Are you aware of anyone with LCIS who got Stage 4 Breast Cancer?
Comments
-
True, Leaf, the overall LCIS #s are low. Anecdotal evidence is never as reliable as research. My own doctor, who has been practicing 25 years in a metropolitan area could not recall a previous case. I know we are about 4 at most in 100,000.
If you care to respond, has your recent biopsy experience caused you to reconsider your treatment options or take more drastic measures?
Thanks for that link.
0 -
No, not really. I've already taken 5 years of tamoxifen, so the only other major option is bilateral mastectomies. I have another condition which makes healing more difficult, so that makes that more problematic.
0 -
Thanks for the info Leaf and let's hope the scary biopsies are now done for good.
0 -
so, I had LCIS that developed into a tumor. Not knowing what caused the tumor they did a lumpectomy. They got the entire tumor, no node involvement. But after finding the LCIS, knowing my risks, I opted for a bilateral mastectomy.
Followed by Lupron shots, then ovary/ tube removal and meds for the next 10 years, because the tumor was loving my hormones... lol
So, am I understanding this correctly, the chances of me getting late stage cancers or metastases is very low???
Or did I miss something??
Thanks!
0 -
Hi all, I got results back to today from the MRI guided biopsy. Everything was fine. I'm so relieved. Thanks for listening.
0 -
faithhopelove - Yay!!! So glad to hear the biopsy was benign!
0 -
Faithlovehope, wonderful news!
0 -
Thank you, Pegasus and Lea, my report said dense breast fibrosis. Follow up with another MRI in six months. At my last MRI I needed to read and sign a sheet that was new. It talked about the contrast dye and how it "generally leaves the body in 3 days" but can be known to stay in tissue such as the BRAIN for YEARS. What's this now????? Anybody else know about this? Enjoy your weekend ladies!
0 -
Good report, Faithopelove! Gadolinium is used in breast MRIs and other MRIs to enhance what is seen. Questions about its safety are now being raised. This is a very helpful document.
https://www.itnonline.com/article/debate-over-gado...
3 w's then dot then itnonline.com/article/debate-over-gadolinium-mri-contrast-toxicity
Excerpts from this linked document:
"Radiologists and patients began to question the safety of gadolinium a few years ago when a study came out in late 2014 showing the agent is deposited and retained in the brain.[1] This, combined with a small percentage of patients who claim their health was harmed following gadolinium exams..."
"It is known that patients with renal insufficiency cannot filter the gadolinium from their body, so it is included as a U.S. Food and Drug Administration (FDA) warning label on the contrast packaging. But, there has been little evidence showing patient safety issues in those with normal renal function."
"November 2017...action movie actor Chuck Norris filed a lawsuit against a contrast vendor and the contrast distributor for allegedly poisoning his wife Gena. She had several contrast MRI exams and the suit alleges numerous adverse health effects began after these exams. Norris is seeking $10 million in damage." %%%%THIS IS THE BIG DRIVER OF THE CHANGES WE HAVE SEEN IN WHAT WE SIGN AND IN INVESTIGATIONS INTO THE SAFETY OF THE DYE%%%%%
"Physicians have largely been reluctant to directly link gadolinium agents to these maladies, because there is little clinical evidence showing a direct correlation. Symptoms can also vary greatly between patients reporting problems. Gadolinium contrast agents have been used in hundreds of thousands of patients over the past couple decades and the clinical evidence shows it is safe in most patients...Until the past few years, it was not widely known that the gadolinium accumulated and was retained in tissues, especially the brain...It was previously thought the agent was entirely excreted from the body.. A couple large scale studies are underway, but it will take time to gather data to determine the long-term effects of gadolinium retention.
"I am not completely convinced gadolinium is not toxic," Kanal [Emanuel Kanal, M.D., director of MRI services and professor of radiology and neuroradiology at the University of Pittsburgh Medical Center] said. "I don't know which way to turn yet. The issue is a lack of data showing toxicity, but lots of data showing it is safe."
"Sheela Agarwal, M.D., U.S. medical affairs, Bayer Healthcare, who spoke during a Bayer-sponsored lunch at RSNA on the topic of gadolinium safety...said there have been about 50 studies that have come out on this subject in the past few years, but none of them offer a smoking gun showing gadolinium retention leads to chronic disease."
"What is the FDA Doing About Gadolinium Toxicity Concerns? The FDA agrees that more research is needed and there is not enough evidence to impose a regulatory clampdown on GBCAs. In September 2017, the FDA's Medical Imaging Drugs Advisory Committee (MIDAC) voted overwhelmingly to recommend new labels on gadolinium-based contrast agents (GBCAs) warning of the possibility of gadolinium retention in the body"
"The FDA stated there is no clinical evidence that directly links gadolinium retention to adverse health effects in patients with normal kidney function, and the FDA has concluded that the benefit of all approved GBCAs continues to outweigh any potential risks."
