How are people with liver mets doing?
Comments
-
Jjzn, Your numbers don’t sound that bad. I think your liver is still functioning but I am not a doc. I have heard that when ascites is really bad it does have to be drained. So, yours not needing to be drained is a good thing
0 -
BIG ANNOUNCEMENT...........********************** I HAVE RECEPTOR FLIPPED...I AM TRIPLE NEGATIVE NOW
So MO just called. We were both not really too surprised. While I had a lot of tears...they weren't all negative.
1. Now we know why no endocrine therapy was working for me. (this is a relief)
2. This opens me up to not only trials but to Abraxane + Tecentriq and Trodvely
3. My MO is NOT changing the game plan at all.
A. I will go for planning Tuesday Aug 3rd for RADS to T&C spine they are doing both together it will be regular RADS NO SBRT..the T3 area is too small to pack a big punch and my RO is being very careful. We completely agree with his decision. 10 Session just like they did to my sacrum a few months ago and it worked very well he even mentioned that the PET showed it all gone.
B. I will go August 5th for Mapping for Y90 but we are waiting to see when she will do the Y90 (she will probably now want to wait until after RADS to spine are done) MY MO sent an email today to RO & IR about all this to all be on same page.
C. My MO wants to go back to Eriubulin before even pulling out Abraxane. She is also waiting for the PDL1 results which should be in on Monday and then she will send out for the Full Panel TEMPUS...(don't know how much that matters now since I am triple negative???) anyway she also said was not confident with endocrine therapy anyway.
D. Right now they have me on a steroid and ALL MY BITES WENT AWAY!!! They actually started going away as soon as I stopped the Afinitor...this tells me my assumption that my cancer is very active and fueled by inflammation is very true.
MOTH any advice or info you can give me would be greatly appreciated....
Lots of tears..but again...some relief. I know CUREIOUS has mentioned that those that flip to TNBC have been shown to have a better response to TN treatments than those that start out TNBC.
