Any Early 40s Declining Tamoxifen?
Comments
-
Am struggling, phys & mentally lately, so am not really able to put all of what I'd like to say to everyone on "paper" right now, but wanted to send good thoughts to you all, to thank you for sharing, and to cross my fingers for everyone as we make our choices going forward. I agree BT39, this decision seems more difficult than the surgery/chemo ones. Uggh. Le Sigh.
I had a scary thought the other day -- I already live with constant, chronic, severe pain in my bones, joints, spine, nectk. How the heck am I supposed to tell the difference between my "normal" pain and symptoms of pain due to a recurrence occuring in my bones/joints? Makes me want to push even harder for a bone scan or pet scan before I start anything. IDK.
Soooooo many unknowns and variables. Feel like I'm just gonna be shooting in the dark and "hoping" I notice something early enough if worst case scenario the cancer returns or shows up somewhere new.
Guess I rambled even though I didn't plan on saying much. LOL.
Anyway, let's all keep us posted on what we decide. There's no "right" answer, just the one that's best for us. Healing and hugs to all.
0 -
Hi Sharla
My understanding is that Zoloft is a moderate inhibitor of Tamoxifen and they normally switch you to another antidepressant. I am on zoloft currently for OCD, but I will switch to one of the 3 antidepressants that do not interfere with Tamoxifen once I start the hormone therapy after radiation. A discussion on this with your MO would be best.
0 -
Spoonie - will do, definitely will keep you posted. So far, I'm on the side of trying tamoxifen but waiting until 1-2 months after radiation (or my latest 'pull eggs' surgery, whichever comes later - the second one was supposed to happen Friday and didn't because the egg dropped, so... one more round). The reason I'm leaning towards waiting is to allow my body to fully recover AND because a couple people who have been doing pretty well on tamoxifen - aka little to no side effects - both waited around 2-3 months before they started it. So maybe there's something to that!
0 -
I really like that idea, Pebbles. Sure makes sense to me!
Was/is your MO on board with waiting?
My MO has been ok so far with waiting but I worry about the how long is "safe" to wait, know what I mean?
I see her mid Dec so I'm definitely going to hold on it until then. Plus, I'm still not feeling "settled" and "myself" on the new Pristiq they switched me too, since I'd been on Cymbalta before. It's been nearly 5 weeks and am still struggling, so don't want to add a new drug into the mix yet until I know that issue is settled.
Wishing you the best on your next egg round-up! I think you and your hubby are smart to take these steps now vs have regret later.
0 -
Far warning....this is gonna be a rant of some sort. Ugggh.
Soooo, saw my Psych yesterday. This Pristiq change over in order to take Tamoxifen is a beeeotch. It's been awful since day one.
Going on 5 weeks of this new rx and still not much better. Even with her doubling my dose from 50mg to 100mg 3 weeks ago. Was supposed to be a smooth transition from Cym to Pris but that is not what they've delivered at all.
I miss my Cymbalta and feeling like myself...so very very very much.
Psych insisted I tough it out for another month on Pristiq and see if anything changes/improves. So looks like it's going to be a lovely freakin Christmas. Le Sigh.
I feel so much aggression out of no where, for no reason, plus suicidal thoughts (FYI I am not suicidal AT ALL nor was I prior to this dang switch!), thoughts of putting my puppers to sleep (out of nowhere and scary and led to me crying for about 3 hours after that happened), and depression/anxiety is just unchecked.
I've tried to explain to both my Psych and Counselor that this is not me and I feel alien but they all keep telling me to use these "distress skills" and work through it.
It pisses me off since I didn't need any of these "distress skills" prior to them switching my med so I can "maybe" take this dang Tamoxifen. Ugggh. I rarely needed my Clonazapam prior and now I feel like I need it daily just to survive.
Sorry, am just feeling really beat down about this and want to feel like myself again, the myself on Cymbalta with IBC was miles an miles better than myself on Pristiq. This med is just hellish for me.
I can't imagine what adding Tamoxifen to this mix at the beginning would have been like! Thank goodness I insisted on only starting one drug at a time!
0 -
Spoonie - so sorry you are feeling this! What is helpful for you to feel uplifted? Do NOT put those lovely and supportive puppies to sleep, do NOT harm yourself, you have an entire network of supporters here and I hope you know it. Let us know what we can do to help you through this. If listening to music, getting outdoors, petting your adorable fur-babies, or something usually helps you feel uplifted, please do that.
Some thoughts - go for a second opinion? Clearly this new change to Pristiq is having major side effects. What's the reason why you couldn't take Cymbalta with Tamoxifen?
I know this seems to be an out there suggestion from someone who is planning on taking Tamoxifen, but for you I might consider the option to not take Tamoxifen. It's just a risk/benefit analysis you have to do for yourself. Keep in mind there are lots and lots of stories out there from people who have beat cancer naturally, without tamoxifen or chemo or anything else. Suzanne Somers did the surgery and radiation like us but she declined chemo and she declined tamoxifen. I've been reading and learning a lot from ChrisBeatCancer.com and FoodForBreastCancer.com and I do believe that nutrition can go a really long way towards curing and/or preventing cancer.
