Lobular Sucks!
Comments
-
Yes, I attended the First International ILC Symposium in Pittsburgh 2016. It was awesome. Definitely movers and shakers there, and lots of smart patient advocates too. That is where the Lobular Breast Cancer Alliance was born. Today's virtual sessions are finished, but the second half is tomorrow. Then a patient advocate meeting on June 30.
One of the speakers noted today during the Q&A at the end that only TNBC and Pleomorphic ILC are getting good responses from immunotherapy. : ( They mentioned GELATO with atezo + carbo and also Eribulin + immunotherapy.
0 -
Thanks for the post about the virtual symposium, ShetlandPony. I missed the live session due to work, but I listened to the recording. I’m glad there is no fee to attend. These virtual meetings are great for those of us who can’t travel.
It is reassuring to me that these researchers are working on “our” type of cancer. Seeing the signet ring subtype mentioned on a slide with other ILC subtypes, gives me hope.
I’m on Tamoxifen. Hearing the discussion about Tamoxifen versus AIs was interesting. I’ll be asking my MO again whether he still thinks Tamoxifen is the best choice for me. My hair is falling out and my scalp is sore around the crown area. I know AIs also cause hair loss, but maybe I’ll do better on an AI
0 -
Cyathea, they have all this data that points to aromatase inhibitors being a better choice for ILC, but they won't actually say it because they don't want to speak against the official NCCN guidelines, and the guidelines require really definitive proof. When I attended the first symposium in Pittsburgh I noticed that the European oncologists were saying they did not like tamoxifen for their ILC patients, and the oncologists working in the USA were saying, "You don't have proof." Well, someone could die waiting for them. Aromatase inhibitor are an approved treatment, and so is ovarian suppression. I have strong feelings about this, since I recurred after just three years on tamoxifen with stage 1 and an Oncotype score of 16. I wish I had done OS. I know that nobody should base their decisions on one other person's experience. But look at BIG 1-98. Another point is that PR negative may be a marker for tamoxifen resistance.
0 -
SP: thank you for mentioning PR- is resistant to tamoxifen. I have attended this symposium with lots of distractions from home and haven't followed as much as I prefer. I am PR- and from Dana-Farber, I was recommended tamoxifen that I didn't take it. Thank you for mentioning it!
I do have a question about ILC and OS: how come this BC is called old ladies cancer since it is common to women in their 70s? Aren't women at this age in menopause? Aren't our bodies at this age producing min amount of estrogen? How come women of this age get ILC when they are in their low-level estrogen stage of life?
0 -
Hi, I see no one has posted anything for over a year on this thread during Covid. Shetland Pony has directed me to this thread after receiving her wonderful compiled list of BCO threads with ILC information- and accessing the ILC Alliance website that is giving me information I should know. I'm repeating a post I recently put on the Xeloda thread here (my current medication). My CA15-3 is rising dramatically while being NED on a PET and I started worrying about why and ILC seems to be the answer. CA15-3 did not originally identify my intestinal mets, so I'm confused about why it is going crazy now (up to 768).
I didn't realize how different ILC is from IDC, only 10-15% of BC are diagnosed as such. I'm trying to track down old findings, I believe my BC (1998) was originally a mix of IDC and ILC but a recent biopsy on my rectal wall only mentioned ILC. It was very clear to me that my "unheard of" cancer to the outside of my small intestine was very predictable for ILC- a string net of cancer cells that will wrap around and squeeze, not seen on CT. I feel more enlightened than all the docs I went to when trying to diagnose my "digestive" problem for a year, including MO and GI specialist. I'm glad it's a slow growing cancer but it is hard to detect when it is there. I Hope everyone is doing as well as can be expected and finding hope in the right places. Right now this feels like my "people". NIna
0 -
OOPS! I didn't get past the first page when I wrote my post. I now will read all the subsequent posts. I'm finding myself lost in Lobularland today.
