just making personal educated guesses.
Good luck to you. I am taking a break from the boards and all things BC for awhile. I think I need to give myself some distance as my anxiety levels have started rising again.
Be well and good luck!
0 -
Good evening,
This may seem odd, but I just discovered that I was weakly ER+. I had been a Tamoxifen for six months and now Arimidex for a 18months. I was having a 3 month follow-up and asked the question what % ER+ I was. Anyone here taking anti-hormones who as also weakly ER+?
0 -
Hi humble, yes there are several of us. On pathology staining I was 100% ER. Oncotype I was much lower. This often goes along with being PR neg or close to it. I have been on arimidex for over 18 months now. I would be alot more excited about taking it if I was strongly positive on both but I'm plugging along. Hope you are feeling ok
0 -
Humblepeace- I am 3% ER +. I have been on Exemestane for 2 1/2 years.
0 -
Thanks so much for the responses. I’m more encouraged now. I hope to hear from others 😀
0 -
Me, too. I was 62% ER+ on pathology but ER negative on the oncotype. I'm on tamoxifen, though, because I already had bone loss. My MO said if I was even 1% ER positive, I should be on endocrine therapy.
0 -
Thanks everyone. I’m both upset that I didn’t have this information in the beginning, but also somewhat relieved because I would have been stressing over being TN. I was not told until I recently asked the percentage of ER* I was. Did I miss this initially or was he not a good communicator??? Moving forward I need to ask a million questions and not assume anything!!!
0 -
humble, in my case it was most obvious in my oncotype report then I asked a few more questions. I often wondered if that was because it doesn't effect the treatment path too much (unless really low ER then chemo is thrown in the mix) .
1 -
My initial patho on the biopsy was 10% but after my oncotype came back negative, they redid the patho - I think on the tumor itself rather than the biopsy sample but I'm not sure - and said it was very low. I can't remember if they gave me a number the next time. No tamoxifen or AIs for me.
0 -
Hi everyone,
This thread is super interesting and a bit scary. I'm newly diagnosed and 39 years old, premenopausal. On its face my pathology was ER/PR + and Her2- but then my MO explained to me that while my ER was > 90% positive while my PR was only 1% positive with “moderate" staining and she's concerned about this. I don't know where this leaves me. I had a bilateral double mastectomy with clear margins and clear nodes. I am stage 1B, grade 2 and also had a whopping 13cm if DCIS. Mucinous features of the IDC were mentioned but different doctors seem to have different takes on that as it is not pure mucinous apparently. Oncotype came back in the intermediate range. MO said my case is not straightforward. I guess I'm here to learn and mostly looking for support and encouragement! I'm glad to hear you other ladies are doing well.
Edit: I guess I’m also confused in terms of the Oncotype report if ER and PR that it looks as if some of you are referring to. Mine states 9.8 ER positive and 6.7 PR positive and 10 HER2 negative. Can anyone explain to me what this means
0 -
KeepingCalm,
The Oncotype test measures ER, PR and HER2 using a different methodology than the IHC testing that is usually done in the pathology lab. So the results aren't the same but hopefully the findings are comparable (but sometimes they are not, which is where it gets interesting).
I pulled this from a sample Oncotype report:

The Oncotype methodology considers ER to be positive if it is in the range of 6.5 to 12.5. Your 9.8 is just above the middle of the range, suggesting that the Oncotype methodology did not find your ER to be as strongly positive as the IHC testing (>90%) from the pathology lab. On the other hand, the Oncotype methodology reports PR to be positive if it is in the range of 5.5 to 10.0. Your PR, at 6.7, is towards the low end of that scale but would nevertheless appear to be more positive than the 1% from the pathology IHC test.
As for the 10 on the Oncotype HER2 scale, you can see that HER2 is negative if it falls in the range from <7.6 to 11.5. So consistent with your IHC testing, you have a true negative, probably equivalent to an IHC test result of HER2- 1+. From the Oncotype scale it appears that 10.7 to 11.5 would be considered equivocal, similar to an IHC 2+. Normally with a 2+, further testing is done (a FISH test) to clarify if the HER2 result is positive or negative. On the IHC test, both a 0 and a +1 are considered HER2-.
Hope that makes sense.
0 -
Hi Beesie,
Your explanation is so very helpful - thank you! Your comment about the Her 2 is spot on. It was in fact found to be negative and designated +1. My oncologist said my case is not straightforward, which makes me nervous. Had an oncotype come back in the intermediate range but she thinks that might be an underestimation because of a 2 week clinical trial I was in on a drug that likely substantially lowered Ki67 before surgery and could have impacted other proliferation markers used in the Oncotype. (My presurgery biopsies missed the tumor and only identified DCIS so we don’t have the option of comparing/testing the biopsy sample!). She’s recommending chemo which I will do but what I’m learning about low PR is unsettling!