For me, part of the reason I'm OK with giving Tamoxifen a go is because I've been skating through radiation with little to no side effects, and I was pretty good after surgery too, bouncing back quicker than most, and I am not on any other medication, so I'm hoping I can be one of those who takes tamoxifen and has little to no side effects. I'm still really, really worried about it, and honestly if the side effects are too much to bear, I will probably stop taking it and just bank on the healthy nutrition and lifestyle to prevent the breast cancer from coming back. But I'll give it a try, also because it's the reason the docs did not pressure me into chemo, so I'll try it.
But, while you and I have been similar in that we do a LOT of research and we really go to these boards for support, our experiences have been different - like you said, you get the side effects, it's happened, so you have reason to be super weary. I would said it may not be worth taking something that is giving you depression and suicidal thoughts just so you can take Tamoxifen. Go back to what you're comfortable with and know works for you, find out if you can really take it alongside Tamoxifen or maybe there's another option too, and consider the path of natural healing as an alternative too. Just know you have options and do what's best for you. Maybe have a look at the women in the alternative boards to see what worked for them? You already did the surgery and radiation so those are the most curative things... the tamoxifen is just another tool to help keep it from coming back. But maybe you can keep it from coming back with pure, good nutrition and lifestyle updates.
Just realized I forgot to answer your question re: whether my MO was on board with waiting... I don't know. I have an appointment with him in December after I'm done with the radiation so we will find out. I'll keep you posted. And thank you for the well wishes on the next egg round up! Right now we are just waiting for the next cycle - the 'pulling eggs' surgery we thought would happen over Thanksgiving weekend didn't happen because there was one egg growing faster than the others that ovulated even though you take all the stims to try to keep that from happening. But the body does what it does, so we'll give it a go with one more cycle, and if that doesn't take, at least we had a good first cycle and got 2 little embryos from that one!
0 -
Thank you Pebbles.
These thoughts are so random and have no precursor, at all. I know it's this drug. It's awful.
I can't take Cymbalta with Tamoxifen since it's one of the anti-depressants that completely blocks Tamoxifen from turning into its active form. So short story, if I take Cymbalta I won't get the benefits from Tamoxifen and yet all of the SEs. It'd be like taking a placebo that messes with my entire system. Ugggh.
My pysch won't change anything until after one more month but trust me if things don't improve or these thoughts increase then I am off it and back on my Cymbalta. You're completely right that stressing about about Tamoxifen is not worth hurting myself or my furbabies whom I love to pieces.
I just hate that no one will listen to me and take me seriously. I am forbidden from getting a referral to see someone else unless my current provider allows it and she has already said no because other therapists would suggest the same. It sucks.
So, I just have to push through it and/or decide when enough is enough. Thankfully, 95% of the time I'm just sad/zoned out/or fighting my anxiety. Not fun but at least not dealing with the scary thoughts and aggression that just pop out of nowhere.
0 -
Hi Spoonie, I’m just butting in here because I am really upset that you are forbidden to seek a second opinion. Why is your current psych so sure that every other doctor would say the same thing? Isn’t the whole purpose of a second opinion that someone else’s opinion might be different? I don’t know your circumstances, but if you could afford a one-time consultation with one or more doctors or counselors outside of your insurances group, you wouldn’t need “permission”. Maybe there is a low fee clinic or sliding-scale clinic nearby or one that is connected to a university or an institute such as the Jung Institute which has a sliding-scale fee clinic. Many psychiatrists, psychologists and MSWs use forms of treatment that are not based on medications but are based on listening and discussion and analysis and the patient is not ordered around but comes to a new understanding of their problems....Just my 2 cents....maybe it is the antidepressant medication you might consider dumping.
 0
0 -
In my area (NYC) there are also excellent Nurse Practitioner Psychiatrists who can prescribe. They are cheaper to see without insurance than psychiatrists - like about half the price. I was doing that for a while while I didn't have insurance, and then when I was having difficulty finding an in network psychiatrist.
0 -
Hi Sara - thanks for "butting in", lol, I appreciate it. I know my Psychs' statement doesn't make sense at all. I've asked and the only way I can seek another opinion is to go to another clinic system completely, otherwise I am not allowed to schedule with anyone different.
Right now, if I knew I would be battling this whole BS for months, I would do so, but as I see my MO on Dec 15, I'm going to ride it out as best I can. I just don't have the physical energy to expend on it right now.
If my MO can't find a way for me to take Tamoxifen on a different anti-depressant (other than Pristiq or Effexor) so I can be mentally healthy or am not able to recieve Tamoxifen gel for topical application, then I'm pretty sure I will be telling her that I'm not willing to sacrafice my mental health to "maybe" prevent a recurrence or another cancer. I just can't. It's too much....
So, for now I bide my time and manage the "alien" living within me .
Thanks ladies for the support. It's tough going. Seems like IRL I'm all alone now that RADs is over. No one seems to care nor ask what is going on or how I'm managing these days. Le Sigh. Oh well, since I've been a Spoonie all my life, I was prepared for this to happen and am not surprised.
Hugs and healing to all --- may the weekend be kind!
 0
0 -
Spoonie - I agree with you in your case, mental health first. Lots and lots and lots of other ways to prevent a recurrence.
