When do most recurrences for HER2 happen
Comments
-
Sue - just wanted to say, yes, me to... random bone and joint pain... all fleeting - nothing that lingers, but definitely notable. I didn't realize it may be the herceptin until I read this... thought maybe the tamoxifen (and of course, the dark places my mind can take me!).
0 -
Sue-
I finished my herceptin at the end of Nov. I had the muscle and joint pain all along. My doctor kept saying it was from sudden chemo menopause and not the herceptin. I disagree. I did tons of research on this and so many women have the same symptoms. It is also on genentechs website as a side effect. I had burning in my quads like I had run ten miles. I still have it a little bit but it is slowly getting better. I also had a steroid like facial swelling and that is finally starting to go down.
I don't know why they tell us its not from the drug. I know herceptin is a wonder drug and I would have used the drug no matter what.
Good luck!
0 -
Onas; ALL
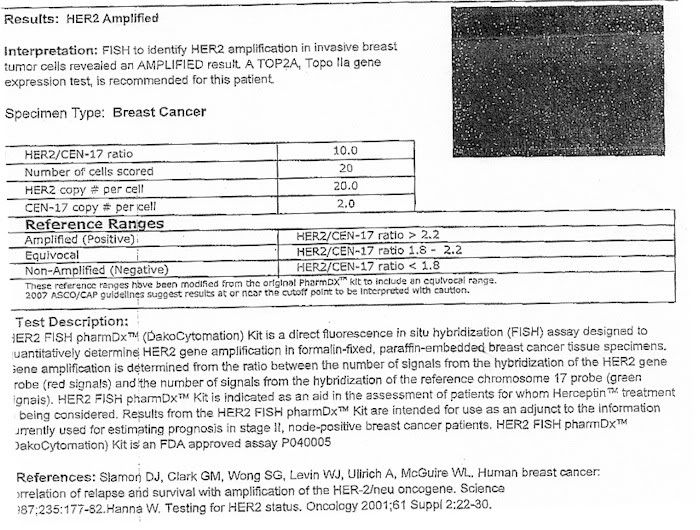
In reading this thread, my confustion factor has gone up regarding my FISH results so I am posting a copy of the path report I received.
Will someone please decipher it so that I can see the relevance to the reference ranges listed on it? I have redacted only personal info. Thanks.


 0
0 -
OOPS...that should have been posted to Omaz! Sorry for the typo.
0 -
On my path it says:
--------------------
Results of reported as HER-2/neu: chromosone 17 cetromere probe signal ratio
Not Amplified = less than 1.8
Equivocal = 1.8-2.2
Amplified =greater than 2.2
---------------------So it looks like on your path you posted says your ratio is 10. That seems pretty postive to me but I might not be understanding this right. Did you ask your onc?
0 -
Lago
As is shown on the image I posted the reference ranges are the same as on your report. The "10" score on the original FISH report just doesn't make sense to me, given the ranges.
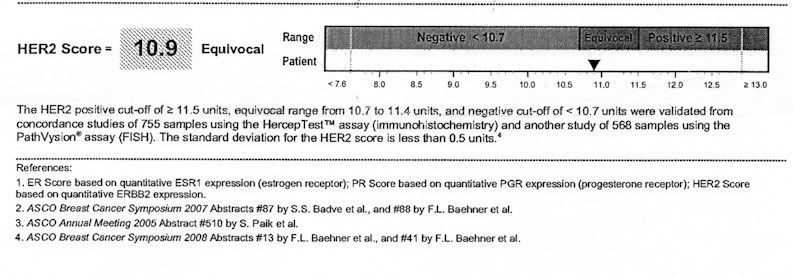
I have a new Onc who hasn't seen the FISH report, he picked up the score from the surgery path report. I didn't question the score until I saw this OncotypeDX score as just barely equivocal with positive beginning at 11.5. (see the bar graph). My original IHC score was equivocal at 2.7 also.
 0
0 -
worldwatcher - The scale for the oncotype and FISH are different, so the 10 for FISH and 10.9 for oncotype are not measuring the same thing as I understand it. If the FISH result is accurate then yes your sample was positive - ie amplified for HER2. I *think* for the FISH they look at a certain number of cells from your tissue. Within those cells they determine how many copies of HER2 gene there are (stain red) and how many copies of chromosome 17 centromere (center part, stain green) there are. Each cell should only have 2 of chromosome 17 which you cells have but apparently your cells have 20 copies of the HER2 gene (I think 2 would be normal?). So then they compute the ratio, 20/2=10 which is an amplified result - the HER2 gene is amplified, there are more than the expected number of copies of the gene in each cell. Again, it is confusing that you have a definitely positive result from FISH and equivocal by OncotypeDX. If they are BOTH accurate and not from mixed up sample or something then maybe ?? your tumor may have had some HER2+ and some HER- sections if that is possible. This is for sure something to talk about with your oncologist!0
-
That's screwy. You really need to talk to your onc. I know there can be different results for FISH depending on how the sample was handled.
