Diagnosis Usual Ductal Hyperplasia---surgery?
My diagnosis was Usual Ductal Hyperplasia (UDH). It's been in my breast for seven years, although I never received any indication of it in the letters from Radiology about my mammograms, and my primary care physician never discussed it with me. What a blow. I'm still gathering data because some of the research papers on line conclude that UDH can be or is a precoursor to malignant breast cancer. Was not told what type of cells were in the biopsy, epithelial, neoplastic, non-neoplastic. The biopsy was ruled Nonmalignant. Surgeon does not think removal is appropriate. Mass can't be felt but is apparent on mammogram and ultrasound. My feeling is that it is a foreign growth and I'd like it removed. Has anyone had this type of non-malignant mass removed? I asked for a second opinion from a breast care center of a major healthcare institution in my state and requested that my local hospital deliver all mammograms, slides, smears, and other data to the major breast center. What I got was a "limited" second opinion because the major hospital felt they didn't get all the information and didn't communicate with my local hospital or me re any lack of information. What good is a limited second opinion? QUESTION: Has anyone had UDH and had the mass removed or had the mass change from nonmalignant to malignant?
Comments
-
Mary - Glad you posted here. That other thread had been inactive since May 2019.
You didn't state your age. I expect that would make a difference. Or if you have any family history of breast cancer?
If you are seeing a breast specialist, you have to decide if you trust that doc - and then go with watchful waiting. If not, I would make an appointment and go personally meet another doc. 'Limited' sounds like you were unable to have any personal contact and for me that's important to decide who I trust. You can take copies of all the reports with you & get CD copies of the mammograms.
0 -
Hi, Mary, Happy New Year!

It's not that I knew before my excisional biopsy that my lesion was just UDH (among other also benign findings), actually it was a BIRADS-4 1 cm solid mass, I found out so as soon as I received the histology report. In my case my breast surgeon based on the imaging results decided that it would be safer to perform straight away an excisional biopsy (same procedure as lumpectomy but the latter term is used when cancer cells are present) rather than a sono-assisted biopsy. So, yep I did have an excisional biopsy for UDH (which was great histology news to receive!) but I didn't know beforehand the nature of my lesion, in my case malignancy was not at all excluded according to mammo, sonogram and MRI and the mass was also spiculated (synonym of cancer) and located very close -almost attached- to my chest wall muscle, they couldn't risk not removing it completely. Wishes to get your substantiated second opinion soon. Hugs, Jo
 0
0 -
Thank you for your reply. I am a very active 78 year old, walking at least 12 miles a week, lifting weights, babysitting with a toddler. I have longevity in my family, with aunts living years beyond 100 and one currently at age 108 and still fairly active. Two aunts on my mothers side had breast cancer, and one on my father's side as well. There is other cancer in my immediate family; my twin died of a brain tumor and one brother has slow growing prostate cancer, which one doctor told me is from the same type of cell family as breast cancer. The limited second opinion came from the Radiology Dept of a reputable health system, with their reasoning being that they did not have access to certain info from my local health system. I'm amazed that the Radiology Dept did not make contact with my local hospital for that information. I've written letters to both hospitals and am awaiting replies. I did meet with an oncology surgeon from the other health system who said he didn't believe the articles from the American Cancet Research Institute and other institutions that published research papers (though UDH research seems to be limited) and concluded that UDH was/could be a precursor to malignant breast cancer. At this point, they want to watch it with annual memmograms. I had an ultrasound and a needle biopsy which tested as UHD, but, as I understand it, other parts of the mass could contain other types of cells. My mass measures 1.3 cm, and I've raised the question about its shape. I was shown the mass briefly on the screen, and it did not have smooth edges or shape. I feel like I'm fighting a battle to get information. The mass was rated a BiRad 2.
0 -
You'd need genetic testing to know if your family history is actually relevant. My mom had breast cancer, and a paternal aunt died from it. My dad had kidney cancer, and so did I. My maternal grandmother had uterine cancer, and so did I (endometrial, but it had infiltrated a bit). I had genetic testing done and there was no connection found to any of them. For breast cancer alone, I've seen in other threads here that the genetic connection is surprisingly low even when there's a family history. I think having family members with it is more relevant to getting mammograms and other testing earlier and more often than the general population.