I discovered this lady's story through lots of searches I was doing on breast cancer, and she healed her breast cancer naturally: http://theresadinallo.com/about-coach/
Those stories exist! Now for me, I'm OK with the surgery, radiation and tamoxifen, and I'm ADDING the healthy eating nutrition and exercise to that, which I think can also help me hopefully take tamoxifen with little to no side effects (I'll keep you posted)... but finding the stories where people have beat this naturally with just the diet and lifestyle changes is so encouraging to me, so I like learning from those too.
Hugs and healing and furry paw cuddles to you too!
0 -
Thanks Pebbles...am so struggling. Had a mental breakdown in the car today.
THis Pristiq is a nightmare for me. Maybe it works wonders for others but for me it is toxic or so it feels. I don't want to be on it anymore. I am counting down the days till I see my MO on 12/15 where I plan to tell her unless her and my Psych can find a drug that ensures I'm safe mentally for myself and others, then I can't do this anymore and can't take Tamoxifen. I'm scared of myself, not all the time, but during those 2 mins where for no reason I snap and just want to die or hurt myself or someone else...for no FLIPPIN reason at all. It's all the drug. This was not me just 7 weeks ago when I was happy and stable on Cymbalta.



----------------
Forgive me if anyone read this on the Nov Radiation thread, but this is how it's been for me lately, if anyone wants to know:
Feeling super depressed.....Breast Lymphadema and Radiation Fibrosis suck. My life prior to cancer was already full of chronic pain, doctor appts, stress, and living a Spoonie life. Now add all of this into my day and it seems 24/7 I am just treating symptoms, at physical therapy appts, onco appts, and other dr appts. In the last 3 weeks since RADs finished, I've had 8 dr appts and 3 PT rehabs. No end in sight.
Just soooooo tired of this. Having to wear a compression prosthesis on my L breast 8-12 hours a day to combat the Fribrosis/Lymphedema is painful and frustrating. Going to PT twice a week and then to wake up next morning feeling like I was hit by a truck (even using the gentlest of treatments at PT) is difficult at best. I guess at least upside is Elisabeth (my cancer rehab wonderwoman PT) thinks we are making progress and the adhesions are lossening a bit between my scars and my range of motion is still improving.
On top of that the whole having to switch from Cymbalta to Pristiq in order to at some point take Tamoxifen is just killing me. Going on 6 weeks of this particular nightmare. I can't wait to tell my MO and my Psych to take Pristiq and shove it mid December, and if there's nothing else I can take to keep me mentally healthy with Tamoxifen than I choose mental health. I have to.
Sorry to be such a downer but I am just really struggling, mentally and physically. Most of my life I've been sick, fatigued, in pain, last year when I was planning this move back home I was looking forward to a new start and then cancer happened. Oh well, right? The best laid plans...of a 41 year old woman. Le Sigh.
Tomorrow will be better I know. Nights are just so hard.
--------
Long story short ---> Being a Spoonie w/o Cancer sucked. Being a Spoonie w/ Cancer sucks, but to a whole nother degree. Uggh.
0 -
Spoonie - I really feel you know what is best for you, should you just stop taking Pristiq? Can you call your therapist in advance of the appointment? If you are struggling this much, think of it like an "emergency" - maybe you need an emergency session, something like that.
What helps you? The fluffs? Uplifting music? Writing? Maybe do some of what you know has lifted your spirits in the past, just to counteract what's happening with Pristiq. I took Tucker and Domino for a longer walk after my radiation treatment today and this time went with my headphones on (which I don't usually do) and somehow it uplifted me more on the walk, I even started dancing about, and then that added the endorphins so it was a net net plus. Whatever works for you give it a go?
If I were you and you know these side effects are super toxic, just stop taking the drug. You know your body best, the doctors always prescribe things and hope for the best, and then adjust if the side effects are too great. It's sounding like you need to make an adjustment now, so make it. If this means you take cymbalta and don't take tamoxifen, you will have to consider if that's a better path than pristiq with tamoxifen.
I forget if I shared this already, but I found the story of this lady who beat breast cancer naturally - she does free consultations and I was going to connect with her just to see what she said. Want me to keep you posted? Maybe you might want to look into her story too? It's at least encouraging regarding the natural things you can do to keep breast cancer from coming back. https://theresadinallo.com/
Like you know, for me, I'm going to give tamoxifen a try - partly because there was cancer in my sentinel nodes and radiation + tamoxifen is my way to treat that without having to do chemo, and partly because I've don't take any other medication and have been skating through radiation with no side effects so far, so I'm hopeful that in my case, I can figure out a way to have little to no side effects on tamoxifen. But my case is different from yours and we all need to do what's right for us. I'm still also doing the diet and exercise stuff... if I didn't have my husband or my parents and sister and niece to think about, I might actually try not taking tamoxifen and see if I can succeed beating the breast cancer with ONLY diet and exercise. But I have them to think about and since tamoxifen is my ticket out of chemo, I'll try it.
But for you, do what's right for you. We're all snowflakes, we are all different, and we know what's best for our bodies and our minds... go with what you feel is right for you.
0 -
Hey Pebbles, thanks for posting. I appreciate it. I know we are battling our different wars and it means much to me when others take the time to offer some support. Truly, thank you.