Was your biopsy sample also tested for HER2? I know both my biopsy sample and the tumor from the BMX were both tested and had the same HER2+ results.
0 -
worldwatcher and lago - I only had one test on my biopsy sample, they did not repeat with the tumor after surgery.0
-
Thanks ladies for your responses...
Omaz
ONLY the oncotypeDX test was run on my actual tumor cells. The IHC and FISH results came out before the surgery from the biopsy sample. Also, the surgery path report noted that there was a DCIS component of "less than 5%. I suppose the biopsy sample which generated the FISH report could have contained some of the DCIS.
This is what has concerned me...the surgery path report just picked up the biopsy findings. The Oncotype test was done on the actual tumor sample.
This will not affect my immediate treatment as I am not doing chemo now, but if/when there is a recurrence it would have been nice to have had a FISH result on the actual tumor sample rather than the biopsy.
I feel that I was somewhat let down by the medical community here in the beginning....I had an appointment with an Onc. just a week after surgery and they called the day before the appointment to tell me my insurance was no good with them....then, the search for another oncologist was slowed because I couldn't get decent references for the oncs that WERE on my insurance (Medicare/Advantage) plan. I saw one oncologist who was prepared to just add me to the "factory protocol" without considering my wishes.
I finally found a doctor that I like and trust who IS on the plan, so we are moving forward with Tamoxifen. I AM happy with my radiology doctors and my surgeon has an excellent reputation and at six months I am having no problems with either the surgery or the APBI (Accelerated Partial Breast Irradiation).
I have an appointment next week with my Onc. and will discuss all this with him. They were kind enough to send me the test results so I could digest them beforehand.
Again, thanks for walking me through this.
0 -
I think there is a risk for the rest of our lives--I was in "remission" for 22 years, 10 months and 27 days from first occurance to reoccurance.
0 -
worldwatcher - I hope it was helpful. I guess I would lean toward the oncotype result since it was done on the removed tumor cells. Let us know what the doctor says!0
-
All of this talk of FISH and Oncotype has me feeling kind of dumb. I don't know my Her2 numbers. They told me I was positive, and I just went with it. I do know my ER was only 12% but like many have said on the boards - any ER+ % makes you ER+. I guess maybe for me it wasn't such a big deal to know my Her2 numbers because I had 2 positive nodes. This meant I was having chemo for sure no matter what. That's also why they didn't even do Oncotype on me.
Do you guys think I need to know my Her2 levels for anything? One thing that bothers me is that my onc insists that Tzmoxifen is right for me for now, but I have read about Her2 responding better to AI's. And now that I have had my hysterectomy (last week) I could really do either. I keep wondering if I should be switching...
0 -
For all the newly diagnosed HER2 gals, many many notable Oncologists do not like Tamox with Her2 and there have been 2 studies that have shown where Tamox actually fueled the Her2 cells. One such study referred to poor Metabolizers of Tamox. If you go back on the Her2 thread to last year you can find Orange1's very helpful thread on this. If you are Her2 and your Onc is giving you Tamox, at the very least I would have the Metabolizer test done.
My Onc who is nationally renown will NOT allow Tamox with Her2.
0 -
Important for Her2+ on TamoxifenThe above is the name of the thread started by Orange1 on page 11 of the Her2 topics.0
-
worldwatcher the test from your actual tumor after surgery is more accurate. You are absolutely right that the DCIS could have been HER2+ but not the IDC and that was the sample that was tested.
saralmom The only reason why I do know my numbers is because of all the talk and I do have a copy of my path report. I don't think it really matters what your exact numbers are.
Thanks mmm5. Here's the link for anyone interested http://community.breastcancer.org/forum/80/topic/742141?page=1 For those of you who are on Tamoxifen don't panic. Ask your oncs and read the entire initial post. Some HER2+ do well on Tamoxifen. Also we don't know how old that reseach is. New studies may have come out… that's why you should ask your onc.
0 -
Yes Absolutely, do not panic!
I know many many Gals on Tamox and have been dxed Her2 positive! Many on this board in fact are doing great with this regimen and two of my friends did tamox for years after dx and are both doing well 5 and 6 years out.
Just remember to ask all the questions and be your own advocate.
0 -
Post deleted because of newer info on thread.
0 -
Thanks for all the info everyone. Will for sure follow up again with my onc. But she was insistent that she doesn't give credence to the studies about Her2 and Tamoxifen. Also, she says that she doesn't really trust the metabolizer tests. She is young and up to date, so I trust her. Just need to hear her say all of this again.
I do have my path report from my biopsy, but I never followed up to get a copy after surgery. I need to do that. I want to have it all in my files just because. I can't explain why I didn't make sure to get it other than that in the moment and the chaos I just let it go. Time to get back on top of all that. (A year later!!!! yikes)
0 -
worldwatcher - I thought your post was very helpful.