Thank you again
0 -
I, too, had discrepancies between my pathology and ONCA = pathology, ER+ 99%; PR + 60%; ONCA; ER + 6.8; PR - 4.7. While I understand the two labs are using two different testing protocols, I don't understand the significant differences in results. Especially since my oncologist (and it seems others, reading this thread) rely more heavily on the ONCA results than the pathology. I raise this because my cancer was very small and found "by accident" (they went to biopsy one area, which turned out to be benign and saw the small cancerous spot under the magnification - hidden by calcifications)., and because of COVID 19, the hospitals were advocating for me NOT to have surgery and since the tumor was grade 1 (score 4), they were recommending I go on Tamoxifen and wait until they deemed it "safer" to be in the hospital environment. I pushed and got the surgery anyway. But it scares me that that decision was based on data the doctors seem to no longer be relying on.
0 -
I am 61 and recently diagnosed IDC Stage 2b, Grade 2, ER 95%, PR 3%, HER2 -, and high KI-67. Is there anyone with similar or almost similar stats? I'm starting to research and will get 2nd and 3rd medical opinions.
I'm concerned about the negative progesterone and if that affects the effectiveness of endocrine therapy letrozole femara.
Besides that, I'd like to know if chemo therapy was recommended and if so, which protocol?
My core biopsy was a few weeks ago. I don't know if it's too late to get an Oncotype test for it but I understand from posts that PR - can raise the score to recommend chemo. Was that the case for you?
Were you recommended to have lumpectomy/radiation or mastectomy?
Also what tests did you have? Besides Oncotype, I've heard of Mammaprint, Foundation one, and Guardant 360. Others? Thank you.
edit to add %
0 -
Hi Marguin,
My situation has somewhat similar stats but I am 39. Mine was IDC, grade 2, stage 1B >90% ER+ and 1% PR+, HER2-. My Ki67 was low but my MO feels this is not reliable because I participated in a short presurgery clinical trial that might have lowered it. My MO was definitely concerned about the essentially negative progesterone in my case combined with my age. I also had extensive DCIS and my Oncotype score came back just into the intermediate range for my age but again the MO wonders if that might have been an underestimate because of the study I was in. So, mastectomy was recommended at least for the effected breast because of the extensive DCIS and I decided to have a bilateral mastectomy with immediate direct to implant reconstruction. Because of my Oncotype, essentially negative PR and my age, my MO recommended chemo and I’m fortunately halfway through 4 cycles and doing well all things considered. Because of mastectomy and clear lymph nodes I won’t need radiation. Feel free to PM me if I can provide any other helpful info. Navigating treatment decisions is definitely nerve racking and I was very anxious leading up to my surgery but it is true now that I am moving along through chemo I have adjusted and it’s not fun but manageable as my MO promised
0 -
KeepingCalm, Very similar tumor stats. It seems like lots with very high ER + and negative PR - had mastectomies, radiation, and chemo. Good to hear you won't need radiation. Over time it looks like more tailored responses are becoming a reality.
0 -
Ladies, I didn't know there is a problem when you are ER+ only. My test results are:
ER: POSITIVE (90%, MODERATE)
PR: NEGATIVE (<1%, STRONG)
HER2: NEGATIVE (1+)
None of the MO I met mentioned that may be a problem at all. Why would be more difficult to treat than ER+ and PR+?
0 -
Hi Lily,
My understanding was not necessarily that it's more difficult to treat (My MO said she knew how to treat me with chemo just knew that I would be disappointed to hear chemo.) but that there's some evidence to suggest it's more likely to be aggressive or potentially come back without more aggressive treatment. My MO said assessing my level of risk in this regard was tricky because I had some factors that fell into the lower risk category but that the low PR fell into a more concerning category. I think these stats may fall into the Luminal B category which apparently can have slightly worse outcomes than Luminal A which I understand to be strongly ER and PR+ and maybe more likely to be treated effectively with just hormone treatment. But of course, treatment decision making is all individualized based on multiple factors - mine just happened to lead to chemo unfortunately.
Marguin, mastectomy was largely driven by the large amount of DCIS I also had - almost the entire breast - not by the hormone receptor status. In fact in my case we didn't know for sure that the IDC was there until surgery because the biopsy missed it which was an emotional roller coaster in and of itself. I was led to believe I might have had surgery and be done if just DCIS but now I'm doing chemo and will do some form of hormone therapy as well. It's been quite the year needless to say.