I really don't know what more I can do at the moment. I already am seeing my counselor 2 x week while I'm going through this. I have to document all these "distress management skills" daily in order to show that I am doing what my therapist suggests in order to "cope" with these dang side effects and disturbing thoughts Pristiq is giving me.
Perhaps my psych would say stop taking it if I told her things are not getting better, but part of me is really trying to fight this out, ride it out, whatever, so that I know I've tried, really tried to do all I can in order to get on to a med that will allow me to try taking Tamoxifen. If it doesn't work out that way, then I know I did what I could.
I could probably say no more and they'd have to concede but for my own self I guess I'm battling on. If that makes sense?
It really sucks and is difficult but I guess I just need to take it day by day. Maybe tomorrow I'll wave the white flag, maybe not. It's kind of how I've taken to looking at taking Tamoxifen in the future. I know, almost with a certainty my body will not take kindly to Tamoxifen, given my chronic illnesses and previous medical history. Yet I've convinced myself that I will just tell myself I'll take it for this month and see how it goes. I can do anything for a month. Maybe in the end a ton of months will add up to 5 years and I'll have made it. Maybe not. Time will tell.
Thanks also for the link. I'll will bookmark it and read when I can. Wishing you the best of luck when you contact her. I hope she can be a great resource for you on that particular path. Keep me posted!
 I already work with a Homeopath/Naturopath/Acupuncturist so she has been working hand-in-hand with me in order to fine tune my supplements, herbs, and so forth to give me as much of an edge as we can. She's a gem and I'm so thankful she's been with me, helping battle my Lyme Disease and other illnesses for the past 5 years. Having her on board the cancer train is reassuring.
I already work with a Homeopath/Naturopath/Acupuncturist so she has been working hand-in-hand with me in order to fine tune my supplements, herbs, and so forth to give me as much of an edge as we can. She's a gem and I'm so thankful she's been with me, helping battle my Lyme Disease and other illnesses for the past 5 years. Having her on board the cancer train is reassuring.Sooo another day down and 11 more down until I see my MO. I can do this.
0 -
Spoonie - I'm totally here for you, and I SOooo admire that you are going to battle this out! OK, fight the good fight and please know that you have support all around you! You can do this! One day at a time is the right approach.
Also if it helps, my friend's boyfriend encounters a lot of women who are on tamoxifen in his line of work (he's an anesthesiologist) and he told me that most women do fine on it. The major side effects are few and far between from what he's encountered. My other friend's sister is on it and doesn't think twice about it. Like you, I'm really wary based on the side effects I've heard about, but I will also grasp onto any GOOD stories I can find to also give me resolve to soldier through it.
I will keep you posted if the Theresa Dinallo lady has any good advice.
0 -
Thanks again Pebbles!
It's great to hear that others have little to no SEs. I can only hope, however I have learned from my long medical history that the best way for me to survive going forward is to not have high expectations and just be surprised if things go well!

----------
Posting this here, (sorry for multiple posts) but want to be able to find this again when I talk to my MO in 2 weeks.
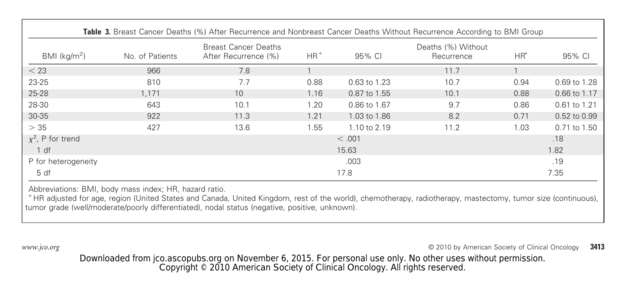
Interesting studies I found regarding Tamoxifen efficacy/overall survival related to premeno women & BMI (body mass index).
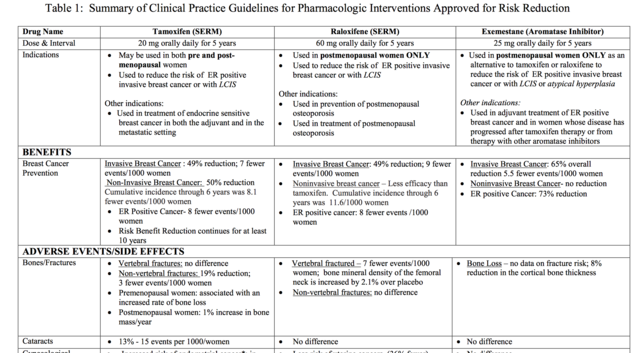
See table below -- under Tamoxifen "contraindicated" for BMI > 25 kg/m
My MO never mentioned this, and though I am not obese, I am overweight and this is something I will be asking her about when I see her in 2 weeks.
--------
Effect of body mass index on the efficacy of adjuvant tamoxifen in premenopausal patients
2014
https://www.ncbi.nlm.nih.gov/pubmed/27061527
RESULTS:
In both normal weight and overweight patients, the baseline clinicopathologic properties and the treatment history with radiotherapy and chemotherapy were similar and no statistical significant difference could be detected. Tamoxifen in combination with luteinizing hormone-releasing hormone (LHRH) agonist was used in 33% (136/408) of the patients in Arm A and in 22% (91/418) of patients in Arm B (p<0.001). Three-year disease free survival (DFS) rates were 89% and 87% in arm A and arm B, respectively (p=0.39). Three-year overall survival (OS) rates were 99% in arm A and 94% in arm B which appeared to be of significance (p=0.028). In univariate analysis no statistical significant effect of LHRH agonist usage on DFS (p=0.58) and OS (p=0.96) was found.
