"Tamoxifen Road" - Support and Encouragement
Comments
-
Tamoxifen can cause NON-ALCOHOLIC FATTY LIVER DISEASE so please be sure your team monitors liver enzymes routinely.
0 -
Here are some links to studies and information. I just think SO many BC patients need to be aware of the potential risk to our livers with Tamoxifen. My MO never talked about this with me. I found out about the risk from others.
Hugs and healing to all.
--------------
(cross posted)
I'm just going to add this link, it goes to a thread where a member posted her experience with Tamoxifen.
I feel like anyone deciding on this hormone treatment should be aware of possible damage and risk to their liver, as I was never made aware of this by my MO or team.
Please, as her story illustrates, at the very least, before starting Tamoxifen, have a liver enzyme test run. Better safe than sorry and needing a liver transplant because of the damage!
(Reference post is written by CanadaLiz on 12/15/2018)
https://community.breastcancer.org/forum/78/topics/868854?page=1#idx_29
Symptoms to be aware of:
https://www.breastcancer.org/treatment/side_effects/liver_probs
Here are a few studies for info:
A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462391/
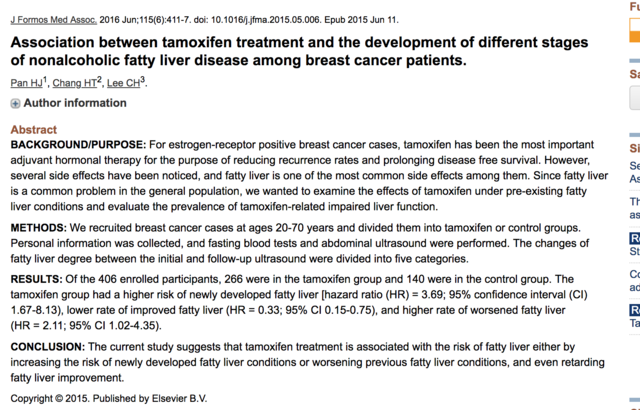
"In addition, fatty liver disease, also known as non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH), was observed in more than 30% of patients with breast cancer who received tamoxifen as adjuvant therapy.10,11 The first anastrozole-induced hepatotoxicity case was reported in 2006.12 A retrospective study demonstrated that fatty liver disease detected using ultrasound was more frequently seen with tamoxifen than with anastrozole (30.4% vs 6.25%).13 "Association between tamoxifen treatment and the development of different stages of nonalcoholic fatty liver disease
https://www.ncbi.nlm.nih.gov/pubmed/26071793
https://www.sciencedirect.com/science/article/pii/S092966461500176X
"Several studies showed that taking tamoxifen may incur a 30–40% risk of developing nonalcoholic fatty liver disease(NAFLD), according to different diagnosis instruments."ConclusionThe current study suggests that tamoxifen treatment is associated with the risk of fatty liver either by increasing the risk of newly developed fatty liver conditions or worsening previous fatty liver conditions, and even retarding fatty liver improvement."
"Our study suggests that tamoxifen is associated with the risk of NAFLD development, either by increasing the developed fatty liver or worsening the previous fatty liver condition and even retarding fatty liver improvement. The severity of fatty liver is associated with higher rates of abnormal LFT. During the follow-up period, regular abdominal ultrasound checkup, not just for detecting liver nodules, but also for identifying fatty liver change, is crucial. Further checking of liver function and other metabolic conditions once the fatty liver condition has progressed is essential."