"The health consequences, if any, are as of yet entirely unknown, and so far there are no known consequences of retained gadolinium," Kanal [Emanuel Kanal, M.D., director of MRI services and professor of radiology and neuroradiology at the University of Pittsburgh Medical Center] said. "It does not mean that there are none, it just means that we don't know of any at this stage and more studies are needed."
"However, in July 2017, the European Medicines Agency (EMA--European Medicines Agency) issued a final opinion that recommended restricting the use of some linear gadolinium-based contrast agents (GBCAs) and suspending the marketing authorizations of others, citing concerns about gadolinium deposition.[5] But, the EMA said it supports the continued use of macrocyclic GBCAs. The EMA stated "there is currently no evidence that gadolinium deposition in the brain has caused any harm to patients.
"The EMA recommended suspending the marketing authorizations of GBCAs Magnevist (gadopentetate dimeglumine), Omniscan (gadodiamide) and OptiMark (gadoversetamide). The group cited the benefit-risk balance is no longer favorable for certain linear GBCAs. But, the EMA recognized certain linear GBCAs are still needed for liver imaging, so retained Primovist (Eovist in the U.S., gadoxetate disodium) and MultiHance (gadobenate dimeglumine)."
"There are two classes of GBCAs based on their chemical shape — linear and macrocyclic agents. Agarwal (M.D., U.S. medical affairs, Bayer Healthcare) said there are four studies[6,7,8,9] that have shown linear agents have more retention in the brain than macrocyclic agents. However, recent studies have also shown all agents, including macrocyclic, leave gadolinium behind in the brain to some level. While deposition in the brain has been the main reason for concern in recent years, she said in animal studies, there was 100 times more gadolinium retained in skin and bones than there was in the brain. SEE LIST AT END
>>>HERE IS WHY YOU ARE BEING ASKED TO SIGN SOMETHING. I HAD TO SIGN IT TOO.<<<
"Some practices are looking into informed consent documentation, but others do not want to do this because of fears it may open the door to litigation"
I don't have the source, but I copied this into my own Gadolinium files:
The macrocyclic agents are shaped like cages around the gadolinium ion and have a lower probability of releasing free gadolinium. They are considered more stable than other contrast agents and have a lower risk of NSF-- Nephrogenic systemic fibrosis. The linear nonionic agents are the least stable, and the linear ionic agents have intermediate stability. For example, the vast majority of patients with NSF have been exposed to the linear nonionic agent, Omniscan (gadodiamide), even though it only has about 15% of the worldwide market share of gadolinium-based contrast agents.
-------------
I will be asking specifically what kind of Gadolinium is being used in my MRIs, and will consult the list at the bottom. I've had one MRI only so far. I have asked several docs about Gadolinium over the past 18 months and here are the responses.
Gynocologist--"Do they need dye for breast MRIs? I did not think they did."
This response surprised me and shows how localized doctors' knowledge can be. Dye IS used for breast MRIs.
Breast Surgeon--"An MRI without gadolinium is not worth doing. The safety is something to consider." When I became a little desperate, maybe a little hyperventilating and said something like, "All the more reason to remove my breasts if I can't do MRIs now because they are not safe which takes away one of my best weapons for early detection," the surgeon very nicely let me know she thought I was way over reacting and the benefits still outweigh the risks.
Family doc--"This risk is low. Keep doing your breast MRIs."
Cancer specialty and research center--"We use the safest gadolinium. We do not see problems with it." This is where I got my one and only MRI. But I plan to do annual ones there.
Nurse Practitioner specializing in high risk for breast cancer--don't remember her exact words be she felt it tipped the balance away from doing annual MRIs over a lifetime, but the occasional MRI was still ok.
One of the professionals, but I don't remember who and cannot find it written down said, the biggest concern is for MRIs OF THE BRAIN, not so much for other areas.
The List from the linked article
Linear GBCAs:---shown as more dangerous--
Ablavar (gadofosveset trisodium)
• Eovist (gadoxetate disodium)
• Magnevist (gadopentetate dimeglumine)
• MultiHance (gadobenate dimeglumine)
• Omniscan (gadodiamide)
• OptiMark (gadoversetamide)Macrocyclic GBCAs:---little less dangerous---
• Dotarem (gadoterate meglumine)
• Gadavist (gadobutrol)
• ProHance (gadoteridol)"It's always something" ~Roseannadanna
(in retrospect, a rather poignant quote, considering the source)
0 -
This is very concerning to me as I have had many MRIs. Ugh. Thanks for this research Lea7777
0 -
Good info as usual, Lea7777. Comments from the various professionals that you’ve encountered is always interesting Thanks for posting.
