Best Of
Re: I say YES. YOU say NO....Numero Tre! Enjoy!
Thank goodness the European leaders are coming along with Zelensky tomorrow, so Trump can't go off on him like last time (or at least I hope they will call him out if he does).
Re: Can we have a forum for "older" people with bc?
Glad the laugh for the day brought smiles to some of you. I found it posted on a local Nextdoor and had a laugh, so I decided to share it. Never knew Dawn was the answer to my weight issue, but now know why my hands are slim.
Taco, belated happy anniversary. I loved the "romantic" gifts and have to say that we also exchange more practical gifts for birthdays, anniversary's and holidays. I asked DH to spring for a car detailing as a gift. Haven't done it yet, but intend to do it.
Home ownership does come at a cost but when you look at what rents are these days and that money is seldom spent on upkeep, it is an investment in yourself. When I loved in an apartment they would only repaint every 5 years and it was with really cheap paint that was unwashable and dirtied rather quickly. By 3 years, I ended up repainting it, which meant the next renter got a freshly painted apartment, because we found a house we liked within 4 months.
Sandy, your bathroom dilemma left me confused. I am still trying to figure out where you have a usable shower? It's a shame you couldn't get the riser replaced before they repaired the dining room wall.
I am so glad I have a DB who is a general contractor and has done so much work on my home. He is sometimes obsessive about the caliber of his work and has been known to redo something multiple times until he is pleased with the outcome. The floor in my eat in area has a walnut Celtic knot design in the wood flooring. It was the first time he had ever done one and he worked so hard on getting it right.
cindyny, love the photos and second what harley07 said. You have been to some areas in Ireland that we have not seen on our many trips there, so it is nice to see them. As far as your fence and garage repairs, you may find that your insurance company probably hasn't done much in your absence. Hopefully they will go after your neighbor's to recoup your deductible. Better you are home so you can supervise the repairs and contractors that way when issues arise you can clarify what is acceptable.
Joint family birthday party at Bonefish Grill was really good. We know the manager from eating there and also we booked the back room last year. It was available when we spoke to him awhile back and booked it. It is quieter than the main dining room so we can talk without having to yell. We had 2 servers and they were attentive. We let everyone order off the menu so everyone was pleased with their entree. I ordered Bang Bang Shrimp and Calamari for a shared appetizer and they seemed to enjoy it. I don't eat either because I am very selective about which seafood I eat so it is limited in scope. For dessert a few of us had mango creme brulee, others had the cheesecake with strawberry champagne sauce, DGD had a brownie (sans bourbon sauce, but lots of whipped cream) and DD had the Key Lime cake. I like their Drunken Coconut pie but will have that on my next visit. I am a member of their Rewards program and today's visit gave me a large reward towards our next visit. My dessert was free (and had a lit candle on it), I had a reward credit and then they was a credit towards the Bang Bang shrimp. Not sure what the latter was about but that was fine. Everyone left full and had a good time. I brought home half my meal, so I have a dinner for later this week. Had a lovely glass of Prosecco that hit the spot.
Guess that's all for tonight. I hope everyone had a great day.
Re: Can we have a forum for "older" people with bc?
Betrayal - thanks for the laugh. Since Dawn dish soap dissolves fat, perhaps I can drink it to dissolve my LDL cholesterol !?! 😜
Taco - Happy Anniversary!
Carole - the joys of homeownership! It’s always something and it always costs $$$
Sandy - same as I said to Carole above. There is always something to be fixed on a home. Crosby’s Kitchen sounds yummy. Have you been before? We don’t get over that way often but it might be worth a trip if you recommend it.
Cindy - keep the pictures coming! I am so enjoying traveling along with you.