0 -
Thank you for directing me to the ILC Symposium. Just finished watching, at least first and last day- I'm so glad they are now focusing on ILC. I went back to my initial pathology report in 2002 and found ILC in my first liver biopsy. I've never thought it was different than IDC, and my MO"s never had anything to say about it being different . I liked their term LobMob to describe themselves. I was confused by some terminology- when they were talking about -No her2 amplification or over expression on the Neratanb trial, the tumor did have Tumor mutations on the surface that worked with their drug. I'm thinking even though I'm Her2 negative, my IHC comes back +2 equivocal, is that the same as tumor mutation?
Tamoxifen? I metastasized after 3 years on it, markers went down as soon as I started on letrozole. It appeared to be fueling the cancer. Recently someone suggested I take Tamoxifen but I'm not going to even consider it.
I'm going to look into the FES PET since my PET is clear but my markers high. Maybe it will show something diagnostically. ALSO does anyone have a different tumor marker they can recommend since my tumor has gone to unusual places (outside of small intestine, rectal wall)? I only get CA15-3. THANKS
0 -
NinaCA, I just had an FES PET in June. It was a trial that I was in. It is the only thing that showed the mets in my stomach and the two micro metastasis under my right armpit that I didn't know about. They say it's not good to see the liver or small bowel, as they take up a lot of the tracer. I was disappointed to know that since it showed everything I already know about. I was hoping it would show my peritoneum and if there was anything going on there. It was awesome to finally see it in my stomach, though. Not one other test shows it there except endoscopy. It also showed all the metastasis from my skull to my femurs that I already knew about as well.
I have the 15-3, 27-29, and CEA tumor markers monthly.
0 -
Nina, just checking -- did you see my last two PMs to you? I'll repeat some of it here on this thread.
About Her2, here is what I know about the categories. (Please double-check with your doctor as I am just a reading cancer patient, not a professional!)
https://ascopubs.org/doi/10.1200/JCO.19.02488
Her2 positive, aka amplified: On IHC 3+. This automatically gets a person herceptin and/or other Her2 therapies.
Her2 negative: 0 on IHC. Or TRADITIONAL CATEGORIES: 1+ on IHC and negative on ISH. Or IHC 2+ and negative on ISH. No herceptin given.
Her2 low A NEW CATEGORY: IHC 1+ or 2+ and negative ISH. They are starting to use Her2 therapies for this type.
HER2 mutated aka ERBB2 mutated: This is not the same as Her2 amplified or Her2 low. Rather there is a mutation in the Her2/ERBB2 genes of the tumor. This is not found by IHC or FISH. One needs genomic testing of the tumor (or CTCs in the blood) such as Foundation One or Guardant. This qualifies one for the Her2 therapies such as neratinib, whether in a trial or out. Note that herceptin alone seems not to work well for Her2 mutated, while neratinib can work well.
So in your case, Nina, with Her2 2+ equivocal on IHC, I would expect FISH to be ordered. If FISH comes back positive, you would qualify as Her2 positive/amplified. If FISH is negative you probably qualify as Her2 low, traditionally called Her2 negative. In that case, discuss the new Her2 low treatments/trials. But you will need a genomic test of a biopsy to see if there is a Her2/ERBB2 mutation to see if neratinib is a possibility.
0 -
Yes, I do have a different tumor marker to recommend: CA 19.9. I have used the breast cancer marker CA 27.29 for years as it tracks well with what the cancer is doing. When jaundice etc. led to ultrasound and ERCP that demonstrated my bile duct stricture, my oncologist and the liver/biliary specialist wanted CA 19.9 added. This is a gastrointestinal marker, and even though we are dealing with ILC breast cancer not GI cancer, because of the location of the bc in or near the bile duct, we watch CA 19.9. It does track well. With my current treatment working, we saw this marker fall and I stopped needing bile duct stents. So even though imaging did not show the ILC in or near the bile duct, the symptoms decreased as the marker decreased, and the treatment worked in both liver and bile duct area. This is why I asked you about this marker earlier or in another thread, KBL. If they cannot see the cancer, maybe watching CA 19.9 will help you track whether it is progressing or receding in the GI tract.
