TRIPLE POSITIVE GROUP
Comments
-
I'm never out of the Cancer Center faster then 2 hours and if I have to see the Doc and get labs, count on a good 3 - 3.5 hours.
0 -
Big Peaches- herbalist here, black cohosh is a big NO for us hormone positive women as it contains phytoestrogens (like soy does). While there's some controversy regarding phytoestrogens hurting or helping hormone positive breast cancer in general, (as phytoestrogens can actually help LOWER estrogen in high estrogen women), for women already on endocrine therapy, all they do is add estrogen back into the system (albeit weakly), which is how they help alleviate hot flashes.
0 -
Severe Hot Flashes: anyone have any solutions other than gabapentin, oxybutynin, Effexor or Paxil? I was going to try black Cohosh, but since HeartShapedBox said that's not a good idea, I won't.
I have been approved for SBG Nerve Block (Stellate Ganglion Block) which is suppose to ease Hot Flashes (50% chance it will work) but Can't get a ride to the specialized doctor. Any Suggestions out there?
0 -
rljes, There has been some that say Vitamin E has helped with Hot Flashes ... mine are coming more frequent and the night sweats are awful!
BE CAREFUL if you are in active Chemotherapy, it is an antioxidant so my Onc said I have to wait until all Chemo is done, 1 more Chemo then just H&P.
https://www.ncbi.nlm.nih.gov/pubmed/17664882/
https://www.medicalnewstoday.com/articles/317864.p...
https://www.livestrong.com/article/337453-is-vitam...
0 -
Hi Kimmh012 - - thx for the feedback -I've been taking Vit E for years, and I've finished chemo/Herceptin almost a year ago. Not starting Tamoxifen until I can get my hot flashes under control. They are so severe I have panic attacks if I'm out in public, so I've become a hermit. ( also have tried acupuncture)
I'm almost to the point of taking Estrace Pills again. I'm that desperate.
0 -
Re Vitamin E and hot flashes https://www.breastcancer.org/tips/nutrition/supplements/known/vit_e
"Vitamin E does not appear to be effective for treating hot flashes in women who have had breast cancer."
Rljes - My MO prescribed Clonidine transdermal for me. Can't say for sure whether it helped or not; I had to discontinue due to skin burns from the patch.
Just increased my Effexor from 37.5mg to 75, and switched my AI to Femara because hot flashes are an issue for me, too.
0 -
0
-
Magari, thank you for that information.
Rljes, Sorry this has taken such a toll on you, praying you find relief soon.
I just purchased a necklace mini fan and an essential oil inhaler "balance" that was suggested by some women in my support group, at first sign of hot flash that usually starts on the back of my neck, I use it, so far so good.
HAVVA Balance, Nasal Inhaler with Synergy Blend of 5 Essential Oils to Reduce The Effects of Hormones in Women https://www.amazon.com/dp/B07GJP139X/ref=cm_sw_r_cp_apa_i_c..IDbR1GK1JM
0 -
Jumpship.
I take a small dose of Ritalin (https://www.drugs.com/ritalin.html) twice daily. It keeps me focused and when I feel tired I can still accomplish what I set too.
Coach Vicky
0 -
Jumpship/Coachvicky--who is prescribing (or will prescribe)? I've heard of this, am very interested, but don't know if I should talk to my MO about it or my PCP. (I thought I was doing relatively well energy-level/fatigue-wise but had a wedding last weekend absolutely ruined because of the overwhelming fatigue. Kind of a bummer. Some of my kids have had ADHD meds in the past and I like that you can take it on an as-needed basis.)
P.S. Coach--what dosage are you using?
0 -
HeartShapedBox, thank you for the info, that's what I was afraid of. It's still in the upper 90's here (Fall, where are you??). It seems my only option is to sleep naked! LOL
0 -
Correction to my earlier post.
I got my Rx bottle, I am actually taking Adderall Xr Caps, 10mg, twice a day..
Here is a comparison chart I found that may help as to what to ask: https://www.diffen.com/difference/Adderall_vs_Rita...
Vicky
0 -
thx for the info, unfortunately I can't take clonidine, it lowers BP and mine is low enough (90/60) - I too have a mini fan attached to my purse and one of those cooling scarfs I wear when I have to go out. The night sweats are horrific. at least twice a night I wake up drenched from head to toe, and have to change clothes and sheets. its exhausting. (I can't sleep nude - I'll have 'naked dreams") I have a window a/c as low as it can go, box fans and a ceiling fans going. Counting down the days till winter.
Its just hard to believe after all these years of women going thru menopause, they can't come up with something that will work.