CONCLUSION:
Although BMI had no negative effect on recurrence risk, poor OS (overall survival) was observed in overweight and obese premenopausal breast cancer patients with hormone-receptor positive tumors who were treated with tamoxifen.
--------
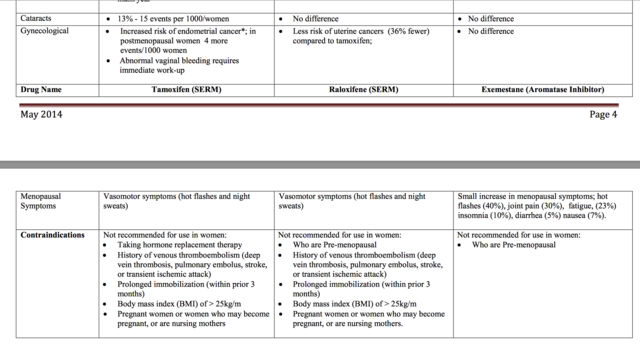
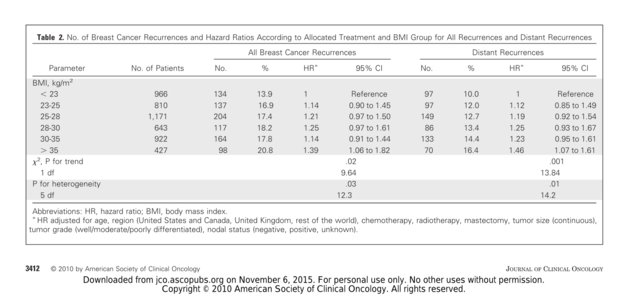
Effect of body mass index on recurrences in tamoxifen and anastrozole treated women
2010
https://www.ncbi.nlm.nih.gov/pubmed/20547990
Results: Overall, women with a high BMI (BMI > 35 kg/m(2)) at baseline had more recurrences than those women with a low BMI (BMI < 23 kg/m(2); adjusted hazard ratio [HR], 1.39; 95% CI, 1.06 to 1.82; P(heterogeneity) = .03) and significantly more distant recurrences (adjusted HR, 1.46; 95% CI, 1.07 to 1.61; P(heterogeneity) = .01). Overall, the relative benefit of anastrozole versus tamoxifen was nonsignificantly better in thin women compared to overweight women.
CONCLUSION:
These results confirm the poorer prognosis of obese women with early-stage breast cancer. Recurrence rates were lower for anastrozole than tamoxifen for all BMI quintiles. Our results suggest that the relative efficacy of anastrozole compared to tamoxifen is greater in thin postmenopausal women and higher doses or more complete inhibitors might be more effective in overweight women, but this requires independent confirmation.
------
The predictive impact of body mass index on the efficacy of extended adjuvant endocrine treatment
https://www.nature.com/articles/bjc2013367
2013
Results:
In all, 634 patients (177 normal weight, 307 overweight, and 150 obese) patients were included in this analysis. Normal weight patients with additional 3 years of anastrozole halved their risk of disease recurrence (disease-free survival (DFS) HR 0.48; P=0.02) and death (HR 0.45; P=0.06) and had only a fifth of the risk of distant metastases (HR 0.22; P=0.05) compared with normal weight patients without any further treatment. In contrast, overweight+obese patients derived no benefit from additional 3 years of anastrozole (DFS HR 0.93; P=0.68; distant recurrence-free survival HR 0.91; P=0.78; and OS HR 0.9; P=0.68). The possible predictive impact of BMI on extended endocrine treatment could be strengthened by a Cox regression interaction model between BMI and treatment (P=0.07).
Conclusion:
Body mass index may be used to predict outcome benefit of extended AI treatment in patients with receptor-positive breast cancer.
0 -
Spoonie - thank you SOooo much for posting that information! I'm also overweight (big reason why I've been trying to lose weight... I'm down 25 lbs but have 15-25 lbs more to go), so this information is super useful. I'm going to print this out and bring it to my oncologist as well - I meet with him on Dec. 14th, post radiation, to discuss starting tamoxifen etc.
I'll share with you what he says and please do the same for what you hear as well!
0 -
Super! By the way, I'll be seeing my MO on the same day! LOL! Good luck with your visit!
 0
0 -
Well, that's settled everyone.
I've been doing research on my various chronic illnesses, namely Chronic Late Stage Neurological Lyme Disease and multiple co-infections (Bartonella, Babesia, and Ehrlichiosis) and the contraindications of Tamoxifen.
Thankfully I was my own advocate because I found some very troubling things that apply specifically to my own medical history and since I know it's complex I can't blame my MO or Onc Team. They specialize in cancer, not in Lyme. But I'm disappointed that my Lyme team did not point this out.
