Will 30% of Early Stage (1-IIIA) go on to metastasize??
Comments
-
Barbe, all good comments. It boggles the mind that some women even seem to think a mammogram keepsthem from getting bc.
0 -
I know, eh!?!?!?!?!? They hear "Mammograms prevent late stage breast cancer" or some stupid line like that and think just getting them means they'll never get breast cancer!
0 -
That the "Komen syndrome" and pink-washing of all women. "Get a mammogram and you will save your life" Ummm, nope, not if you are Stage IV de-novo or eventually go on to mets. Even with DCIS, my "odds" are still higher that I will get another BC diagnosis. Better than someone of a higher stage and I am grateful, but sure as hell not out of the woods as is NOBODY! Not anyone with breasts. (men included) You either will get BC or you won't get it. Period.
Edited to add that I still believe in mammograms. Just don't believe that they save all that many lives to be honest.
0 -
Another terrific book, The Microbe Hunters, speaks to the surprising ways that discoveries are made. In print for close to 100 years, it is a medical "classic."
Dragon, science discovery is very, very messy. And yet, researchers continue to toil in their labs, trying to make sense out of the messy, but elegant cell. What makes the current research so incredible, is that those discoveries are happening more quickly.The folks running The Rare Breast Cancer Lab at Sloane Kettering have told me that great discoveries are astounding them every few months rather than every few years. Just want to add that those researchers are the ones who have found blood markers in Stage IV patients that track progression sooner than imaging. One may ask, why woukd a Rare Breast Cancer Lab be studying Stage IV patients' cells? The answer is that a Stage IV out of the gate is very rare. It afflicts 15% of breast cancer patients. One of the biggest controversies in population based screening mammography is that despite screening, the number of Stage IV diagnoses from onset has not diminished. We NEED to do better.
0 -
I have my mammogram next week, and am five years out from Stage 1 IDC. Every year, my anxiety ramps up like nobody's business, and I come here for comfort. You all give me so much of that!
I just posted something I thought I would share. I worked in Republic of Georgia, where there is little, if any screening for breast (or any other) cancer. I once asked my doctor what the old mammogram machine in the hallway was doing, and she replied, "being sold to a third-world country"! So even if they do get screened, the technology is very far behind.
The statistics there are staggering: most women are diagnosed at Stage IV. Most women here, at Stage 1. Their conclusion was screening accounts for this, at least in large measure. I was an anti-mammogram "they don't save lives" type, cynical about my own improper diagnosis until I found this out. And I have been humbled.
They may be better than we think.
0 -
LtotheK, yes, as much as we can grumble about liitle things like gas prices, being stuck in traffic, bad service at a restaurant, ect.....and get angered about big things like having breast cancer, I still am aware that living in the U.S. affords me access to some pretty good health care. These past several years, for some reason, I'm quite aware of certain good fortunes I've had by living here, by my grandparents immigrating to the states in the early 1900s
0 -
Lto...population based screening mamography does work well here in the US for those btween the ages of 50-75. Unfortunately for other US populations, it doesn't work as well. Perhaps there will come a day that a less expensive way of screening patients, via blood markers, will be available. That way, feaer women will require expensive mammograms. You are right with respect to developing countries, we need to not onky do better here, but all over the world.
0 -
LtotheK, thank you for pointing out that cancer care is different in other countries. I'm also quite familiar how things are done in post-Soviet countries. Women are not screened for cancer. If the lump is found, you get a mastectomy or lumpectomy. One round of chemo is about $3000-4000, and you pay for it by yourself, if you have means. Very few can afford the full course of treatment, hence no chemo. I think radiation equipment is only in the major cities, and it's outdated anyways, so no rads either. They are instances when you can go abroad for treatment at your own expense, but often you cannot afford the treatment and lodging for the extensive stay, so you bring drugs home, and have to pay nurses for administering them. You have to bribe the nurses in order for them to open the vial in front of you and you witness them administering your drug to you, otherwise it will be switched and sold on the black market. So, if you go through a surgery only, you just wait and see how it turns out for you. I suspect that poorly educated women without internet access are not as emotional about it as the ones that have the same access to info as we are. Thus, they got less treatment and, probably, experience about the same level of anxiety as we do after chemo and rads. I would say that, emotionally, the waiting game is comparable, only we get it after a barbaric treatment., and they- after the surgery only. It would be nice to see the statistics of progression to stage IV and recurrences, but these data are unavailable. I also have to say that attitudes in the medical community change, and they are attempting to treat according to US protocols (without means to do it). If I continued living there, my cancer would hot have been found, and I had a chance to live a happy life for a little longer. My whole outlook on life changed after my diagnosis, I will never be the same. I have no hope to return to the full and productive life I had before that routine mammogram.