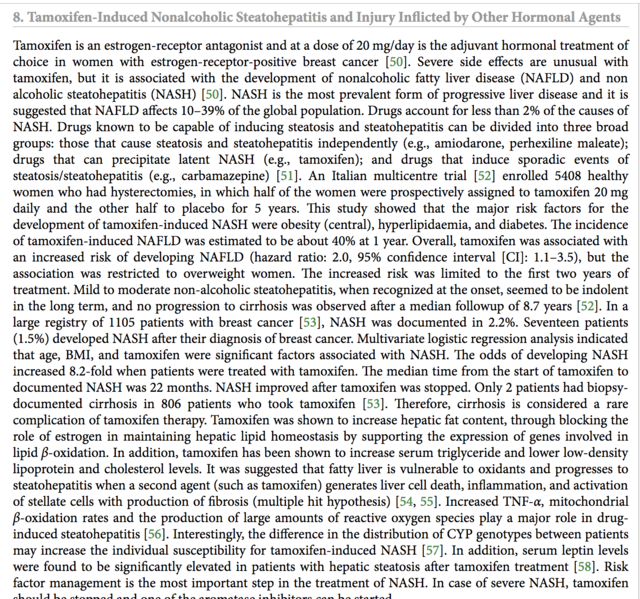
Drug Record: Tamoxifen
https://livertox.nih.gov/Tamoxifen.htm
"Outcome and ManagementWhile fatty liver arises in at least one third of women treated with tamoxifen for up to 5 years, clinically significant steatohepatitis is less common. Nevertheless, monitoring of serum aminotransferase levels during tamoxifen therapy is appropriate. In women with persistent elevations in ALT levels, the relative benefits and risks of continuing tamoxifen therapy must be weighed. Factors to help in the decision, include noninvasive tests for hepatic fibrosis (platelet count), imaging of the liver and, in some instances, liver biopsy. Other approaches short of stopping tamoxifen therapy include nutritional advice and weight loss, abstinence from alcohol, and possibly medical therapies for nonalcoholic steatohepatitis (which are currently investigational and have not been shown to be specifically helpful in tamoxifen induced fatty liver). The possible development of serious hepatic fibrosis and portal hypertension can be assessed noninvasively by serial determinations of platelet count, but may require liver biopsy to document."
Tamoxifen induces hepatotoxicity and changes to hepatocyte morphology
https://www.spandidos-publications.com/10.3892/br.2015.536
"Clinically, patients who accept the endocrinotherapy are instructed to reexamine their liver function every 4 months due to its hepatotoxicity. Numerous research and clinical studies have illustrated clearly that TAM causes the inhibition of mitochondrial β-oxidation and subsequently leads to macrovacuolar steatosis (21,22). The early symptoms were characterized by the presence of a single, large lipid vacuole within the cytoplasm of the hepatocytes (23)."
"In conclusion, the present data showed that a relatively low concentration of TAM (6 mg/kg/day) for a short time treatment (2 weeks) would cause hepatotoxicity and change morphology at the microscopic and ultrastructural levels. Although the liver function may compensate or reverse the injuries gradually, the damage that occurred in the short-term TAM therapy has been shown. Thus, there is a necessity to obtain measures for monitoring liver function and protection at the early stage of the TAM endocrinotherapy, prior to apparent and undesirable clinical symptoms occurring. Furthermore, as DNA damage also occurs at this early period without clear clinical symptoms, which in the long-run increases the risk of hepatocarcinoma, exploring alternatives for TAM in long-term clinical endocrinotherapy is required."
Liver Injury Induced by Anticancer Chemotherapy and Radiation Therapy
https://www.hindawi.com/journals/ijh/2013/815105/
Death due to liver failure during endocrine therapy for premenopausal breast cancerhttps://www.tandfonline.com/doi/full/10.3109/0284186X.2010.484813
"In the tamoxifen product information, liver-related side effects are listed and it is recommended to perform periodic liver function tests, although in clinical practice blood tests are no longer performed routinely during follow-up for women with early breast cancer."
"Young women, in particular between ages 26 to 35, seem to be—for yet unknown reasons—more frequently affected by acute liver failure, and the use of antidepressants (metabolized primarily via liver enzymes CYP 3A4, 2D6, 2C19), other potentially hepatotoxic drugs (e.g. acetaminophen-type analgesics and NSAIDs), and alcohol are more frequent in younger breast cancer patients than generally presumed and reported. We therefore advise physicians to pay special attention to patients treated with endocrine therapy for breast cancer who have concurrent depression and who potentially or actively consume hepatotoxic drugs and alcohol. Such patients should have their liver function monitored and liver imaging should be performed if indicated."
The Association of Nonalcoholic Steatohepatitis and Tamoxifen in Patients With Breast Cancer
https://onlinelibrary.wiley.com/doi/pdf/10.1002/cncr.24374
A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer
https://pdfs.semanticscholar.org/3aa1/d236d38c20f3a9377dea6f9d5ad8235221c6.pdf
G.L.O.W.N. - Tamoxifen
https://www.glowm.com/resources/glowm/cd/pages/drugs/t002.html
"Effects on lab test results
• May increase BUN, calcium, and liver enzyme levels.
• May decrease WBC and platelet counts.Special considerations
• Tamoxifen acts as an antiestrogen. Best results occur in patients with positive estrogen receptors.
• Adverse reactions are usually minor and well tolerated. They usually can be controlled by dose reduction. ALERT Serious, life-threatening, or fatal events associated with tamoxifen in the risk reduction setting include endometrial cancer, uterine sarcoma, stroke, and pulmonary embolism.