0 -
I'm glad you found my post(s) helpful...I think at the very least they have illustrated the fact that there can be more than one test result that affects an individual's treatment.
I see quite a few posts here that believe there is overtreatment of some BCs. In my case, I have migitating factors that preclude an automatic jump into the chemo/Herceptin protocol, and have gone from little hope of defeating the HER2+ because Herceptin won't be allowed without chemo to the renewed hope that the new test result will mean that my very life does NOT depend upon receiving Herceptin.
That's a very major change for me, and I pray it will be true.
On another note, the original biopsy test showed me with a weaker ER situation than is shown on the OncotypeDX. Does anyone know if the higher ER score will be beneficial in the use of Tamox and the AI's?
0 -
Re: Her2+ and Tamoxifen,
Because of new conflicting data about the importance of CYP2D6 metabolizer status on outcome in patients taking tamoxifen, most oncs will not order the test or use it to decide which patients should have tamoxifen.
To panic or not if you are Her2+ and on tamoxifen....
One important thing to keep in mind is that in all three of the big adjuvant trials that tested Herceptin vs no Herceptin, almost all of the premenopausal women who were hormone receptor positive received tamoxifen, not an AI. And as a group they did quite well. In both the Joint Analysis trial, and the HERA trial, Her2+ hormone receptor positive (HR+) did a little better overall than Her2+ hormone receptor negative (HR-) patients. If tamoxifen was generally bad for Her2+ women, the results for these women would probably have been worse, not better, than for HR- women. In the third large adjuvant trial - BCIRG0006 - the results for HR+ and HR- were not reported separately, so we don't know which group did better.
So where do we stand now? We have 3 large trials Herceptin trials where the vast majority of HR+ premenopausal women received tamoxifen. In two of the trials, the HR+ women on tamox fared quite well. In the third, we don't know how they fared vs. HR- (but no reason to believe they did any worse).
As far as I know - and someone please correct me if I'm wrong - there is no well conducted study (large, prospective) that has shown that Her2+ women do better on an AI than on tamoxifen.
What about tamoxifen causing increased tumor growth in cell culture (and even in mice, as it turns out)? Well, as mentioned in other threads, tamoxifen needs to be metabolized to its active form - endoxifen - to be active. The conversion cannot take place in cell culture, nor in mice. So in these models of tumor growth, the tamoxifen is was never converted to its active form. Thus these models are not useful for understanding the activity of tamoxifen in humans.
Bottom line if prescribed tamox....don't panic, odds are you will do well.
0 -
I have been following the tam and herceptin problems on MD Link Oncology and it seems that some are resistant to one or the other or both but it involves a lot of genetic testing. MD Anderson (4-12-10) reported that overexpression of micro RNA 21 gene PTEN is associated with a poor response to Herceptin. Cancer Research (2-1-10) reports that receptors erbB2, erbB3 and insulin-like growth factor 1 receptor is linked to resistance to herceptin. I asked my daughter's 1st onc about this and she said that the laptinib + herceptin double blockcading is only in trials now - the ALTO trial, so, obviously, resistance is an issue for some. Dr Zhen Fan at MD Anderson seems to be a leader in this research.
As for Tam, Am society for Biochemisty and Molecular Research (6-10-09) -study to identify the potential for tam resistance, triple positives don't metabolize well; Health and Medicine (4-2-09) cholestrol appears to promote tam resistance.
What all this shows is that reseachers are studying the problems. I am going to ask about more genetic testing; even if it is part of a reseach stud, it could be useful info.
I worked in research during grad school, so I do know the limits of published studies, but we should keep up to date on it and ask questions.
0 -
omaz
You got that explanation about FISH test right on the button, great way to explain it, it is all about the "red" and "green" stain! Maybe you should go into oncology.
0 -
3daywalker - Thanks, that makes me feel better, I wasn't exactly sure if I was explaining it right.0
-
Just found this thread and thought I'd chime in on the original question of recurrence. My onc said that after three years the risk for HER2 women really drops dramatically. She said the 3 year anniversary is a bigger deal than 5 years for HER2.
She also said year 2-3 is the highest risk period which was news to me. She said she doesn't often tell patients that but I was asking. So I am 2 1/2 out from diagnosis and counting the days for my 3 year anniversay this summer!
0 -
deekaay - Thanks, good to know!0
-
Is the 2-3 years for HER2+ hormone negative AND hormone positive? It would make sense that 2-3 years is the most crucial for HER2+ negative then fall of after that… I believe it's the same for triple negatives too.
0 -
I have also been reading about PTEN in tumors. The lack of this tumor suprressor gene makes the cancer resistent to Herceptin and being that the recurrence rate for Her2+ before herceptin took place between 8 months and three years, it makes sense that the first three years recurrence free are significant. I wish they had a test for this PTEN marker so we could know if our treatment will work.
0 -
Yes it doesn't make sense but for triple positive I'm not sure the risk goes down as much as a hormone negative after 3 years.
0