Love you all...
0 -
That is big news indeed Nicole. It must be a relief to better understand what is going on, so you can be strategic. Did they do some sort of surgery to stabilize the collapsed vertebrae? (If I understand it correctly)
0 -
Husband it really is a relief it was very frustrating to have so much continuing hope that endocrine therapy would work only to find out it wasn't. Now we know why.
The radiation should kill the cancer and/or shrink it away from the fracture and then new bone can grow to repair it. My main concern is the side effect Esphogitis > spelling I am praying for minimal to no side effects if you can be one with David and I in this I would be grateful.
0 -
Nicole- TNBC oh my. 😳 Thanks for the update! Looks like that biopsy was very much worth the trouble. I know you are suffering but you have a good plan. I would do y-90 again too because it worked for me. I hope it is still on the table for you. Keep on fighting one day at a time. 🙏🏻 For no side effects on the rads.
Dee
0 -
Hi Nicole, yeah, that explains a lot! Which biopsy was it that is triple neg now? Is it your liver.
The PD-L1 will tell you whether Tecentriq is an option.
Tempus at this point is probably to look for PI3K which would let you go to piqray.
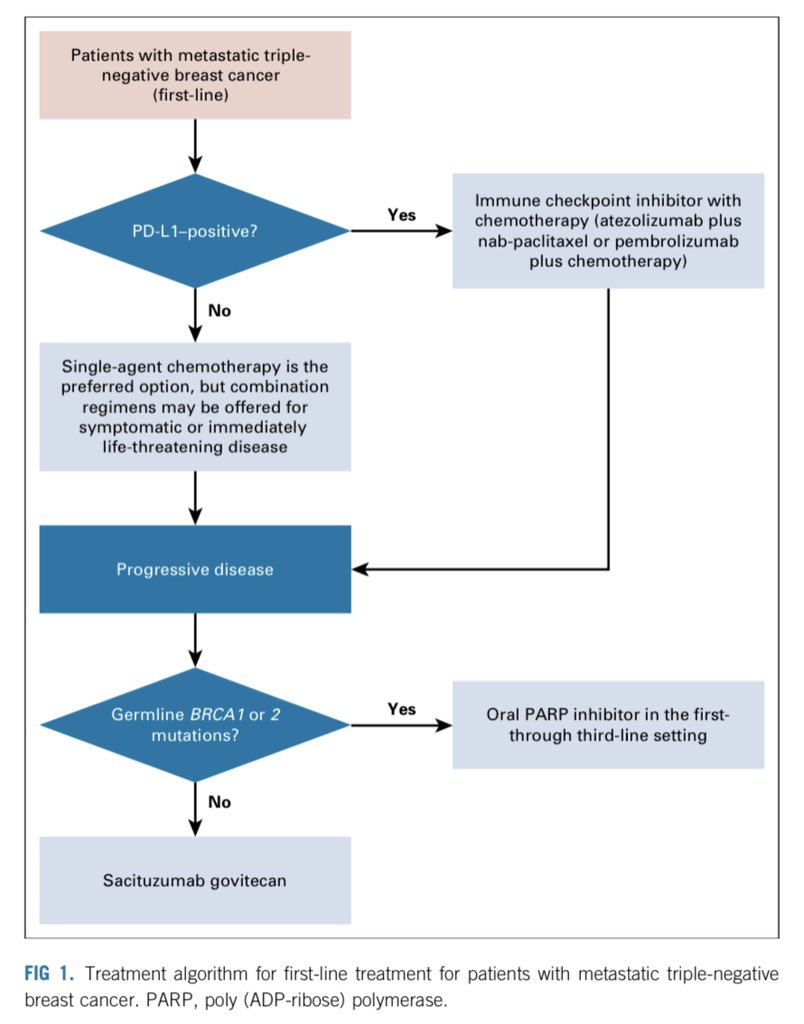
Trodelvy is the next option after Tecentriq. ASCO *just* put out new clinical pathway documents for metastatic breast cancer. This is the TNBC one:
I think things are different in the US but one question I'd have for your MO is about whether she can access tecentriq for you if it's not first line. Here it's approved for ONLY first line so if I had done any chemo after being dx with mTNBC, I wouldn't be able to get Tecentriq.
So I'd clarify that with her because once you have your PD-L1 results and if you test positive, you might want to start Tecentriq+Abraxane right away.
hugs!
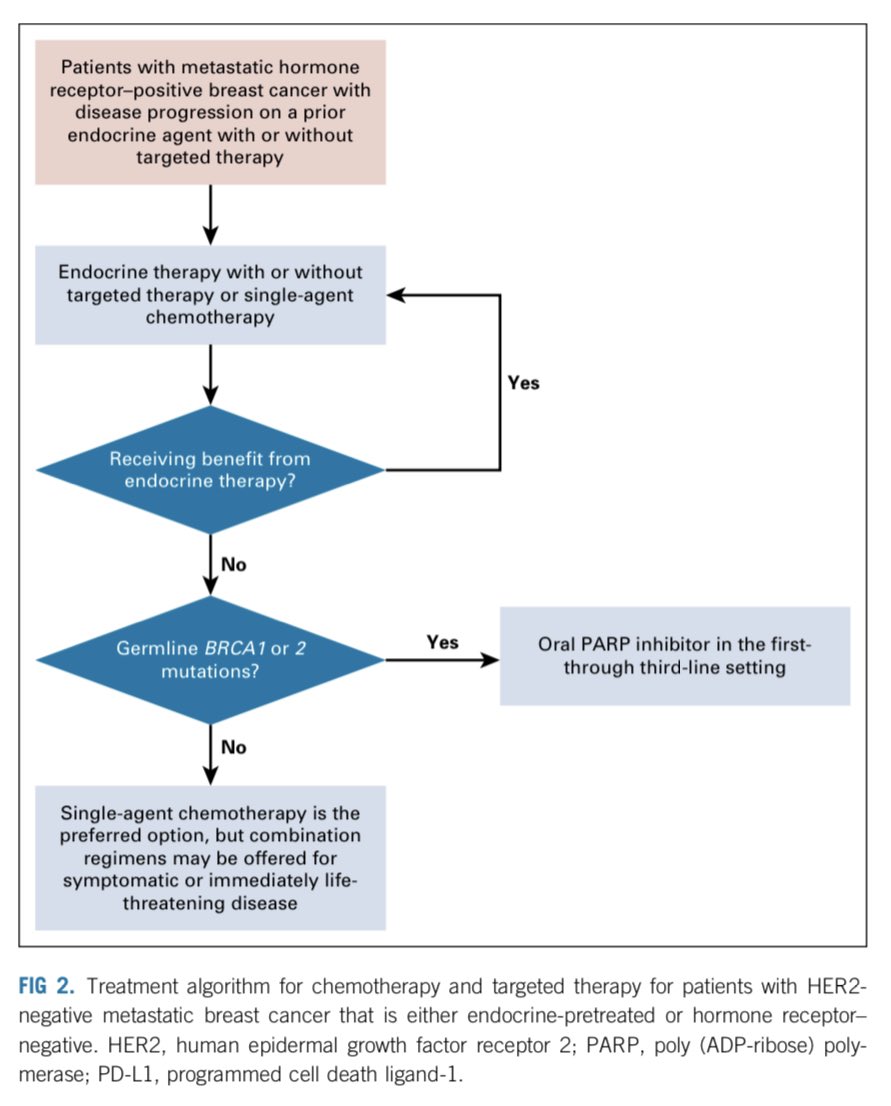
ps. I also have screen shots of the HR+/HER2- algorithms and HR+ which is refractory to endocrine therapy. If anyone wants those, let me know & I'll post.