0 -
I posted this article comparing incidence and treatment in Ghana. We have faults with our system of care in the US but it's better than many. Thread
0 -
Hi BosumBlues:
My understanding is that for all patients, the risk initially peaks in the early years, declines, and then persists at a low level. In ER+ patients, the risk does not decline quite as much as it does in ER- patients, placing ER+ at somewhat higher risk for late recurrence. See for example:
Colleoni (2016): "Annual Hazard Rates of Recurrence for Breast Cancer During 24 Years of Follow-Up: Results From the International Breast Cancer Study Group Trials I to V": http://jco.ascopubs.org/content/34/9/927
Note: A complete pdf copy of the article can currently be obtained for $2.00 via the PatientACCESS option (requires registration with the Copyright Clearance Center).
This study was done in a diverse patient population with invasive disease (ER+, ER-, node-negative and node-positive, pre- and post-menopausal, a range of tumor sizes, etc), with a long follow-up period and found: "For the entire group, the annualized hazard of recurrence was highest during the first 5 years (10.4%), with a peak between years 1 and 2 (15.2%)." The initial peak is illustrated in the first graph below.
After that, the risk in ER+ disease (yellow) declined up to a point, but not as much as seen in ER- disease (blue): "We have demonstrated that the hazards of recurrence and death decreased consistently until year 10 but then remained stable after year 10 through year 25. We have also shown that patients with ER-positive tumors continued to have a higher risk of relapse, including distant metastases, during years 5 to 25 . . ."
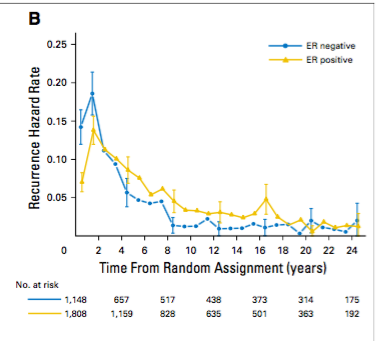
"As shown in the Kaplan-Meier curves (Fig 3) as well, the curves of ER-positive and ER-negative cohorts cross, and the hazard ratio of ER-positive versus ER-negative disease changes over time for BCFI, DFS, and OS (P , .001 for interactions of ER status and survival time)."
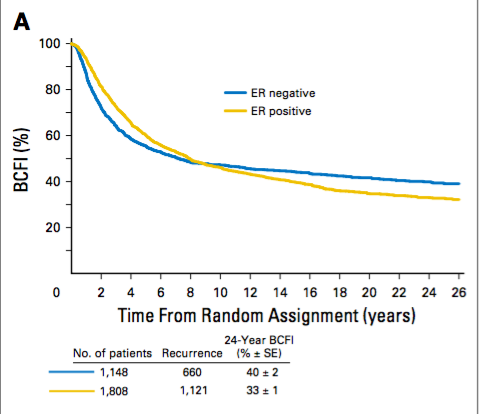
"BCFI was defined as time from the date of random assignment to any invasive breast cancer recurrence (including ipsilateral or contralateral breast recurrence) and was censored at date of last follow-up or at date of death without recurrence."
BarredOwl
0 -
BarredOwl - Did I miss it? What is BCFI?
0 -
Hi Warrior_Woman:
I did include an explanation of BCFI under the chart (last three lines). However, I should have added that the abbreviation BCFI stands for "breast cancer-free interval" and was the primary endpoint of the analysis.