ALERT Serious, life-threatening, or fatal events associated with tamoxifen in the risk reduction setting include endometrial cancer, uterine sarcoma, stroke, and pulmonary embolism.  ALERT Discuss the potential benefits versus the potential risks with women considering treatment to reduce their risk of developing breast cancer. Benefits of therapy outweigh risks in women diagnosed with breast cancer.
ALERT Discuss the potential benefits versus the potential risks with women considering treatment to reduce their risk of developing breast cancer. Benefits of therapy outweigh risks in women diagnosed with breast cancer.
• Clotting factor abnormalities may occur with prolonged tamoxifen therapy at usual doses.
• Variations on karyopyknotic index in vaginal smears and various degrees of estrogen effect on Papanicolaou smears have been seen in some postmenopausal patients. May increase serum thyroxine concentrations and may be explained by increases in thyroxine-binding globulin.
• Initial adverse reactions (increased bone pain) may be a sign of good tumor response shortly after starting tamoxifen therapy.
• Monitor WBC count, platelet count, and periodic liver function tests results.
• Monitor serum calcium levels; hypercalcemia may occur early in therapy in patients with bone metastases."0 -
I have nafl regardless of tamoxifen. My pcp does labs twice a year. I'm very overweight. Losing lbs would help.
0 -
Artista, I'm sorry to hear about your FLD. Wish you the best with its management. I only posted because Aseyes was specifically asking since her liver labs were newly elevated since starting Tamoxifen.
0 -
I am NOT saying the chance of fatty liver disease isn't real, but can someone verify my math on this: Quoting from a post above "a relatively low concentration of TAM (6 mg/kg/day) "
a kg is approx 2.2 pounds so a 100 # person is 45 kg. 6 mg / kg would be 6x45 or 270 mg so over 10 times what most of us are taking - right??
0 -
Dorothy - your math is right I believe.
I think it may be important though that that amount you are referring to is from an article which is only about Tamoxifen mechanisms in general, not in reference to Breast Cancer. Also, the medicine is given via injection to mice to study the effects. "Group II were labeled as the TAM group, administrated with i.p. injection of 6 mg/kg/day TAM for 2 weeks."...."At the animal level, 6 mg/kg/day TAM was selected for 2-week treatment to build a short-term animal model, while the normal clinical dose for patients is 0.33 mg/kg/day (20 mg/day) and the scientific research dose for mice is 25 mg/kg/day (26,27)."
I'm sure if we were all given these mega doses we would sustain liver damage (thankfully we aren't!) which is what I think the point is, showing it's a "safer" range. So because we AREN'T given this dose, we still need to know there is the RISK.
Like all medicines they come with risk, but IMO we all should be informed about what could happen. I wish more teams would discuss this with their patients. I know it wasn't discussed with me. And given my other medical dxs it should've. The one study I feel is most important is the one that states those on Tamoxifen, especially those in the age range of 26-35, do run a 30-40% of developing NAFLD at some point in their therapy regimen. Given those type of statistics, it should be discussed every time it's prescribed.

""Several studies showed that taking tamoxifen may incur a 30–40% risk of developing nonalcoholic fatty liver disease(NAFLD), according to different diagnosis instruments."
Conclusion: The current study suggests that tamoxifen treatment is associated with the risk of fatty liver either by increasing the risk of newly developed fatty liver conditions or worsening previous fatty liver conditions, and even retarding fatty liver improvement."
0 -
DorothyB Should I ask about blood tests? I'm not having those, sounds like others are??
0 -
My primary doctor does a liver function test every 6 months for now. I just received my results and my levels have returned to normal. My ALT was elevated on my last test. I do have NAFLD and was told to decrease my carb intake and lose 20lbs. I had gained weight after a knee injury and was on a lot of Tylenol and ibuprofen. I was told that can also increase your ALT level. I have been trying to lose weight, exercise, and only take Tylenol/ibuprofen if I really have to. I also started fish oil 6 months ago. They said Omega 3 supplements, Salmon and Tuna would help decrease the level. I try to have nuts as a snack and put Chia seeds in my smoothie. So far so good. My MO wouldn't order the labs so I am glad my Primary is following up on this. Definitely ask for the liver function test, CBC, and a CMP.
0 -
haven been taking tamoxifen for 4 years. my liver blood work has been up and down. Just got my results today and they are higher than ever. I had my surgery 4 years ago diagnosed with dcis stage 0 breast cancer. Did radiation. Is anybody else having the same problems. i have joint pain all over. please help
0 -
did you stop taking tamoxifen? i eat a lot of those foods listed.