0 -
Nicole- I know about esophagitis as I just went through it with my recent chest radiation. There are meds you can snd should take to help. I wil ask any questions I can about my experience.
Glad you finally have an explanation and a good plan. Makes s as world of difference.
0 -
Hi Moth,
Not sure if I have this from you but would appreciate the screenshot for refractory to endocrine as that seems to be where I sit now.
0 -
Sadiesservant, here it is - but honestly it's a bit disappointing IMO
Algorithm for endocrine-refractory HR+/HER2- MBC
0 -
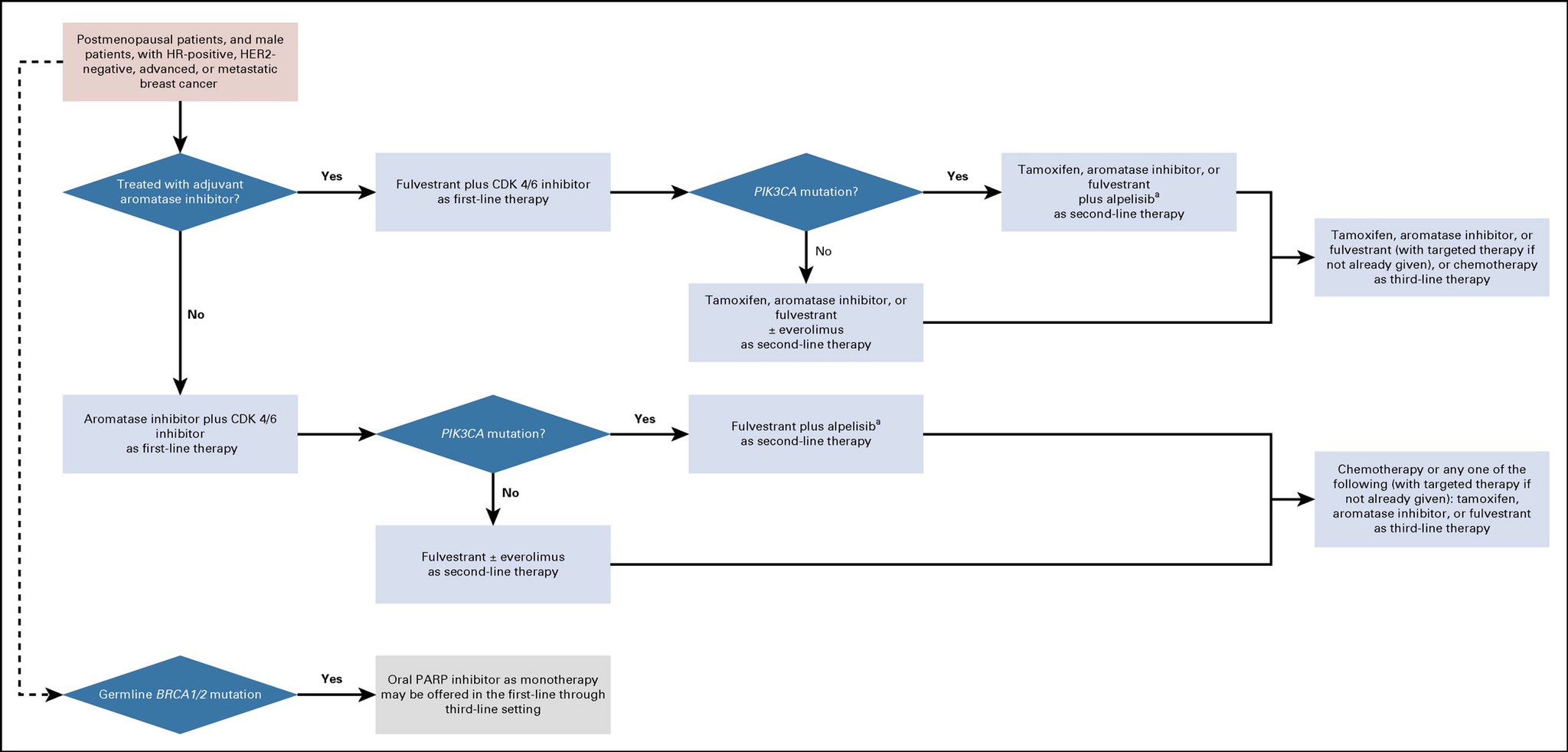
Actually I'm just going to post the HR+/HER2- MBC clinical pathway without being asked. Someone will want it I'm sure

Algorithm for HR+/HER2- MBC
0 -
oh & if any of the images are too small, on a computer right click and open image in new tab and most browsers will then have a zoom option
0 -
Dee I know you looked terrified about me having TNBC...but according to studies..and even CUREIOUS on here its been noted that those that flip to TNBC do much better on TNBC therapy then those who start out TNBC. Either way I actually feel a bit of relief bc I was failing every ER+ drug there is...and I would rather know what I actually have then just want ER+ bc they have more treatments ya know? I mean having more treatment options means nothing if they are all failing me anyway..which they were. The one that I had success on was Halaven..and it targets PDL1 specifically.
Moth Thanks....Yes...it was a liver biopsy and 3 samples from there from 3 new tumors all other tumors are dead in the liver anyway from last Y90...
I am still getting Y90 my mapping is this week.
Moth...I will ask my MO about that stuff about tecentriq...but we did talk about that today and she didn't mention the concern you have but I will ask her anyway in case she doesn't know that. Moth you did see that I already had PDL1 2 years ago 10% so my MO did say chances are very high that I not only still have that...but it may be even higher.
If ya'll think of anything else I should ask...just let me know.
BTW...has anyone heard from HOPE?? I have not and reached out ....still nothing? JFL? anyone?
0 -