Re: Double Mastectomy
Hi sweetie, I went through this 12 years ago, at age 47. It was not nearly as bad as I thought….surgery went well and I only needed couple of oral pain tablets for first few days. The drains were a bit of a nuisance but were out after week or so. Recovery fairly easy and really not much pain at all. I play a lot of sport so not having boobs bouncing around was a real benefit!! Not sure of your support system, but my husband was absolutely amazing, as were my four children. Not once did anyone question my choice to forego reconstruction….they just wanted me alive and happy. I have never regretted my decision and am at peace with it….I am more than a pair of boobs! Sadly, I lost my darling husband four years ago, however now have four grandchildren and live my life around my family. Happy to answer any questions you may have, if you'd like to message me :)
Re: Can we have a forum for "older" people with bc?
betrayal your laugh of the day was fabulous. Maybe dawn can deal with my weight gain issues from Letrozole. Yay more pizza and cheezies are in store for me with a swig o dawn!
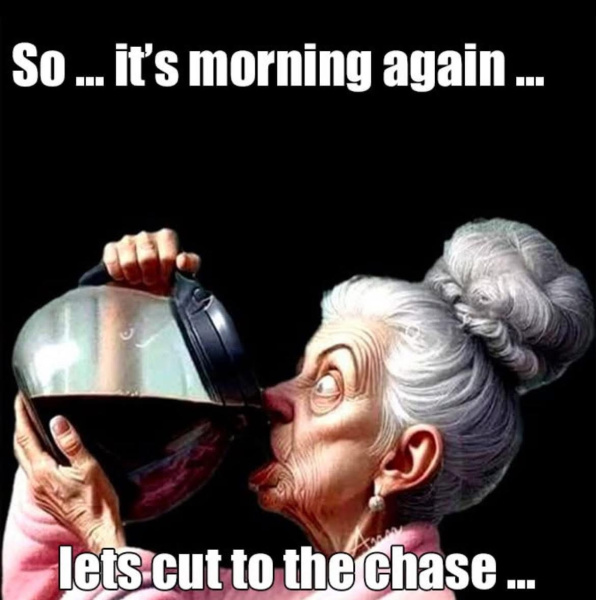
Super busy weekend at work. Always great when we are busy. But I’m exhausted now. Good thing I only work two days a week. Likely you will see this tomorrow so the photo is appropriate for the morning.
have a great week everyone.
Re: Can we have a forum for "older" people with bc?
Here's a laugh for today.
𝐃𝐨𝐧'𝐭 𝐰𝐚𝐬𝐡 𝐲𝐨𝐮𝐫 𝐡𝐚𝐢𝐫 𝐢𝐧 𝐭𝐡𝐞 𝐬𝐡𝐨𝐰𝐞𝐫!!! (𝐈𝐭'𝐬 𝐬𝐨 𝐠𝐨𝐨𝐝 𝐭𝐨 𝐟𝐢𝐧𝐚𝐥𝐥𝐲 𝐠𝐞𝐭 𝐚 𝐡𝐞𝐚𝐥𝐭𝐡 𝐰𝐚𝐫𝐧𝐢𝐧𝐠 𝐭𝐡𝐚𝐭 𝐢𝐬 𝐮𝐬𝐞𝐟𝐮𝐥). 𝐈𝐓 𝐈𝐍𝐕𝐎𝐋𝐕𝐄𝐒 𝐓𝐇𝐄 𝐒𝐇𝐀𝐌𝐏𝐎𝐎 𝐖𝐇𝐄𝐍 𝐈𝐓 𝐑𝐔𝐍𝐒 𝐃𝐎𝐖𝐍 𝐘𝐎𝐔𝐑 𝐁𝐎𝐃𝐘 𝐖𝐇𝐄𝐍 𝐘𝐎𝐔 𝐒𝐇𝐎𝐖𝐄𝐑 𝐖𝐈𝐓𝐇 𝐈𝐓 .....