0 -
I’ll chime in and say that genetic mutations, as we currently know them, are responsible for the minority of breast cancers. I have an illustrious (not!) family history and belong to a minority group that has a much higher incidence of BRCA genes. I have had extensive genetic testing and… nothing! So as Alice said, you need genetic testing to confirm a familial connection and odds are that there may not be one. Birads 2 is good! Take care
0 -
I also asked the surgeon about testing for estrogen receptors. I have been on birth control and HRT for about 35 years (reasons: complete hysterectomy at 38, very small boned and osteopenia). He said no reason to do this. There are at least two research papers online that state that HRT is a contributor in UDH moving to malignant cancer. Which do you believe?
0 -
Usual ductal hyperplasia is a fairly common benign condition. It is usually not treated and while it does increase risk, the amount of risk increase generally keeps most women within the normal risk range. For this reason, UDH usually doesn't warrant mention from radiologists and other doctors when it's found on a pathology report.
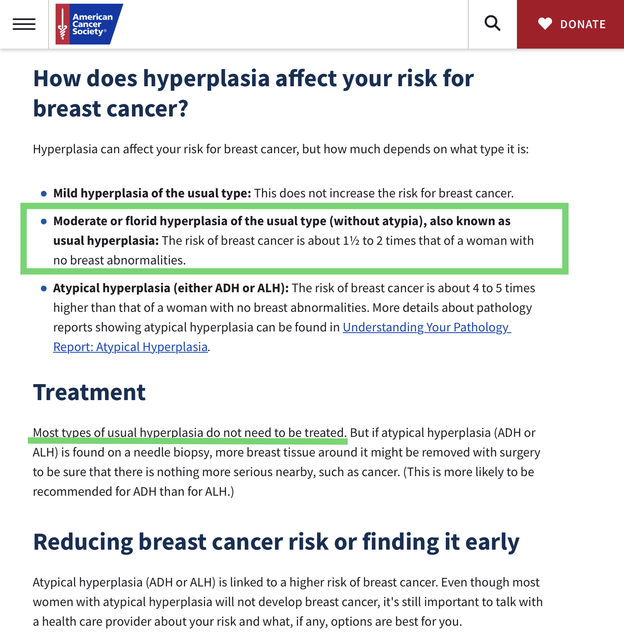
The very important line in the copy that I've posted above from the ACS is that usual ductal hyperplasia increases risk about 1 1/2 to 2 times above that of a woman with no breast abnormalities. All women start off with a base risk for breast cancer, just because we are women. This risk is about 4%-5%. Most women also have one or two low risk conditions. This is why average breast cancer risk, across all women, is approximately 12.5%.For someone who has UDH alone, her risk will be 6% - 10% (a 1 1/2 to 2 times increase of 4%-5%). This remains lower than average risk. By comparison, someone who has ADH or ALH (atypical hyperplasia) has a breast cancer risk of 16% - 25% (a 4 to 5 times increase of the base risk of 4%-5%). This is why ADH and ALH are often considered to be high risk conditions. Additionally, because ADH and ALH so closely resemble breast cancer on imaging, whenever ADH or ALH are found in a needle biopsy, an excisional/surgical biopsy is done to remove the entire area. The concern is not the ADH or ALH, but the risk that some breast cancer might be hiding in the mix along with the ADH/ALH, undetected by imaging. In about 20% of cases, some DCIS and or invasive cancer is found along with the ADH. Most often it's just DCIS but I'm one of the ~5% of those diagnosed with ADH who ended up being upgraded to invasive cancer, although I only had a microinvasion. UDH cells, on the other hand, have an appearance that is much closer to normal cells than to cancerous cells, so the same risk that cancer might be missed doesn't exist.
You have to do what you feel is right, but I wanted to explain why your doctors have been unconcerned. Good luck with whatever you decide.
Edited to add: ADH is not tested for hormone receptors and in rare cases, sometimes even DCIS isn't. So it would be most unusual to test UDH for hormone receptors. I've been hanging around here for a long time and I've never heard of it being done.
An additional edit: When ADH is removed, the concern is not the ADH but the risk that something more serious might be hiding in with the ADH. ADH on it's own does not need to be removed, and if some is left in the surgical margins, there is no need for a re-excision. This is because the risk ADH confers remains even when the ADH is removed - the risk is a generalized breast cancer risk across both breasts. So women who have ADH removed during an excisional biopsy still have a 16%-25% breast cancer risk, because of the ADH. I don't know if the same is true for UDH - UDH is rarely ever removed. But since ADH is similar to but more advanced than UDH, if this is true of ADH, I expect it is true of UDH too. Therefore having surgery would not reduce the 1.5 - 2 fold risk increase conferred by the UDH.0