0 -
I will ask my onc to test it, but I have a feeling she won't be thrilled. I asked for the 125 to be tested. She did it, and it came back at 1400. She dismissed it and said it's because of the breast cancer. My 19-9 in 2016 was higher as well. When I had an abdominal MRI a few months back, they said I had sludge in my gallbladder. I'm not sure what to make of that.
0 -
Thanks Shetland. I have read your 2 PM's and am grateful for all your advice and suggestions. My FISH have always come back negative, there are "no reportable genomic alterations: ERBB2 (copy number 2.0)." So I guess I am the NEW Her2 Low category. I have an email in to MO and I plan on having discussions with him armed with all the new information I am still trying understand. Glad you found the Neratanib trial. NINA
0 -
KBL, who cares if your onc is not thrilled? In order to see if 19.9 or any tumor marker will be helpful, they need to check it regularly, like every month, to see if it tracks with anything a scan or scope does show, and with your symptoms. She can't just check it one time and say Yup, that's because you have cancer. You need to be able to look for patterns and trends. Is it rising, falling, steady? Why should your onc be so stingy? You have a cancer that is very difficult to track and she should be open to trying and using anything that could help. The risk to not doing this is that the cancer gets away from you when it doesn't have to. Maybe she does not want to fight insurance for you? Tough. Part of caring for you is working to get you what you need, and your case is not typical. Have I misunderstood something here?
0 -
I edited my post above about Her2/ERBB2 mutations to clarify that neratinib can be accessed both in and out of a clinical trial (USA). (I like my trial a because it gets me a neratinib along with two other drugs, that may give longer PFS than single-agent neratinib. Another BCO member gets neratinib and xeloda, not in a trial.)
Nina, there is a lot of discussion here on BCO about Her2 low treatment. Interested to hear what your onc says.
0 -
Thank you, Shetland. I tell her all the time what I want. She knows I'm very direct. I may tell her to go ahead and add the 19-9 and 125 again. I don't think insurance has a problem paying, and I'm at 100%, so I certainly won't be paying for it. She does do what I ask. I guess I'm trying to give her a break because I can be pretty forceful sometimes. Lol.
0 -
I'm thrilled that this thread is still active after a year of not logging in! Lobular gals have so much ambiguity to deal with their disease. Lobular really does suck!
I've been having FDG (glucose) avid PET/CT scans every 6 months since diagnosis in 2018. They have always been negative. FES (estrogen) avid PETs have recently been approved by the FDA.My first FES avid PET/CT was last week. It showed:
1. No evidence of estrogen receptor positive abnormality.
2. Stable numerous scattered sclerotic osseous metastasis with no radiotracer uptake.(I'm bone only mets) but….I read that FES is not great at reading visceral involvement.
By this report it seems that I'm stable. I'm meeting with my oncologist tomorrow, so she will confirm.
I will tell you…I've never been symptomatic. My CA 15-3 levels have been only slightly elevated. The side effects of Ibrance/letrozole/xgeva have not been terrible, but definitely have had an impact on my QOL. I truly wish I've never known about my disease. It's a total mind f***. I wish I could just stick my head in the sand and continue on with my life.as if nothing ever happened. Anyone else feel this way?
0 -
Leigh68, I was in a clinical trial for FES PET in June. Unfortunately, I lit up like a Christmas tree in my bone mets because I’m covered from skull to femurs. It’s also the only thing besides an endoscopy that shows the mets in my stomach. I agree, it doesn’t do well with other organs. The radiologist said they take up too much tracer to be of help. After probably five FDG PET scans throughout, I finally figured out FDG doesn’t work on my cancer. The only thing that shows the bone and bone marrow involvement I have are MRIs and now the FES
I’m one where my cancer was missed for six years until I had the symptoms when it spread to my stomach. Please don’t regret knowing. If I had known when it was in my bones only, I probably would be able to live many more years than I’m going to get to.