Well, Nicole, its a big surprise but at least you know what you are dealing with now! Remember that both Barbara Bigelow and Judy Perkins were also converters, and I remember from Barb's site that her Dana Farber MO told her that all of their top IO responders were in cancers that had flipped from ER-positive to triple-negative. These are not at all like traditional TNBCs, remember they are their own beast, and if they are for some reason more readily accessed by the immune system, you may get better responses from each of the therapies than they see with TNBC proper, because even when you are not on immunotherapy, your immune system can still get better access.
I posted on the Clinical Trials site that they are getting a nice bounce to chemo by adding the CCR5 monoclonal antibody (Leronlimab) to carboplatin for TNBC- that drug is helping the cancer shed the shielding macrophages to give chemo better access the tumor, and should probably boost the checkpoint inhibitors as well. So, that is something for your MO to request at some later point when you think whatever you are on needs a boost, it is already FDA approved and used for years on HIV patients, with very little in the way of SEs. By the time you may want it they should know much more, just keep it on your list, the effects were very impressive. In addition, your MO might consider adding Celebrex when you are on immunotherapy, remember KattySmith responded in a trial that included EP4 inhibitor with immunotherapy- it's just a newer-gen Celebrex, this should help in exposing cancer to the IO..
Then there is also another drug, I forget which one, they were very excited about at San Antonio for TNBC, will go look it up...
0 -
Eganlisib is the promising drug, in the MARIO trials it is used in combination with Atezo and Nab-Paclitaxel. It's well worth looking anew at some of these clinical trials, because they really are upping the combinations.. Mario-3 is for firstline but there will be other good ones out there..
https://www.cancernetwork.com/view/eganelisib-comb...
Patients enrolled on the MARIO-3 trial who had PD-L1–positive tumors had a complete response (CR) rate of 16.7%, a PR rate of 50%, and 28.9% achieved stable disease.
just a few days ago update:
- MARIO-3 TNBC early data suggest the addition of eganelisib to standard of care regimens extends progression free survival regardless of PD-L1 status with majority of patients still on treatment –
- 86.8% of evaluable 1L patients with TNBC in MARIO-3 achieved tumor reduction with a total disease control rate of 84.2% –
And as always, BestBirds guide will be very useful in this area, its complicated!