Anyway long story as short as possible....(just in case others with Lyme Disease stumble upon this at some time):
According to this study, The Effects of Tamoxifen on Immunity https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902982/#R19
Tamoxifen is an IMMUNE MODULATOR (aka an immune system suppressant variant) resulting in lowered lab values such as CD4, CD57 (natural killer cells), Auto-Antibody productions (ANA, RF, etc), B-Lymphocytes,TNF-alpha, TGF-beta, and more.
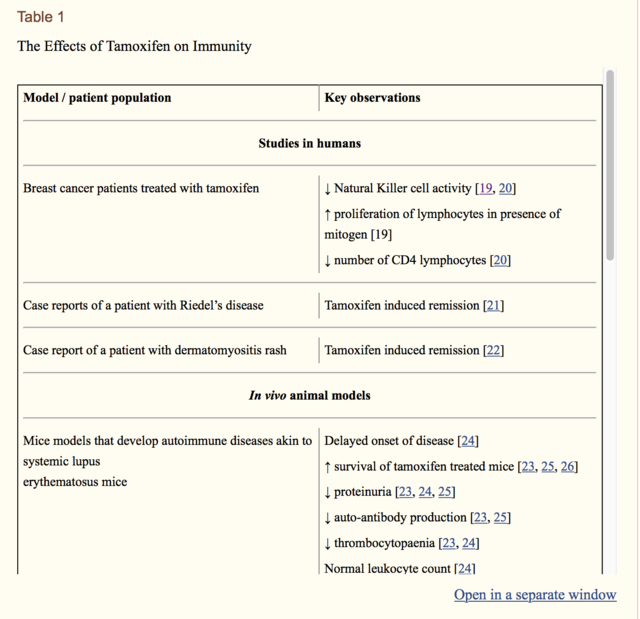
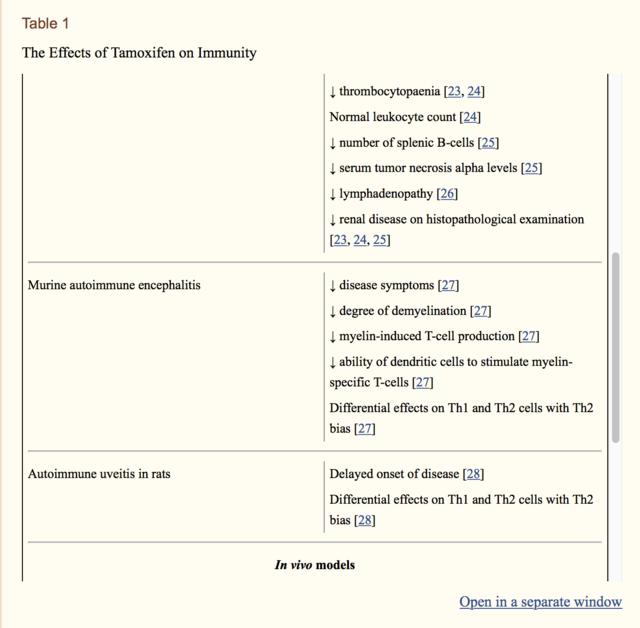
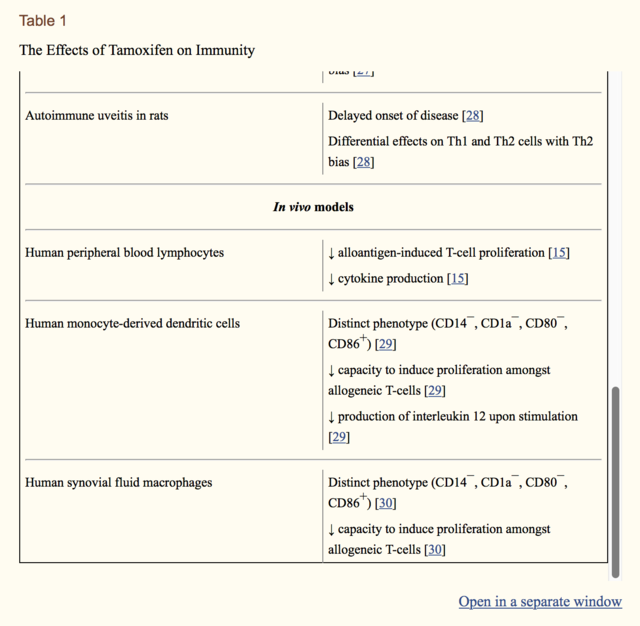
All of these are tests that my Infectious Disease team regularly monitor....and yet....no one mentioned the dangers of my taking Tamoxifen and how it would affect my primary disease and my immune systems ability to fight these multiple chronic infections. Uggh.
----------
Immunomodulatory effects of anti-estrogenic drugs
2012
"Tamoxifen, which functions as a competitive partial agonist-inhibitor of estrogen at its receptor, has been widely used for more than three decades for adjuvant endocrine treatment in breast cancer. Currently, other effective drugs for endocrine therapy include raloxifene, different aromatase inhibitors (particularly third-generation agents) and luteinizing hormone-releasing hormone agonists. In recent years, a growing body of evidence suggests that these drugs can also act as immune modulators by altering the function of various leukocytes and the release of different cytokines. Moreover, there is evidence that anti-estrogens may prove to be beneficial in the treatment or prevention of some autoimmune diseases due to their effects on immune function."
https://www.deepdyve.com/lp/de-gruyter/immunomodulatory-effects-of-anti-estrogenic-drugs-tyQYutFafl
"Inter- estingly, various anti-estrogenic drugs have also been demonstrated to affect the immune system. The immunomodulatory effects described thus far include alterations in the fun- ction of lymphocytes, macrophages, monocytes and dendritic cells as well as effects on cytokines. Additionally, anti-estrogenic drugs have exhibited some immune modulations related to autoimmune disorders, possibly leading to other uses."