Congratulations on a good scan. I enjoy every day and really try to stay in the now. If I think too much in the future, I get sad knowing I’m probably not going to be here.
0 -
Thank you for participating in the trial and helping to get FES available for the rest of us. I’m sorry that the cancer was missed for so long. If you had no primary and were asymptomatic, why would you think there was a problem?
Staying in the now is a good mindset for everyone regardless of health status. Covid, fires, collapsing apartment buildings…really all anyone has is today.
Gentle hugs, leigh
0 -
Leigh and KBL- When you wrote the you hear FES was not good for visceral involvement, are you talking about the abdomen (liver, intestines) because that's where mine have gone? What are the places FES works best on? KBL- what were your symptom when it went to the stomach? I'm wondering where mine will show up next and how do I identify it. Trying to stay in the NOW so I can enjoy today and not worry too much about tomorrow.
0 -
Leigh, I had a car accident in 2013. After an MRI, the radiologist sounded the alarm saying he saw something in my bones and bone marrow. They did testing for multiple myeloma. Of course, it all came back negative. I had back pain. Over the years and more MRIs, it was progressing, but they never went a different route to check for a different cancer. In 2018, I lost 17 pounds in a few months and couldn’t eat. After endoscopy, they found the spread to my stomach. I did have symptoms at that point. That’s when they realized it was breast cancer, not MM.
Nina, here is exactly what the radiologist said when I asked him if he could look to see if it spread to my omentum. “In regards to your earlier question about FES imaging and bowel/mesentery involvement--the bowel and mesentery/omentum around the bowel normally show a lot of FES uptake so that makes FES limited to detect potential disease in that area. The areas where FES is particularly limited to detect malignancy are the liver, biliary tree and small bowel.”
The stomach symptoms were taking a few bites of food and being really full and nausea after eating. I’m actually having the same symptoms again and have lost a few pounds. I’m not panicking but will have to try to figure out how to stop it. One of the only things I can watch are my tumor markers. One has gone up four months in a row but in very little increments. I have never thrown up from the nausea.
0 -
0
-
KBL- Are you having CT scans? I had a similar issue with throwing up and I had lost 35 pounds by the time I had surgery. The final straw was when I threw up through my nose!! So Gi had me take a 4 hour test to show how my food was not going through my stomach to my small intestine fast enough (every hour they took an x-ray of my radiated scrambled eggs and toast). Finally a CT scan showed thickening of the wall of the small intestine so they went in and did an exploratory laparotomy and found the culprit, ILC tumor around the small intestine which they took out. I was finally able to eat again. My markers had not gone up very much, not helpful for this event (has been helpful for others). Are you getting PET/CT or CT scans with contrast only? After this incident I was switched to PET/CT (with no contrast). Endoscopy never found anything, maybe I should consider it again now they know what to look for. I attribute my stomach/diarrhea upset to my current medication, Xeloda.