0 -
I posed a similar question to the title of this post again last week to a NP who went over MRI results with me. I actually asked her how many women with atypia had she encountered who eventually died due to breast cancer. She said she thought it was none. She added that her practice had followed many women with atypia over many years. The NP was probably 50-ish.
0 -
Lea,
I"m not sure that polling one NP in one practice will give you any reliable information. Similarly, I don't think that polling even the BCO group, and those among it who might answer, would give you reliable info either.
Also, just for the record, asking how many people died is just a little bit offensive for those of us who DO have stage IV disease. This is something that is in our minds 24/7.
If you want reliable information, you might try researching on PubMed for actual research articles. The information is much more reliable.
The reality is that, according to current statistics, about 1/3 of people who are diagnosed with any type of breast cancer will go on to Stage IV. Those stats have not changed very much over the years. I was originally diagnosed with LCIS in 1990/1991. In 2003, I was diagnosed with invasive lobular cancer. In 2006, I was diagnosed stage IV with a single site metastasis. It didn't spread further until 2019, and I now have lobular cancer in my liver and my skeleton. So if you want proof that LCIS can spread, there you go.
0 -
BevJen, not to take away from the main point of your post, but I do think it's important to mention that there is evidence that "1/3 of people who are diagnosed with any type of breast cancer will go on to Stage IV" is no longer true. The percent of early stage patients who progress to metastatic disease appears to be in decline, possibly quite significantly.
"The observed fifty percent relative decline in distant breast cancer recurrence over time may be related to both improved treatment for initial disease at diagnosis decreasing recurrence risk (hormonal therapy, polychemotherapy, dose-dense chemotherapy, taxanes, and trastuzumab) and stage shift to more early and less late stage disease at diagnosis with improved screening technology and screening program participation. Distant recurrent disease incidence decline over time differed by phenotypic characteristics. We observed a 70% decline in distant disease recurrence among hormone receptor-positive patients and a 50% decline among hormone receptor-negative patients over time. We observed a 60% decline in distant disease recurrence among HER2 positive patients from 1999 to 2006. The differential decline associated with phenotypic subtype creates a new profile of recurrent metastatic breast cancer with fewer HR and HER2-positive cases and relatively more TNBC cases. Ten-year cumulative incidence comparisons to accommodate the longer interval to distant recurrence among HR-positive versus HR-negative disease did not significantly differ from 5-year rates."
From Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990–2010, here's a graph showing, over 3 time periods, the percent who have developed recurrent MBC, by stage at time of initial diagnosis: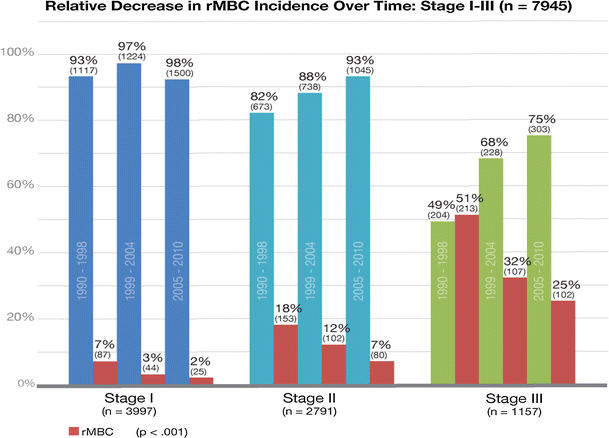
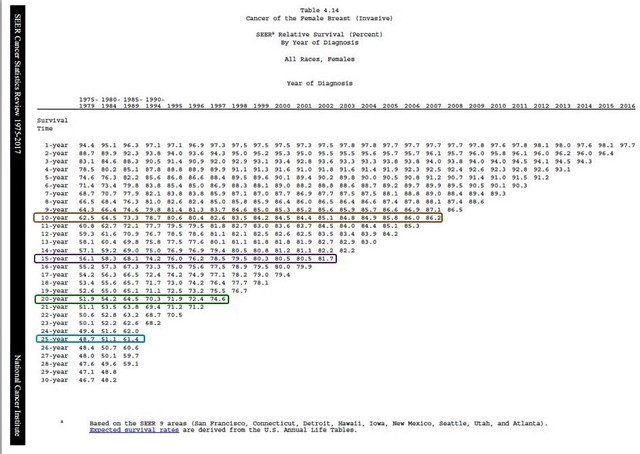
And while the following chart doesn't directly show the percent that have progressed from early stage to metastatic, since the percent who are diagnosed Stage IV de novo has remained constant, long-term survival data does reflect this figure. This is the most recent SEER survival data, based on year of diagnosis. I have highlighted the lines that show 25-year, 20-year, 15-year and 10-year survival, and you can see the significant improvements in these figures. Sorry that the chart isn't more clear.