0 -
HI fernanda08, No I am still on Tamoxifen, but as Dorothy did I decreased my dose to 10mg daily. I haven't seen my MO yet to discuss this. I think there was another post from someone who had your diagnosis that went down to 5mg. because of the side effects and her MO was in agreement. Have you asked to see how your MO feels about it? Are you on Tamoxifen for longer than 5 years?
0 -
I am now in my 4th month of taking Tamoxifen, over the last few weeks I have been experiencing odd symptoms which at first I thought was viral as I had been unwell also, but I've realised that although I am now 'well' again having recovered from the viral illness, I am still getting these strange symptoms that come and go every day.
It feels like I am totally zonked/drugged out, my head feels so heavy and fuzzy, I can barely even respond to my family when I'm feeling like this, feeling completely exhausted, plus a big increase in the severity and number of hot flushes. Last night I even toyed with the idea of stopping Tamoxifen for a month, so I can see if these symptoms disappear.
Does anyone think there is any benefit in stopping for a while, to confirm if it is the Tamoxifen?
Feeling confused and a bit desperate at the moment as it is making life so difficult. 0
0 -
Pooh- what time do you take it? I definitely felt that dizzy/ drugged feeling at the beginning, but I used to take it right before bed, so it didn’t effect me much. After a while, i don’t remember how many months, that feeling went away. Now I take it with dinner, no issues with brain fog anymore. After two years, I don’t know if the hot flashes are less or I’ve just gotten used to them. They’re definitely still there, but they don’t make me as miserable.
0 -
Pooh - I had the same sort of "brain fog". I was taking them at night, but still having a tough time doing anything that didn't "have" to be done.
0 -
Thanks Cpeachymom and DorothyB, I take 10 in the morning and 10 at night, I thought at one stage I was feeling better this way than taking 20 all at once at night, but not sure about anything.
I am also not sure if stopping them for a while will scientifically prove that it is the Tamox that is doing it even if the symptoms go away, but I sure am tempted to give myself a Christmas present of a drug free Christmas and New Year!0 -
Twice I didn't take my tamoxifen at night (taking once a day) and both times I felt a huge difference the next morning. (Once was on purpose when I was going down from 12.5 mg to 10 mg and the other time was an accident.) I tried once taking just 5 mg at night because I wanted to be super-productive the next day, but couldn't tell a difference.
You could take a break for a few days and then start again and see if the symptoms go away, then come back.
0 -
I have been on the Tamoxifen for just 2 months. I don't have the severe type brain fog but do notice some difference from pre-BC. The hot flashes are definitely stronger and last longer than before, but not necessarily more of them. I see my MO for first visit since starting in January, and hope to get the blood tested. I think he did mention that at the beginning. I was already peri-menopausal at time of dx, so I am telling myself that I would probably have been having hot flashes now anyway even without the med. I am now (last few weeks) been noting some tingling, mostly in my fingers but occasionally toes also.
0 -
three months of 20 mg at night I am depressed I realize that Maybe from tamoxifen And I mean depressed emotionally and physically - no energy or enthusiasm Familiar
0 -
Together - YES! taking effexor helps w/ the depression, but still had the lack of enthusiam
0 -
Hello.
I am interested in women who were already postmenopausal and who chose to stop AIs due to side effects. I had a HORRIBLE 13 months - 7.5 on Letrozole and 4.5 on Exemestane (1 month nothing in-between). MO has recommended Tamoxifen but I am wary. VERY wary. I also have fibromyalgia. I have been off AIs for 3 months (still on Duloxetine) and still have pain issues and what appears to be longterm damage in hands, especially thumb.
I am 56, will be 57 in April. I retired from teaching (34 years teaching) last May - teaching and dealing with AIs was horrific. I am still tired all the time. I practice yoga - have for years; but sometimes the depression and pain and anxiety are too much.
Any of you in a similar situation? What have you chosen? How is it? Side effects? Thanks.
Peace.
0 -
Hi all,
I'm on my second go-round with breast cancer. I had it in 2016, had a lumpectomy and radiation for 6 weeks. It came back in Oct 2019 and I had a double mastectomy with reconstruction. One of the implants failed (on the side where I had radiation before) and I was septic, so that was removed a couple of weeks ago. I started taking Tamoxifen yesterday.