0 -
Wow Nicole, what a roller coaster! I am happy that you at least know what you are dealing with. Thinking of you and sending big hugs!
0 -
BIG news is right. WOW Sounds almost like a relief to have an explanation that makes sense. Glad you’re going forward with the y90
0 -
I have been away from BCO for a week with a family emergency. I just read all your posts.
BLMike- I am sorry for your loss. Hugs.
Nicole- Wow. I will keep praying for you.
I was to have a consult with RO and liver surgeon on Tuesday to discuss my options. I have fought with my insurance for a consult approval. Finally got it Thursday, so I missed the Tuesday appointment. Rescheduled for mid August. I hope my cancer is still slow growing as time is clicking away and I still do not have a plan in place. Last scan was June 25 with more progression. And cannot talk to consults till mid August to even decide on a plan.
0 -
Thank you so much Cure! I sent that trial to MO last night...CCR5 monoclonal antibody..... we will see what she says....
0 -
Flipping tumor status, ER+ to something else . Do the DRs monitor the status and how often? If AIs don't seem to work, is that a reason to retest? I've been biopsied 4 times, 3 times with original/new tumor and once to verify if a rash and worsening swelling was metastasis or something else. Unfortunately it was metastatis.
0 -
Blue girl...I never wanted to waste time (to me it was a waste of time) biopsying an original tumor...I always felt we should do a new one...and that is what we did here...she got (I believe a FEW) samples all from new tumors (the rest of my tumors were dead tissue anyway)...they all showed ER- PR- HER2-...my old ones were biopsied 2 times..and both were ER+ PR- HER2-.....I definitely had a BIG feeling I had receptor flipped and I am kind of glad now that I have. Would I rather be ER+ just bc they "have more treatments" but none of those were working anyway? Or flip and maybe get something that can work for a while? For me the answer is clear. Apparently I am not the only one that was ER+ HER2- and treatments didn't work well at all..there are MANY out there and some of them don't flip so they just run out..
 .
. PS: CUREIOUS..thank you for your encouraging words! You took a kind of freightening situation and made me see the glass really can be 1/2 full....
0 -
Can you all tell me how the risk for Ascites comes?? Is it from Y90?? What are the symptoms and what brought it on? It seems even though JFL's liver numbers were going almost normal her Ascites was the problem...or at least thats what I got out of the last post by her. I am very concerned about this for a 2nd Y90....
Husband didn't you say your wife got Ascites from too much die off from Xeloda? So that is my fear with too much die off from Y90..we are only targeting 2 small tumors all under 2cm..... Did your wife have a bunch?
0 -
Nicole, my wife at time of initial diagnosis with stage 4 liver mets was that she had extensive diffuse mets in one area, and several discrete tutors in another area. Something happened during early treatment with xeloda that caused hepatic hypertension and ascites. The hypertension is caused by a blockage of blood flow through the liver. What was the cause we will never know. The hypertension led to the ascites and numerous other damage, like an enlarged spleen and varices in many veins. Eventually, the ascites went away. It was very extreme at first. Close to a gallon of fluid drained per week. The damage to her veins and spleen remains. One theory is that killing off too many cancer cells quickly led to some sort of clotting or blockage. But we will never know. Nor can i say if it was one tumor, multiple, or the diffuse mets. It has left her liver wth pseudo cirrhosis. A look that mimics cirrhosis
0 -
Thanks Husband. ..... So I guess there is really no way to know if that can happen....
 . I was going to try to decided if maybe I should wait on the Y90....0
. I was going to try to decided if maybe I should wait on the Y90....0 -
We were told, and this seems supported by the lack of published case reports, that it is extremely rare. I would not avoid treatment in fear of it
0 -
Moth - thanks for posting the clinical pathway graphs, very interesting.
NicoleRod - that certainly is big news, flipped receptor status appears to be happen more than I ever thought it would. I am learning so much from this group.
0 -
Interesting development with what's going on with me... So I've been off tamoxifen for almost 2 weeks to see if that's what's causing the upper GI issues , rise in AST ect ( Since the CT did not show anything concerning). I get a call on Saturday about a frozen mango recall tainted with Hep A. Normally I would never pay any mind to a recall that spans 9 months BUT, I eat that frozen mango like candy every day and have for the last year ( No exaggeration here.. everyday). So I've had to ask my GP to test me for it to either rule in or out. I would hate to give up a treatment on the basis of mango *face palm*
0 -
B-A-P- have you been vaccinated for Hep A- most of us have been- hope all ok
0 -
NKB,
Never got the Twinrix vaccine. Not sure why exactly. Usually they give it to you if you travel anywhere tropical and I haven’t since I was like 12 give or take. I’m also a non converter (I think that’s the term) to HeP B. I’ve been given the 3 shots on time , twice , and my immunity always goes back down to nothing.