0 -
I have a question... sorry if it’s ridiculous. If someone who’s triple positive gets neoadjuvant chemo and Herceptin treatment, is it possible for the HER2 status to “die off” and only be left with HR positivity? Or is that not how these things work at all? Apologies!
Additionally, is there a way to see how well endocrine therapy is working or works for a specific person?
0 -
Hi 1207262!
Cancer cells can mutate after treatment, so it's possible that HER2+ cancer cells could become HER2-. However, I know of several HER2+ breast cancer patients who suffered recurrences, and their cancer returned as HER2+.
If you want to know how well endocrine therapy is working, it may depend on whether you're doing Tamoxifen or an AI. I'm doing both ovulation suppression (OS) + an AI (Aromasin), and my doctor has tested to see how much estrogen is in my blood. If the OS + AI are doing their job, I should have very low levels of estrogen, if any.
0 -
thank you for your reply ElaineThere!
That makes sense about the estrogen. Thank you!
For the receptor status question, I meant more about current treatment, not a Recurrance. Sorry if that was unclear!
For instance, if someone who’s +++ undergoes chemo+Herceptin and is tested again, could they possibly come up as HR+ and Her2- before continuing on treatment (mastectomy and endocrine treatment etc)?Also, I was asking about estrogen blockers effectiveness in regards of concern for “crosstalk” resistance. I’ve read about this online and it’s frightened me that the endocrine treatment won’t work as well for triple positives… the Tumor is very strongly both ER+ and PR+ I think 97% and 90% respectively. The HER2 status was 2 on ICH so they had to send out for the second test and it was positive for FISH
Thank you!!!!!!
0 -
additionally, if someone who is +++ takes nernylx and an endocrine therapy, would there be any sort of “crossing each other out” effect there? Would they preculde one another’s effectineness at all? Can they be taken concomitantly? Sorry for the spam! Thank you!
0 -
hello ladies,
Noticed this morning my scanxiety creeping up on me. I'm 4 years out from treatment, and at my last annual scan, the radiologist saw something small she didn't 100% like, and so for the first time I got "come back in 6 months" to have a rescan of my left breast.
That appointment is about three weeks from now. I haven't told anyone - not my mom, not my husband, not my best friend. I'm too afraid they will all panic. I went over my last scan with my MO for almost an hour after I had it to really make sure we should wait six months...I felt comfortable then, but now I'm kicking myself...why didn't I just do a biopsy then? Sigh...because I was tired of being sick, and I didn't want to be touched anymore...that's why...
I'm sure it is fine, but I feel jumbled, and anxious, and well, alone. I have been having nightmares.I feel better now that I have told all my +++ peeps. God I hate this sh*t.
Tres
0 -
1207262 - I had my tumor retested for Her2 after neoadjuvant chemo and it came back negative. It was IHC negative (1+) and FISH negative on my original biopsy, IHC equivocal (2+) and FISH postive on a second biopsy a couple months later (which put me on TCHP), and then FISH negative at surgery. I have no idea if it was really negative the first time, if it changed after 1.5 months of neoadjuvant hormone therapy, or if it was heterogeneous all along. My guess is that it was always heterogeneous.
I am currently taking Nerlynx and anastrozole (and zoladex). I believe most, if not all, of the HR+ women in the Nerlynx study would have been taking hormone therapy as well. I also took anastrozole while I was finishing up Herceptin.
Tres - I'm sorry. I hate this sh*t too. I got anxiety over my freaking blood draw a couple weeks ago. I try not to think about it but it's hard not to.
0 -
Tres ... if it was REALLY REALLY REALLY suspicious, you would not have left without a biopsy right then and there! This is most likely "caution."
My prayers for you.
Vicky
0 -
1207262 - I don't think the administration of Herceptin necessarily causes the Her2+ aspect to "die off", rather the mutation may change in recurrence, and agree with ET that is where you would most often see the change in receptors and Her2 status. That is not to say that there are not patients who fail to respond to either Herceptin and other targeted treatments and/or anti-hormonals, there certainly are, but they are not the majority. That said, it is possible to see changes in status after neoadjuvent treatment, particularly if the receptors and/or Her2 are not particularly strongly present. If you are wondering about this you should certainly request new testing of the tumor post-surgery. It is important to know that tumors are often hetergenous so whatever slice is looked may not be indicative of the tumor in whole - some parts may express homone receptors and Her2 positivity more strongly than others. Is your mom post-monopausal? Has there been discussion of the approach to anti-hormonal therapy? I believe most of the crosstalk look has been at Tamoxifen, and I know my oncologist favors the aromatase inhibitors for his Her2+ patients.
tres - sorry you are dealing with scanxiety - it is hard. Crossing my fingers for everything to go smoothly and this be nothing. I feel ya - my labs are wack, indicating bone issues. My MO wants a bone scan and I have been resistant, wanting to try manipulation of my Vit D and weight bearing exercise first. All I am doing is putting off the inevitable scan, and I too am over it this far down the road.