I seem to be extra super sensitive to most medications. When I last had breast cancer, I was put on anastrozole, which gave me a hideous, disfiguring rash - I still have scars from it - plus it made me so exhausted I could barely function and I had constant night sweats. I am really worried about having a similar reaction to tamoxifen. I'm wondering if anyone knows of any studies that may show the benefits of taking tamoxifen if you've had a double mastectomy. Is it beneficial anyway? Or have they even done studies like that?
0 -
Post-menopausal here, and my MO recommended tamoxifen b/c I'd fractured my pelvis running. I tried for three weeks but experienced extreme heart rate spikes on my runs. I'm talking 176--189 within 30 seconds of starting my run.
That is not normal for me. I've run for years and have the heart rate data to prove it.
So I've stopped taking it and doubt I go back on it again. QOL > a tiny chance of recurrence (with all due respect to those who choose otherwise or who do have a recurrence like AmeliaPond just posted. Really sorry this has happened to you.).
0 -
Myyoga4me - I am post-menopausal. I am taking tamoxifen due to osteoarthritis. After being on 12.5 mg for 7 weeks (building up from 10 mg to 20 mg), I was a zombie. My other side effects (leg cramps, hot flashes, etc) were manageable. I decided to not try to take 20 mg. Instead I dropped down to 10 mg. I can still tell a difference, but it is tolerable.
0 -
Hi Ameliapond,
Mastectomy reduces the risk of local recurrence. It does but eliminate the risk of local recurrence and it has no impact at all on the risk of distant recurrence (metastasis).
Hormonal therapies help with both (for women with HR+ cancer).
I couldn’t tolerate tamoxifen but my doctor was willing for me to try toremifene instead, and so far (early days still) it’s going much better than tamoxifen did. Every woman will have her own experience, and it might be the reverse for you. But it might be helpful to know there are options in case tamoxifen doesn’t agree with you. If you are post menopause (I am not), there is even more evidence that alternative SERMs (toremifene, raloxifene, and I think a third) can be equivalent to tamoxifen for risk reduction.
That said, since you had recurrence on AI, you might ask your doctor about testing your tumor for esr1 mutations, which can make it resistant to most forms of hormonal therapy.0 -
Thanks, Salamandra. Is that the testing they initially do when they remove the breast? I know I was HER2 negative and Progesterone/Estrogen positive. I'll have to go back through my records to see if that test was done.
0 -
I don’t know whether they do it routinely on recurrence tumors. I actually came across the info by accident searching for more data about SERMs other than tamoxifen, and it came up in the context of treatment resistance stage 4 cancer. It may not even be relevant to you, I may have made an unwarranted leap. Still, I think it might be worth asking an oncologist about.
Here’s some links from what I found:
https://www.tandfonline.com/doi/abs/10.1080/14737159.2019.1631799
0 -
Thank you! I'll read those tomorrow and see if they're relevant and talk to my oncologist if so. I had stage 1. It was caught very early. I'm just worried because this is my second dx in 3 years. Plus, I'm just a worrier and over-thinker in general. Not helpful in this situation. I spend way too much time looking for information and winding myself into a tizzy.
0 -
I am in just my 3rd month of Tamoxifen so far. I am now 55 and was perimenopausal at time of BC diagnosis. I was told that in order to be considered menopausal and a candidate for AI's, I would have had to be without a period for 12 months prior to starting chemo, which was not the case. I have not had any period since starting chemo, so 9 months now. I understood that after I am on the tamoxifen for a year (assuming no periods occur), I may be transitioned to an AI. I agree that the hormone blocking meds would decrease both local and distant recurrence so are likely beneficial even after double mastectomy. I have not had too bad side effects so far. Hot flashes (but generally tolerable and I figure I would be having anyway with "normal" menopause. Some mild headaches. Some fatigue but it is not a big deal so far.
0 -
Hello ladies. I was diagnosed with early stage one and had a lumpectomy and radiation therapy. I had my five year all clear mammogram and was released by my surgeon in October. I am just finishing up five years on tamoxifen. I have had varying degrees of fatigue and hot flashes on and off during the course of my treatment, but in the past month both have become increasingly worse, I am to the point of barely being able to get out of bed. I was just wondering if anyone else has had such an increase in side effects right at the end of treatment. Luckily my appointment with my oncologist is in a week and a half. Praying she will take me off tamoxifen as planned. What can I expect to happen with these side effects once I stop taking my prescription?
0 -
Welcome, Pcox1609, and congrats on your 5 years! We hope your appointment with your oncologist goes the way you're hoping, and you're able to start the new year off without the side effects you've described. Please keep us posted!
The Mods
0