Good news is Hep A isnt chronic but would explain my current symptoms. If it’s not Hep A then I’m still at a loss of what’s causing my issues because taking a break from tamoxifen doesn’t seem to be helping much.
0 -
Hi everyone!
It has been a while since I have been posting on BC.org and I am in a bit of a funky place and wanting to check in and all the stories and how people are doing and get caught back up with old friends and with new ones. You all were such an amazing support and resource for me during my first couple years with MBC and then I moved away from BC.org to do some volunteer work with Living Beyond Breast Cancer's organization and also cancerland is happening and Covid19 and life just got crazy!
Anyway - here today on this thread because I have a weird story to share and wondering if anyone can relate and what have you done and how have you been etc etc?
Last year in August 2020, my (now old) MO discovered liver mets through a ct scan and then followed up with liver MRI. Switched oncos and went to new MO who wanted to do liver biopsy. When they went in for the biopsy, the IR doc couldn't find any lesions to biopsy despite the MRI and Cat scan findings. Then a petscan follow up showed no actively metabolic liver mets, just hypodense lesions not doing much. That was all in like February 2021?
Cut to then my right breast where primary tumor had been and shrunk from Ibrance and letrozole treatments and suddenly a tumor was growing with a vengeance. Got that removed with unilateral mastectomy in end of March 2021.
Next my labs started to get kooky and my hemoglobin and RBCs started to drop, then followed by my WBCs. Had a lumbar puncture, and three bone marrow biopsies that produced no aspirate (bone marrow fluid) to look at and have pathologized, but they could see that the cancer in bones is still ER+/PR+/Her2- as I have ever been. Same with breast tumor which had Ki67 of 75% (crazy high! eek!).
Then two weeks ago I discovered little weird lumps around mastectomy scar which during port placement last monday, were biopsied and came back positive for BC skin mets.
Next up, started chemo last week, had petscan on Thursday and it showed that I had a moderate pleural effusion and the liver mets are incredibly active and pushing on my liver capsule now. Today I had a pleural effusion to remove the build up of fluid in my bottom right lung lobe which is probably being pushed around by the liver lesions causing inflammation in the liver capsule covering and pushing upward on lungs?
Anyway - going to stay the course on the chemo Gemzar for right now. It is my first chemo experience. I had it on Wednesday and by Friday I was down for the count for the day. So much so and then with petscan showing the liver lesions and pleural effusion I am now completely whacked out on Decadron.
I am awaiting my lung to "unfurl" from the tissues being pushed up against and hopefully breathing will be so much easier and less painful.
Anyone connect with my journey? Any words of wisdom and hope? I am feeling like there is the "dark side" of me that is like, "Okay this is it, I am dying soon." And then this other part of me that is like, "No! So many of us have been through even more challenging experiences with MBC. This is not even close to the end."
I definitely want this to be the only and last pleural effusion. It was not my favorite experience on earth!
Thank you all so much for taking the time to read if you have gotten this far.
Much love to all,
Philly aka Brenda
0 -
Phily aka Brenda, I was in a similar situation this time last year when faslodex and ibrance failed for me. My cancer load spread from lung and lymph to bone, liver and skin. Xeloda was next, but did not work for me. I had some radio therapy on the bone in my back , then more on my skin. I ended up in hospital with very low oxygen levels because of a pleural effusion. The chest drain collected almost a litre of fluid. [ I did not think I would be alive by Christmas] Eventually I started on a course of Taxol , then changed to Abraxane after an allergic reaction. I have been on this drug regime for 8 months now. My scan last week showed my tumours were slowly shrinking and I had no new eruptions. [ I was so pleased ,I would have been happy with stable] My oncologist and I have decided to drop the frequency of treatment from 3 weeks on and 1 week off, to 1on 1 off because of the cumulative side effects of fatigue and neuropathy. I want to keep going for as long as possible and quality of life matters.
I hope you soon find the treatment that works for you and this is just a nasty blip that is not repeated.
0