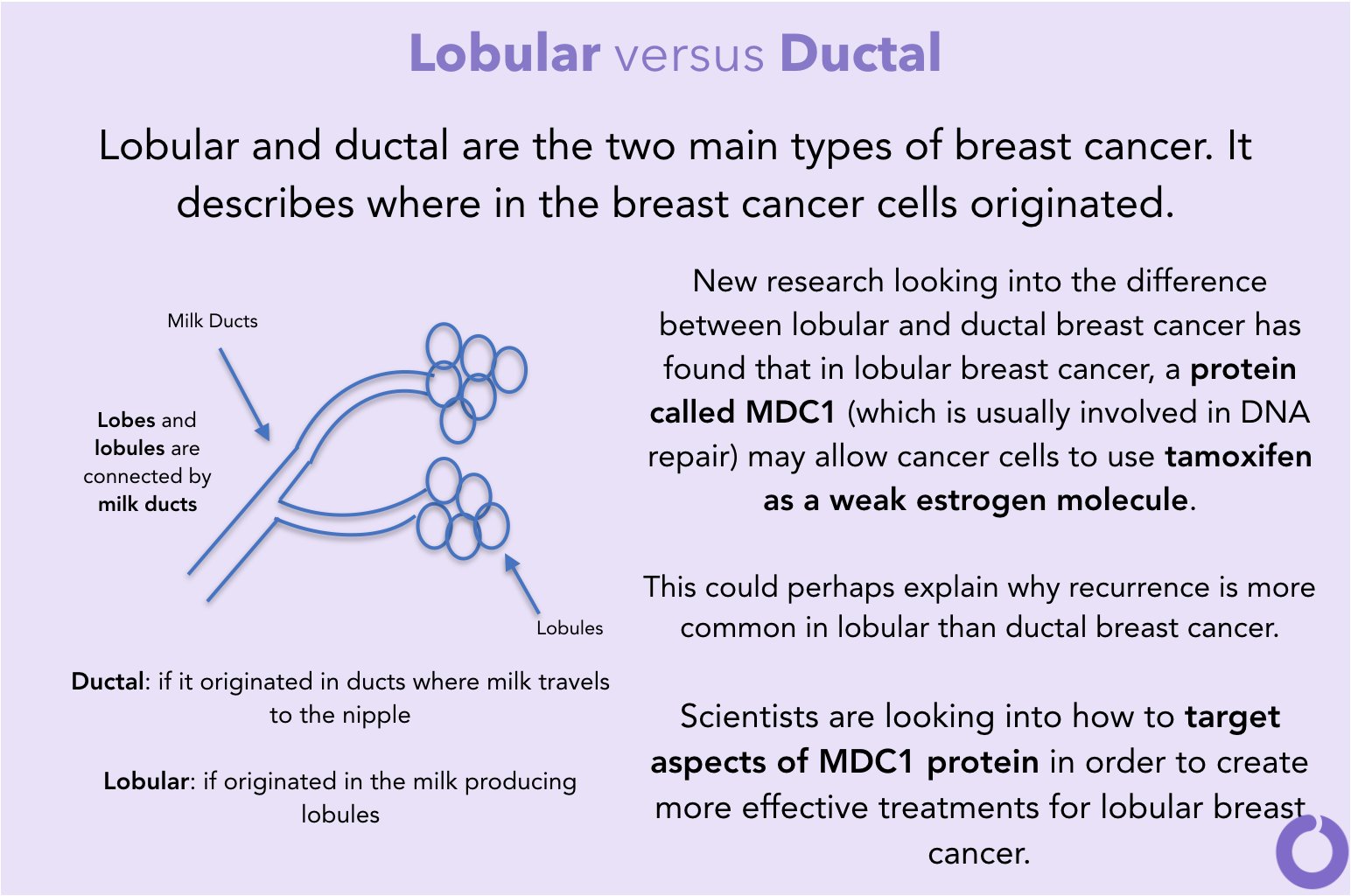
Lilly- thanks for the graphics although I don't quite understand about the MDC1 protein and how it interacts with Tamoxifen. I became resistant to Tamoxifen after 3 years and luckily switched to an Aromatase Inhibitor instead, femara. Are they saying that Tamoxifen can work well with MDC1 or causes resistance (a weak estrogen molecule?)
0 -
Nina, wow, that's fascinating. I'm going to see what doc says. I'm going to save what you wrote to talk to her. I do have CTs and have had PET scans. The cancer doesn't show up in any of them. I actually will probably have a CT soon because I had some other tests and haven't had a CT for a while. I've never heard of what you had done. I have a gastro. I may have to go back to him and ask if we can do any other tests to see if there is another cause. I have been on the same meds the whole time, so I don't think that's it. Thank you for sharing. I'm glad they figured out what it was. This stuff is crazy
0 -
I don't know if I'm reading it correct but my understanding is that MDC1 protein is using tamoxifen as week estrogen. Probably, that's why tamoxifen doesn't allways work in lobular cases.