 0
0 -
Beesie,
No offense taken. Thanks for the charts.
0 -
I think doctors use some other databases where they get their data to let us know the chance of recurrence. Also, depends on the node involvement. I mean Stage 1 no node is different from Stage 1 with node involvement I was told.
Getting back to LCIS, it is a very tricky one. Many times it is missed even from the most advanced scanners out there. In my case, it was missed from the mammogram and MRI with contrast. If it stays in the breast, it may get out of lobules and you got ILC. On the positive side, knowing you have LCIS keep your doctors on the toes to be aware of any other symptoms.
0 -
BevJen, thank you for your personal account and sharing what you have actually experienced. None of my questions to medical professionals or my posts here are ever meant to be offensive, so I apologize for any insensitive words. I do want to share the exact quotes of both questions and answers whenever possible and when I can remember them. I wish you good health and hope you can continue to share your story and perspective on this site, as it is bound to be helpful and insightful to others.
0 -
Continuing with my completely unscientific "poll" if you can even call it a "poll," I asked the oncologist at my checkup appt today, "How often do you see women with LCIS or other atypia go on to advanced stages of cancer or die?" His answer covered two concepts.
First, he stated that in 28 years he had not known of such a case. He added that he also never recalled any colleagues mentioning a case during their weekly meetings and discussions. He attributed that lack of severe outcomes to vigilant screenings that caught cancer early in the cases where atypia did lead to cancer.
Second, he stated he personally dealt with only a couple of LCIS or other atypia cases because so few women at high risk for breast cancer take any type of adjuvant therapy. As an oncologist, he only sees people who are on these drugs. "It's a very small percentage" is how he described the number of high risk patients who opt to take these adjuvant drugs. (I take Raloxifene.) His comment exactly matches all the studies and research I've found that not many women at high risk for breast cancer take these drugs (1 in 7, 8%, under 10%, 25% in clinical trials with oversight, etc.). The oncologist did not seem alarmed by the low number and emphasized the importance of screenings.
0 -
May I chime in on the 1/3 of breast cancers becoming metastatic? One third or thirty percent of breast cancers metastasizing is a figure found all over as a standard fact that I have always believed. It is in the American Cancer Society info and even on big charts in my doctor's office. I have repeatedly asked all the breast professionals I've encountered about this stat with alarm. I've shown them this equation: If my chances of invasive breast cancer with LCIS are even 20% over a lifetime and 1/3 of all cancers metastasize, then I have a 20% x 1/3 = 6.7% chance of metastatic cancer, and that's way too high.
The response has uniformly been that the 1/3 figure has to be taken with a grain of salt; that it's not accurate; that it depends on so many other circumstances; that it's no longer true. Bessie, the charts you've provided us are in line with those comments.
0 -
Lea7777,
Interesting about taking preventive action. When I was diagnosed in 1991 with LCIS, none of these preventive drugs were even around. Thus, watchful waiting was the only way to go. Georgetown Hospital was starting a trial on tamoxifen for such patients in the early 90s. I was going to go on the trial, but when I went through all of the paperwork, it just scared me and I didn't see an absolute advantage for me to go into the trial, with all of the side effects they were talking about at that time. My bad -- it may have helped me, who knows?
As for vigilance screenings, from the time that I was determined to have LCIS, I saw my breast surgeon and had a mammo every six months, until I was diagnosed in 2003 with invasive lobular cancer. So I don't think his response holds any water at all. In fact, less than 6 months after a mammo and screening with my breast surgeon, I discovered my ILC, and my breast surgeon was gobsmacked. She really couldn't believe it. At the time, she was the best breast surgeon in DC.
0 -
And I am gobsmacked reading your account, BevJen! How frightening for you. Hoping all that is behind you now.
0 -
Hi, Lea7777,
No, not behind me. See my treatment history below my post. I had a reprieve from 2006-2019, but now back in active treatment.
0 -
Yes, I do see the 2019 and 2020 entries, BevJen. Thank you for bringing that to my attention. May 2021 bring no more health issues for you.
0 -
KItKit, Hello! How are you today? Can you update us since you were last here having just been diagnosed with stage 4? I like to know how you are feeling and how things went with the trial at UCLA. I hope you are doing much better.
0