-----------
There is ABSOLUTELY no way I will take Tamoxifen knowing this.
For some people with Psorasis, SLE, MS, etc, this would be a help I'd imagine since it would settle their immune system down a bit and keep it from over-attacking their bodies.
However, for me, that would be a nail in the coffin.
I will take this report and other reports/labs to my MO to show her how this will impact me in a huge way.
I know that Tamoxifen "might" reduce my risk of recurrence or future BC by 40-50%, but I CURRENTLY fight and treat these diseases every single day. If I let these run rampant I will die...not if but just a question of when.
At one point in my life, about 10 years ago, when Lyme was wreaking havoc in my system and no one would treat me, I couldn't walk, bedbound 24-7, was losing the ability to talk, short term memory was non-existent, was sufferring myocarditis which nearly put my heart out of commission, pain was off the charts, QOL non-existent, and much more. My brain was sufferring deterioration and inflammation that was similar (words on my MRI's and was wrongly dxed with MS) to that seen in Demylenation Disease.
I have worked soooooo hard to get some semblance of a life back, no way I will risk throwing that away for a "maybe".
Soooo yeah...Tamoxifen is a no for me and basically.
IMO, should be off the table for any that are immunocompromised or battling chronic, life-altering system-wide infections. Not a doctor obviously, but wow, just another piece of the pie that shows we HAVE to be our ADVOCATe, no one else will do it for us.
Do your homework everyone. It is so critical.
0 -
Spoonie - thanks so much for posting that. I am on the fence now about Tamoxifen...
 0
0 -
HI Pebbles - It's bothersome to me that this isn't discussed with patients. I'm sorry to be the bearer of this type of news and part of me is sure most doctors will scoff at it and say "oh it's only in vivo" but for me that's enough proof.
And then you can add this study on to it as well, that used Tamoxifen to prevent immune system cells from doing their normal job..
2016
"Although commonly used for cancer treatment, tamoxifen is used in the laboratory as a tool to activate specific genes in genetically engineered mice. The tool allows researchers to turn genes on and off in specific tissues at will....The breast cancer drug tamoxifen appears to protect light-sensitive cells in the eye from degeneration, according to a new study in mice. The drug prevented immune cells from removing injured photoreceptors, the light-sensitive cells of the retina in the back of the eye. The study, recently reported in the Journal of Neuroscience, suggests tamoxifen might work for the treatment of age-related macular degeneration (AMD) and retinitis pigmentosa (RP), blinding diseases that lack good treatment options."
Which, granted, if a person is suffering from these diseases, this is awesome news! A new possible treatment. However, it's just more proof that this drug affects so much more than we know and more than I comfortable with given my own tenuous health and conditions, prior to adding BC to the mix.
I remember reading some various people mentioning that they dealt with Photosensitivity while on Tamoxifen, and I wonder if the basics of this study might be a reason? Curious.
I'm going to continue my search for more info on this role that Tamoxifen plays with our immune system.
0 -
Well, here's evidence related to Diabetes and the immune system affects when given Tamoxifen...
Beneficial Effects of Tamoxifen Treatment in Type 1 Diabetes
http://diabetes.diabetesjournals.org/content/67/Supplement_1/2155-P
2018
Abstract
"Type 1 diabetes (T1D) results from the destruction of pancreatic β-cell through the β-cell specific autoimmune process. β-cell autoantigens, macrophages, dendritic cells (DC), B lymphocytes, and T lymphocytes have been implicated in the pathogenesis of autoimmune diabetes. Tamoxifen is a selective estrogen receptor modulators (SERM), used in the treatment of breast cancer. Research reports have shown that tamoxifen might decrease the strength of immune responses through modulation of DC differentiation and activation, and it may depress immunity. In NOD/ShiLtJ mice (female), which is a polygenic model for T1D, we found that tamoxifen exerts antidiabetic effects through acting on the immune system, leading to the suppression of insulitis and systemic inflammatory cytokine production in the in-vivo model. Tamoxifen therapy preserved the β-cell mass and prevented the development of T1D. Tamoxifen providing β-cell protection and immunoinhibitory effects offer a novel insight into the possible role of tamoxifen in the regulation of islet cell function and glucose homeostasis. These findings are significant and useful for clinical application."
--------------
And evidence related to the decrease of allergies when given Tamoxifen....