𝐀 𝐖𝐀𝐑𝐍𝐈𝐍𝐆 𝐓𝐎 𝐔𝐒 𝐀𝐋𝐋!!! 𝐈 𝐝𝐨𝐧'𝐭 𝐤𝐧𝐨𝐰 𝐖𝐇𝐘 𝐈 𝐝𝐢𝐝𝐧'𝐭 𝐟𝐢𝐠𝐮𝐫𝐞 𝐭𝐡𝐢𝐬 𝐨𝐮𝐭 𝐬𝐨𝐨𝐧𝐞𝐫! 𝐈 𝐮𝐬𝐞 𝐬𝐡𝐚𝐦𝐩𝐨𝐨 𝐢𝐧 𝐭𝐡𝐞 𝐬𝐡𝐨𝐰𝐞𝐫! 𝐖𝐡𝐞𝐧 𝐈 𝐰𝐚𝐬𝐡 𝐦𝐲 𝐡𝐚𝐢𝐫, 𝐭𝐡𝐞 𝐬𝐡𝐚𝐦𝐩𝐨𝐨 𝐫𝐮𝐧𝐬 𝐝𝐨𝐰𝐧 𝐦𝐲 𝐰𝐡𝐨𝐥𝐞 𝐛𝐨𝐝𝐲, 𝐚𝐧𝐝 𝐩𝐫𝐢𝐧𝐭𝐞𝐝 𝐯𝐞𝐫𝐲 𝐜𝐥𝐞𝐚𝐫𝐥𝐲 𝐨𝐧 𝐭𝐡𝐞 𝐬𝐡𝐚𝐦𝐩𝐨𝐨 𝐥𝐚𝐛𝐞𝐥 𝐢𝐬 𝐭𝐡𝐢𝐬 𝐰𝐚𝐫𝐧𝐢𝐧𝐠,"𝐅𝐎𝐑 𝐄𝐗𝐓𝐑𝐀 𝐁𝐎𝐃𝐘 𝐀𝐍𝐃 𝐕𝐎𝐋𝐔𝐌𝐄."
𝐍𝐨 𝐰𝐨𝐧𝐝𝐞𝐫 𝐈 𝐡𝐚𝐯𝐞 𝐛𝐞𝐞𝐧 𝐠𝐚𝐢𝐧𝐢𝐧𝐠 𝐰𝐞𝐢𝐠𝐡𝐭! 𝐖𝐞𝐥𝐥, 𝐈 𝐠𝐨𝐭 𝐫𝐢𝐝 𝐨𝐟 𝐭𝐡𝐚𝐭 𝐬𝐡𝐚𝐦𝐩𝐨𝐨 𝐚𝐧𝐝 𝐈 𝐚𝐦 𝐠𝐨𝐢𝐧𝐠 𝐭𝐨 𝐬𝐭𝐚𝐫𝐭 𝐬𝐡𝐨𝐰𝐞𝐫𝐢𝐧𝐠 𝐰𝐢𝐭𝐡 𝐃𝐚𝐰𝐧 𝐝𝐢𝐬𝐡𝐰𝐚𝐬𝐡𝐢𝐧𝐠 𝐬𝐨𝐚𝐩 𝐢𝐧𝐬𝐭𝐞𝐚𝐝.
𝐈𝐭𝐬 𝐥𝐚𝐛𝐞𝐥 𝐫𝐞𝐚𝐝𝐬,"𝐃𝐈𝐒𝐒𝐎𝐋𝐕𝐄𝐒 𝐅𝐀𝐓 𝐓𝐇𝐀𝐓 𝐈𝐒 𝐎𝐓𝐇𝐄𝐑𝐖𝐈𝐒𝐄 𝐃𝐈𝐅𝐅𝐈𝐂𝐔𝐋𝐓 𝐓𝐎 𝐑𝐄𝐌𝐎𝐕𝐄." 𝐏𝐫𝐨𝐛𝐥𝐞𝐦 𝐬𝐨𝐥𝐯𝐞𝐝! 𝐈𝐟 𝐈 𝐝𝐨𝐧'𝐭 𝐚𝐧𝐬𝐰𝐞𝐫 𝐭𝐡𝐞 𝐩𝐡𝐨𝐧𝐞 𝐈'𝐥𝐥 𝐛𝐞 𝐢𝐧 𝐭𝐡𝐞 𝐬𝐡𝐨𝐰𝐞𝐫!!!