0 -
Thank you for your response. I've been lurking a while and I admire how knowledgable you are and your helpfulness on these boards! She is premenopausal, but she is very into preventative measures. There is discussion about ovary removal and then an AI. I've read some studies that those cause problems with triple positives as well, which deeply concerns me. It is my (albeit crash-course-internet-educated) opinion that the tumor is more hormonal driven than HER2. The percentages are very high for both ER and PR (which, does that mean anything in regards to responsiveness to medication?).
The pathology report from the biopsy also states that there is DCIS involved. I've read that DCIS is much more likely to be HER2+ than IDC. Is it possible that the DCIS is the HER2+ and not the IDC? Also, would that make any difference? There was only one biopsy so far, however. I assume they used the same "sample" for the ICH test, the HR testing, and the FISH test. My knowledge is limited on these things- I'm a digital media major (but I do work in a pharmacy!) lol.
Additionally, do you think there is a benefit (or is there any evidence of benefit) for ovary removal alongside an AI for stronger preventative measures?
The "game plan" thus far is neoadjuvant chemo-herceptin(the usual combination, I'm not sure exactly the official drugs involved right now, it's slipping my mind) scheduled for tomorrow, granted the all-clear from one more test. Depending on the response of the neoadjuvant treatment will guide the next steps before and after surgery (either a single or double masectomy- she doesn't want to deal with the possibility of a second primary and does not want reconstruction).
I'm concerned about the subtype of the tumor (Luminal A, Luminal B, or HER2+ driven) and wish there was a more commonplace way to test this out. My mom won't push for these things because she's very trusting in the medical community and that they know best, especially since we're at one of the best oncology hospitals in the United States and her doctor is the head of the Breast Cancer department there. I, however, want answers! I want individualized treatment! Wish it was the norm! It should be!
SpecialK, also-- I hope everything goes well with your bone vitamin levels!
TresJoli2-- I understand the scanxiety. I'm awaiting some results right now too and I'm so anxious I could throw up. I'm praying all goes well for you, too!!!
Hapa-- thank you for your answers as well. It is so confusing to me how these things change so much. Praying all is/stays well for you, too!
You ladies are all a blessing! Thank you and prayers for all to be/stay well!!!
0 -
Hello, I was just wondering if there were any ladies out there who have had neoadjuvant chemo? I've finished the chemo but I'm still on herceptin, pertuzamab and tamoxifen. I'm pre menopausal and I was offered ovary suppression instead of tamox but I chose the latter. I've read conflicting reports that tamox might not be the best if her2 positive as well. I was just looking for success stories from ladies who were er+ and her2+ who had neoadjuvant chemo and then a year of herceptin and 5-10 years of tamoxifen. I had pcr in the lymph nodes but there was still a small amount of tumour left in the breast. Many thank
0 -
sejay - look at the signature lines of the people on this thread, you will be able to see who had neoadjuvent chemo and Tamoxifen or AIs, and what their dates of treatment were. Keep in mind that your neoadjuvent treatment was likely because you received Perjeta. Prior to the approval of Perjeta for early stage treatment it was unusual to do chemo and Herceptin neoadjuvently - look back at the beginning of this thread and you will see the majority of us had surgery first. While pCR is desirable and potentially indicative of successful treatment, neoadjuvent treatment with targeted therapy was not designed to eradicate the tumor in the breast - it came about as current methodology to quantify whether adding Perjeta to Herceptin could increase successful treatment. Chemo and targeted therapy is a systemic approach - surgery is for operable tumor removal.
1207262 - you are most welcome - I've said it before, will say it again, helping others who have come behind me is my silver lining! The learning curve is steep, but you are asking great and informed questions, so good for you!
As far as the Tamoxifen versus AI question I will say my MO prefers the AI. I had already had a hyst/ooph years before diagnosis with breast cancer, but either ooph or ovarian suppression is an option that should be considered when deciding which type of anti-hormonal med to use. Worth a discussion with the oncologist. I had BCI testing done at the five year point to help determine whether to add additional time to my anti-hormonal therapy. I needed to take a holiday from Prolia injections because I had been on it quite a while (I had osteopenia that worsened after chemo and the first six months of Femara, so started Prolia to help stregthen bones and it helped tremendously) and I suggested switching to Tamoxifen to see if it would help maintain bone health, and he flatly refused. Of course, this is one opinion, but this is something you should discuss with your mom's oncologist as there are a number of factors used in determining which medication to go with. There are certainly folks on this thread who have done very well on Tamoxifen. There is also some segment of the triple positive population that would never recur even if they didn't take anti-hormonals. Unfortunately, we are not at the point of being able to figure out who that is, so we all take the meds and hope for the best.