1 -
Ladies, do you know if a CT scan finds ILC in the abdomen? I had a CT scan last week that didn't find anything suspicious but I continue to lose weight unintentionally and feel some slight pain where the liver is located. Also, I feel full since I wake up in the morning and I haven't eaten overnight. Any suggestions? Thx so much!
0 -
LillyisHere, CTs have not seen my cancer that I have in my stomach, nor has any PET scan seen the cancer I have in all bones and bone marrow and stomach. I had a CT just the other day that says I have gastric wall thickening. That may mean mine is progressing. The only thing that found it to start with was an endoscopy. I had symptoms in October of 2018 with not being able to eat and nausea, losing 17 pounds. Treatment made it better, but I'm two years and two months on Ibrance, and the symptoms are back. I've lost five pounds in a month and a half.The cancer is in three places in my stomach. If you haven't had an endoscopy, I would ask for one. Please let the gastro know that your stomach may look normal. When I got done with the endoscopy, the doc said I had some gastritis, and otherwise my stomach looked normal, but, thankfully, he took five samples and was totally shocked that I had breast cancer in my stomach. Feel free to ask me anything.
It also could be something else like gastritis, but it's best to check and make sure.I do not have pain with it, just weight loss, not being able to eat much, and nausea. I've never thrown up from it.
I also had an MRI of my abdomen, and it didn't mention my stomach at all.
0 -
Hi- Tumor Markers now over 1000 and continue to get higher every three weeks-no physical symptoms.

I talked to the office where FES PET clinical trials are being done in southern California and they are ready for me with 2 days notice to give me one, after I talk with the Doc. tomorrow. I will schedule a regular PET here in two weeks and then go down south the next week for a follow up FES PET. Two months ago NEAD on my PET- only laugh was they again thought I had a hysterectomy (2nd time they wrote that). Doesn't give me much confidence in their scan reading ability. Just cut and paste from a previous wrong report that was corrected. Good to know KBL that they were able to find ILC in your stomach with the FES. I guess if they find something they will immediately take me off of Xeloda and put me on Taxol (had it 22 years ago but can have it again). I feel like stopping Xeloda right now and changing meds even if they don't know why.
Lillyishere- I lost 35 pounds along with nausea and some vomiting in Dec. 2019 because I had an ILC tumor around the outside of my ilium which was squeezing the intestine so food wouldn't go through. They noticed thickening of the walls on a CT and did an exploratory laparotomy and took out a small piece of intestine with the tumor. Everyone said there was no way of knowing it was there (I only had CT scans at that point, no PET scans so I don't know if they would have found something). It took a year of gradual discomfort before it was finally bad enough to explore with surgery.
0 -
NinaCA, I had already known. I had stomach mets from endoscopy, and was hopeful doing the FES would show if it was elsewhere. Then I learned it's not good for finding other mets in the liver or small bowel because it takes up too much tracer. Still not good for me.
I can totally relate on taking wrong information off prior reports. Ended up in the emergency room in April. They said I had bilateral hydronephrosis. I was like WHAT? Had a kidney scan where they see how fast your kidneys empty. All good. Then the radiologist told me it was because when my bladder was full, it distorted my kidneys. No kidney problems. Had that CT just this past week. Different radiologist compared it to emergency room CT. Lo and behold, in the report, mild hydronephrosis. I completely thought what the ever living bleep, that's a cover-your-ass moment if I ever saw one. I will be talking to my doc about that. That's just not right. I'm sorry that happened to you too. This is so frustrating.
I'm so sorry for what you've been through too.
0 -
Thank you KBL and Nina. I have an appt with my PCP at beginning of October and I will discuss it with her. I am giving a month on any weird pains and symptoms in case they go away. The only comment I got from CT report is that it showed that I am constipated while I am not at all! I told my DH I am literally full of sh***
 0
0 -
Mine say I’m constipated every single time when I’m not. What is that? It drives me crazy. One even said obstipated. I had to look that one up. So frustrating.
0