0 -
I just happened to come across this relevant study which discusses treatment and outcomes according to differing ER/PR status. It looks like the ki67 value is also highly important.
0 -
Yes, that’s exactly the piece of research I was thinking of. In my case, we don’t know the Ki67 for sure because it may have been lowered by the presurgery trial I was in and unfortunately we don’t have a biopsy sample to test because the biopsy missed the IDC - so frustrating! But, I’m halfway through chemo and I guess for what it’s worth in my case will at least never wonder what if in terms of doing chemo or not.
0 -
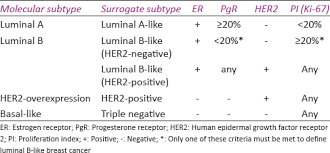
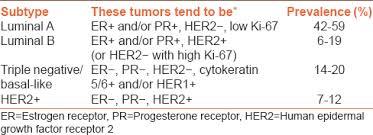
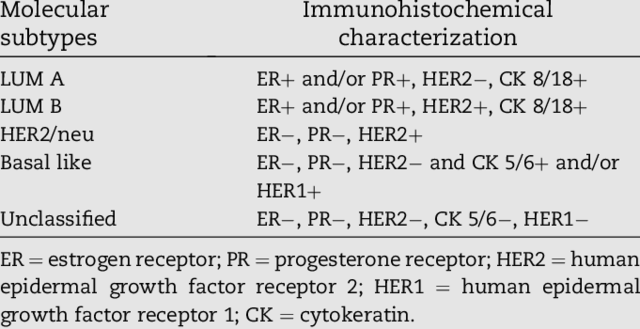
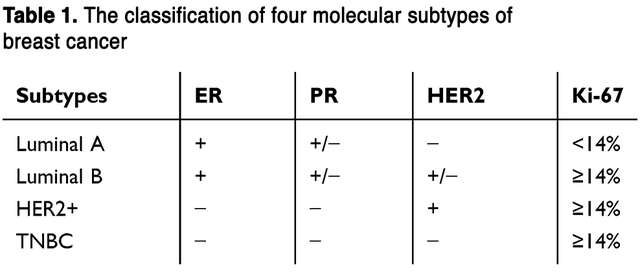
KeepingCalm, I think that some doctors automatically assign all PR- tumors as being Luminal B, and therefore assume a worse prognosis.
But what is interesting is that there appear to be many definitions of what is Luminal A and what is Luminal B. One definition puts all PR- cancers that are ER+ and HER2- in as Luminal B. But others allows for a PR- cancer (that is ER+ and HER2-) to be classified as either Luminal A or Luminal B depending on the grade and Ki-67.
Within this second definition, if the Ki-67 is low and the tumor is either grade 1 or grade 2, then the cancer will be Luminal A. However if the Ki-67 is high (generally considered to be >15%) and the tumor is grade 3 (or possibly grade 2 if the mitosis score is a 3, since mitosis is an indicator of high proliferation) then the cancer will be Luminal B. Most low PR / PR- negative cancers have high Ki-67, so most will be Luminal B, using this definition. But not all.
To my understanding, Luminal B defines tumors that have higher proliferation, higher grade and are more aggressive. Luminal B cancers are more likely to be larger and node positive. So if a patient has a tumor with low or negative PR, but it doesn't meet any of the other criteria for being Luminal B, it seems to me, as a layperson and patient (and PR-, with a small lower grade tumor) that the more flexible second definition makes more sense.
This article talks about the various definitions of Luminal A and Luminal B: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4656721/#!po=29.0698
And in a very quick search, here are 4 charts that show different definitions of Luminal A and Luminal B. I'm sure I could easily find more that are different again.
No wonder we, and are doctors, are confused.
 0
0 -
Oh boy! I am clueless
 )! I don't have Ki-67 done. I just can't get the concept of difference of cancer cells that get fed by ER alone or ER & PR. It seems that one or both hormones feed them and once you remove the hormones, hopefully being in the lucky 50% the cancer cells won't get fed and won't multiply. I wonder why it should be a difference on the type of the hormone. 0
)! I don't have Ki-67 done. I just can't get the concept of difference of cancer cells that get fed by ER alone or ER & PR. It seems that one or both hormones feed them and once you remove the hormones, hopefully being in the lucky 50% the cancer cells won't get fed and won't multiply. I wonder why it should be a difference on the type of the hormone. 0