BarredOwl
1 -
The number-crunchers at the CDC concluded that before age 50 and after age 55, annual mammograms “don’t save lives.” But the metric they used was overall survival, or rates of death from all causes--neither DFS, BCFI, nor death from metastases. By the time you get to 84 (I think the average life expectancy for women in the US & Canada), having had a mammogram decades earlier at an early stage will have had no bearing on whether you’re still alive. Oh, it would affect whether you have NED or are experiencing a poorer QOL from mets symptoms--but you could also (and are as likely as not to) die from an unrelated cancer, heart attack, stroke, COPD, CHF, complications of diabetes, dementia, or a rapid decline after a poorly-or-non-healed broken hip. Statistics are numbers. “Lives saved” does not take into account the quality or longevity of those lives.
It all boils down to what your gut tells you makes you feel more secure. Even if an “early catch” doesn’t always prevent mets, catching those mets early makes them more manageable for a longer time, perhaps changing cancer from something you die from into something you live with until your number is up from whatever cause.
0 -
ChiSandy - The other issues those OS stats ignore, of course, include finding cancer at an earlier stage, perhaps before it has spread to nodes for example, and potentially minimizing both extent and expense of treatment, thus decreasing morbidity, and increasing QOL for batients and their families alike, even without metastases.0
-
I honestly think custom targeted chemo and therapies (i.e. they take just YOUR tumors exact DNA and use it to create an individual chemo) is just a few years away...
I'm doing the Kailos genetic testing and read a study from Boston College saying that Pharmcogenetics is the wave of the future - just knowing your own pathways and how you metabolize on each pathway is so helpful in making personalized dosage decisions.
Immunotherapies are exciting - which is another reason I hope the mammaprint doesn't come back high. You know even if it does, I may forego Chemo and wait til the cancer shows back up in a decade or whatever to do chemo... I'll definitely take the Tamox - but if I'm a poor metabolizer (ie. Kailos).. it may influence me doing ovary suppression... In any case, my cousin who had my type of cancer 10 years ago (but a 1B) had never heard of ANY of these type of individual tests or options. She just did the BMX, Chemo and AI for 5 years... and she's fine now.. so far.0 -
Hello friends,
This is where my brain power reaches its limit : ) Had I not been screened, or pushed for my own screening six years ago, it is likely that by now, my Stage 1 grade 3 IDC would have been much bigger, and perhaps viral. And my understanding is, Stage IV is not the livable disease they'd have us believe these days. The statistics are the vast majority gone by year 5 post met diagnosis. Please correct me if I'm wrong, but at age 39, a Stage IV tumor would have left me with less than a decade unless I was in a tiny minority. A Stage 1 means possibly decades more. By the CDC's evaluation, it sounds like screening doesn't affect survival at all? Help an addled girl.
Also, yes--immunotherapies are rather amazing. My great friend has bone and lung cancer, and she's been on them for a year after her chemo stopped working. I don't think we are talking decades of life, but probably a couple more years, which is amazing. They are not child's play--they make her very sick, tired, and she takes speed to keep her energy going.
0 -
Also, yes--immunotherapies are rather amazing. My great friend has bone and lung cancer, and she's been on them for a year after her chemo stopped working. I don't think we are talking decades of life, but probably a couple more years, which is amazing. They are not child's play--they make her very sick, tired, and she takes speed to keep her energy going.
0 -
I have a question though. So the graph posted by BarredOwl is showing risks of recurrence (of the same tumor), right? If I have a new primary, does that mean I now have TWO "clocks" counting down, each one indicative of one tumor?
0 -
treelilac - I was recently diagnosed with a recurrence (TN) that is different than my original dx four years ago (ER/PR+, Her2-). My MO says I have two clocks running for distant recurrence, with each cancer having a distinctly different recurrence timeframe.0
-
Hi TreeLilac:
I don't know the answer to your question. In the second graph above, where BCFI was measured, they counted any invasive breast cancer recurrence, including ipsilateral or contralateral breast recurrence. The latter (contralateral) are considered new primaries in most cases. Thus, they counted the first additional diagnosis of any invasive disease and did not distinguish between new primary or truly recurrent disease (and it is not always clear). They didn't measure anything else, so the graph is a "clock" for (or up to) first recurrence only, and in my mind, does not speak to the possibility of a continued risk posed by the first cancer after recurrence.