On the subject of high ER and PR, the high ER supposedly helps responsiveness to anti-hormonal meds, and the high PR generally means the tumor is possibly less aggressive than low PR, and also helps responsiveness. It is also important to understand how percentages of ER and PR are derived - essentially the pathologist looks at 100 cells under the scope, and counts the ones with a receptor. say 90 out the 100 have a receptor - 90% ER+. It is possible that a slide of cells taken from a different part of the tumor could yield a more, or less, positive result. Here is some study info:
"In the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-14 trial, a randomized phase III study of tamoxifen vs observation in women with HR-positive breast cancer, the levels of ER expression, analyzed by quantitative reverse transcriptase polymerase chain reaction (qRT-PCR) analysis, was also predictive of tamoxifen benefit.[11] A relationship between ER expression and response to endocrine therapy was also observed in neoadjuvant endocrine studies of aromatase inhibitors including letrozole and anastrozole.[12-14] Interestingly, compared with tamoxifen in the neoadjuvant setting, aromatase inhibitors may be able to induce a response in tumors with lower levels of ER, although the sample sizes in these studies do not allow for robust conclusions in this regard.[12]"
As far as DCIS and IDC, since it is the IDC that is driving these decisions (chemo & Herceptin) I believe they would be making sure that this is what is being tested before subjecting your mom to harsh systemic treatment, I wouldn't worry too much about them using the DCIS portion. Pathologists can tell the two from each other, and many of us with IDC also have DCIS present - I definitely did. Even though there was one biopsy, they should have been multiple "cores" done of the tumor ( I had 6 cores taken) and DCIS and IDC look different from each other. Lab testing does not use the same exact area - thus the multiple cores. If staining is done that particular piece of the specimen is now fouled for subsequent testing. If you wish to learn the subtype some pathologists will expand on that, or you can request a Mammaprint. I was fortunate that my oncological breast surgeon happened to be participating in a study with Agendia, so I had Mammaprint done, which included my subtype. It is an expensive test so it is important to determine whether insurance will cover it.
Thanks for the good wishes about the bone issue - I have had elevated alkaline phosphatase for a while, which is generally not a good thing. It may have been caused by some dental work (which is what I am hoping, and that I am a slow at recovering) but can also be parathyroid problems, or a signal of mets. Bleh...
0 -
SpecialK: when you mentioned "elevated alkaline phosphatase", how large is it to be considered as "elevated"? My wife's was 83 on July 5 when she finished the last HP infusion but on Friday when she had follow-up with the MO, the alkaline phosphatase changed to 91. It is increasing (although it seems to be in the range 45-117). We just got the result and had no chance yet to ask the MO, but would it be something to be concerned about?
Thank you very much!
0 -
Thank you again for your thorough response, SpecialK! Curious, you mentioned you had the opportunity for a MammaPrint. Correct me if I’m wrong, but that’s similar to an OncoType Test? I thought those types of tests only worked on Hormone Positive, HER2 *NEGATIVE* tumors?
I’m also confused, I digress, about how a tumor’s Grade can change after chemo or any neoadjuvant treatment.
Additionally, I know pcr is harder with HR positivity, but does anyone know the benefits a hypothetical pCR gives a triple positive patient?
Thank you!!!
0 -
lilych - fluctuations within the range are totally normal, particularly when receiving treatment. When I say mine were elevated, at the highest it has been 50 points above the high end of the range. Trending with labs is important to watch though and if your wife’s numbers continue to rise it is something to discuss with your MO.
1207262 - OncotypeDX is indeed limited to patients who are ER+ and Her2-, but Mammaprint is a different test without those limits. Since the purpose of genomic testing is to determine the usefulness of chemo it is not usually done for Her2+ or for ER- because chemo is usually a certainty. Here is some additional info:
 0
0 -
That's super interesting and good to know about MammaPrint vs OncoType. We're blessed to have good health insurance, so I will bring that up to see if there is a chance that we're covered for that. Thank you!