One could speculate that a truly new and independent primary would behave in the same manner as an original primary and follow the patterns illustrated in the graphs above for an original primary (starting a new "clock" that runs according to the established patterns). But whether some continued risk for a second recurrence remains from the original cancer was not determined.
In contrast, an actual recurrence (the same tumor coming back despite treatment, sometimes slightly altered) might or might not behave the same way as an original primary with respect to time to recurrence. In another thread, Kbeee has mentioned the limited studies available regarding recurrent disease.
BarredOwl
0 -
You are absolutely at higher risk. A lot of women who get BMX, find out their 'healthy' breast actually was DCIS or even had a hidden IDC. I think insurance covers prophalatic MX on the other breast at any time when you've had cancer.
0 -
I asked the same question of my MO, as I am scheduled for a unilateral mx next week. He said I'm at no higher risk for contralateral recurrence with IDC, and did not recommend a bilateral mx. I understand ILC is often found contralaterally so I might have been more worried had that been my dx.0 -
L.....what the statistics tell us is that for women aged 50-75, population based screening mammography (every TWO years) saves many more lives than they do for all other age catagories. That said, whatever age, DIAGNOSTIC mammograms also save many more lives. What that means is, no matter what age you are, younger than 50 or older than 75 and every age inbetween, if you feel something and you have it checked out, you are more likely to have your life saved with THAT mammogram. AND, when you are between 50-75...that population based mammogram, that is, the one that you are invited to have and you DON'T feel anything, is more likely to pick up a tumor BEFORE you become symptomatic.
One of the big differences, also, with respect to population based cancer screening, is that with certain types of screening, like for colon screening, when you remove a non-cancerous leision, such as a polyp, you are removing the CHANCES of that lesion becoming cancerous. With breast cancer it is not the same. You can have a "clean" population based screening mammogram at age 50 and 6 months later, feel a mass, and have an invasive breast cancer.
Hope that better explains the controversy....
0 -
True--colonoscopies not just discover but remove polyps before they have a chance to become malignant--but if (analogizing the two screening tools) every currently-benign anomaly found by screening mammogram is not just followed up by diagnostic imaging but is routinely excised (and the process repeated annually or biennially), women would be subjected to much riskier invasive procedures, pain & discomfort and expense with depressing regularity. Imagine every woman--lump or not, innocuous or suspicious non-palpable density--being subjected to the equivalent of a lumpectomy every year or two.
But the OS stats include “mortality from all causes” so aren’t very meaningful, nor do they describe the quality or subsequent length of “lives saved.” Current standards of biopsying only suspicious growths and removing only the malignant or definitely pre-malignant ones, based on annual or biennial screening mammos (I’m not counting the "go-straight-to-diagnostic-imaging” women who feel lumps or notice anomalies clearly visible to the naked eye and then appropriately seek medical help) are about as prudent as they should be--until such time (if ever) there exists a clear, reliable, economical and completely non-invasive (no more invasive than a virtual colonoscopy) way of detecting breast cancer or pre-malignant changes.
0 -
That is helpful, Voracious and Sandy, much appreciated!
0 -
My "healthy" breast had DCIS with IDC in the middle...
0 -
I got rid of the right one for peace of mind, and for symmetry. It was large, sagging and it helped that I hated the look of them. Now a great ps has made me smaller and I'm no longer sagging down to my belly.
0 -
I had my prophylactic mastectomy on my right side for symmetry but also because only the breast tissue was removed by the PS. There was no need to remove Lymph nodes because there was no cancer to spread there. I was able to have reconstruction on both sides at the same time. I have no regrets about my decisions
0 -
My "good" breast has some LCIS. MRI did indicate there was something there that my BS was concerned about. Said it would have to be biopsied every year (along with 2 other spots that ended up just being cysts). That's why I got that one removed too.
0 -
I chose BMX because I had bilateral disease. My surgeon did indicate he thought BMX was probably being overused but since I had DCIS in the right and in his words, my breasts were good at making cancer, I went for BMX. Good thing I did, we all agreed, because I actually had small and slow-growing IDC in the right. I also didn't have large breasts and frankly I didn't think breast conserving surgery would give me a result I could deal with. And again, that would only have been an option for my right side and based on surgical pathology they'd have had to remove it anyway.
So for me it worked out, to the extent you can say that about having your breasts removed!
0