Additionally, I found this data interesting. I don't know if anyone's ever seen it before, but it's some SEER data. I've seen other statistics classify Luminal B as ER+/PR- or triple positive or high Ki. In this particular data, it looks like they've grouped it into specifically triple positives as Luminal B.
https://seer.cancer.gov/statfacts/html/breast-subtypes.html
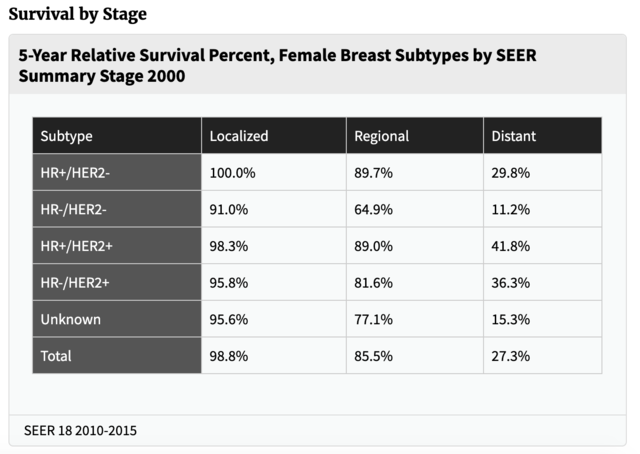
I found this table very interesting as well. Statistically (whereas of course every individual is different) from 2010-2015 data, the rates based on stage are almost the same for HR+/HER2- patients as triple positives.
0 -
SpecialK, thank you. The doctor confirmed it is not a concern, either, especially my wife is having fungal treatment.
I did go back and check the numbers during the chemo last year and it happened once the number was also 50 points higher than the high end of the range.
0 -
1207262 - One thing to keep in mind is that the term subtype can mean different things. There can be subtypes of hormonal and Her2 status within the disease of breast cancer, which is a classification like triple positive or triple negative, and there are further molecular subtypes within each kind arrangement of receptors that is the genetic expression independent of receptor status. Triple positives can be Luminal A, Luminal B, or ERBB (Her2+). I don't believe SEER data is captured by molecular subtype, rather in the table above they are showing hormonal receptor and Her2 status stats. I don't believe SEER data would include molecular subtyping because it is not routinely done for all diagnosed patients. The reason triple positives now have survival that is relatively the same as ER+/PR+/Her2- patients is because of Herceptin. Those stats would not likely include as many patients who received Perjeta as it was approved for early stage patients in late 2013.
Here is some info from BCO on molecular subtyping:
"There are five main intrinsic or molecular subtypes of breast cancer that are based on the genes a cancer expresses:
- Luminal A breast cancer is hormone-receptor positive (estrogen-receptor and/or progesterone-receptor positive), HER2 negative, and has low levels of the protein Ki-67, which helps control how fast cancer cells grow. Luminal A cancers are low-grade, tend to grow slowly and have the best prognosis.
- Luminal B breast cancer is hormone-receptor positive (estrogen-receptor and/or progesterone-receptor positive), and either HER2 positive or HER2 negative with high levels of Ki-67. Luminal B cancers generally grow slightly faster than luminal A cancers and their prognosis is slightly worse.
- Triple-negative/basal-like breast cancer is hormone-receptor negative (estrogen-receptor and progesterone-receptor negative) and HER2 negative. This type of cancer is more common in women with BRCA1 gene mutations. Researchers aren't sure why, but this type of cancer also is more common among younger and African-American women.
- HER2-enriched breast cancer is hormone-receptor negative (estrogen-receptor and progesterone-receptor negative) and HER2 positive. HER2-enriched cancers tend to grow faster than luminal cancers and can have a worse prognosis, but they are often successfully treated with targeted therapies aimed at the HER2 protein, such as Herceptin (chemical name: trastuzumab), Perjeta (chemical name: pertuzumab), Tykerb (chemical name: lapatinib), Nerlynx (chemical name: neratinib), and Kadcyla (chemical name: T-DM1 or ado-trastuzumab emtansine).
- Normal-like breast cancer is similar to luminal A disease: hormone-receptor positive (estrogen-receptor and/or progesterone-receptor positive), HER2 negative, and has low levels of the protein Ki-67, which helps control how fast cancer cells grow. Still, while normal-like breast cancer has a good prognosis, its prognosis is slightly worse than luminal A cancer's prognosis."
On the Mammaprint testing, you might also check with Agendia to see if they can reduce or eliminate the cost of the test if your mom's insurance will not cover it. Because the test is used to determine benefit of adding chemo to treatment insurance will often not cover it for those for whom chemo is a certainty.
lilych - one of the reasons most oncologists pull periodic complete metabolic panels through treatment is to monitor liver and kidney function because chemotherapeutic agents are filtered out of the body by those two avenues. It is not uncommon to see impaired function during treatment, and a normalization over time once it is done.
0