Tamoxifen counteracts the allergic immune response and improves allergen‐induced dermatitis in mice
https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1365-2222.2010.03472.x
2010
"Results Preventive TX treatment interfered with all aspects of the allergic immune response, leading to a reduction of allergen‐specific Ig levels (IgE, IgG1 and IgG2a), a skewing effect in the T cell compartment with the inhibition of IL‐4 and an abrogation of ear swelling responses. Interestingly, a therapeutic TX administration was also effective in reducing Ig levels and ear swelling responses. The vigorous systemic effects were additionally mirrored by local changes in allergen‐dependent dermatitis with reduced clinical symptoms, diminished epidermal thickness and decreased CD4+ and CD8+ cell infiltrates.
Conclusion TX inhibits allergic responses when given preventively and also therapeutically, and improves allergen‐induced dermatitis. Because of its effectiveness, TX could bear significant therapeutic potential for the treatment of allergies."
0 -
And I guess this is why Tamoxifen effects immunity --- the cells that work on immunity are sensitive to estrogen. Take away or block said estrogen and of course it will have a down stream effect. Hmmm.
http://www.jimmunol.org/content/175/4/2666
Abstract
"Most immune cells, including myeloid progenitors and terminally differentiated dendritic cells (DC), express estrogen receptors (ER) making these cells sensitive to estrogens. Our laboratory recently demonstrated that 17-β-estradiol (E2) promotes the GM-CSF-mediated development of CD11c+CD11bint DC from murine bone marrow precursors. We tested whether the therapeutic selective estrogen receptor modulators (SERM), raloxifene and tamoxifen, can perturb DC development and activation. SERM, used in treatment of breast cancer and osteoporosis, bind to ER and mediate tissue-specific agonistic or antagonistic effects. Raloxifene and tamoxifen inhibited the differentiation of estrogen-dependent DC from bone marrow precursors ex vivo in competition experiments with physiological levels of E2. DC differentiated in the presence of SERM were assessed for their capacity to internalize fluoresceinated Ags as well as respond to inflammatory stimuli by increasing surface expression of molecules important for APC function. Although SERM-exposed DC exhibited increased ability to internalize Ags, they were hyporesponsive to bacterial LPS: relative to control DC, they less efficiently up-regulated the expression of MHC class II, CD86, and to a lesser extent, CD80 and CD40. This phenotype indicates that these SERM act to maintain DC in an immature state by inhibiting DC responsiveness to inflammatory stimuli. Thus, raloxifene and tamoxifen impair E2-promoted DC differentiation and reduce the immunostimulatory capacity of DC. These observations suggest that SERM may depress immunity when given to healthy individuals for the prevention of osteoporosis and breast cancer and may interfere with immunotherapeutic strategies to improve antitumor immunity in breast cancer patients."
"Several studies indicate that SERM influence multiple aspects of the immune system. SERM have been shown to modulate a number of pro- and anti-inflammatory cytokines (18, 19, 20, 21). Furthermore, in vivo exposure of mice to tamoxifen (22) or raloxifene (23) reduced lymphoid organ weights suggesting that these SERM may dampen immune responses. In agreement with this idea, raloxifene negatively regulated B lymphopoiesis in BM in two separate studies (24, 25), and tamoxifen treatment was shown to reduce the severity of autoimmune disease in mouse models (18, 22, 26). However, the observation that tamoxifen has beneficial effects on autoimmune disease are contradicted by data suggesting that tamoxifen can augment lymphocyte activation (22, 27). Regardless, because ER are expressed by many cells of the immune system, including DC (28, 29, 30, 31), it should not be surprising that SERM possess immunomodulatory properties."
0 -
Oh hey, look there's a whole book on it....
Tamoxifen: Beyond The AntiEstrogen
I won't paste all the tables of info that are in this book, but if immunity and immune response due to your medical history is of any major daily concern, then I would bring this up to your ONCO team for a discussion.
SMH.
0 -
deleted
0 -
Ok, according to the CDC, regarding getting live vaccines, those on immunosuppressive drugs (look at picture, last line...tamoxifen is noted....although stated it is LESS immunosuppressive than others...still considered immunosuppresive), should wait 3 months before getting a vaccine after stopping said drug, and waiting at least a month before restarting the drug after being vacinated.
I'm sure my MO never mentioned this to me....SMH.
Immunocompromised Travelers
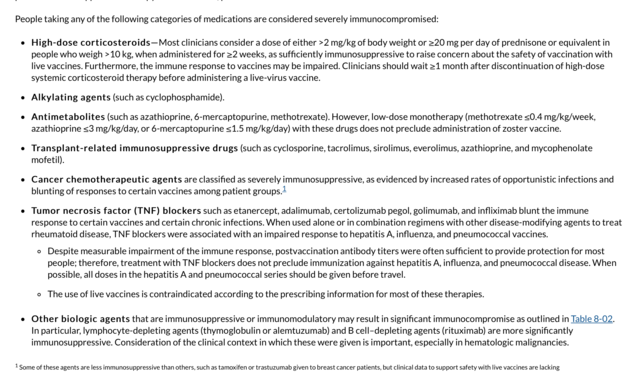
Duration of Iatrogenic Immune Compromise
"The period of time clinicians should wait after discontinuation of immunosuppressive therapies before administering a live vaccine is not consistent across all live vaccines. For cancer chemotherapy, radiation therapy, and highly immunosuppressive medications (exclusive of lymphocyte-depleting agents and organ transplant rejection prophylaxis), the waiting period is 3 months. For lymphocyte-depleting (alemtuzumab and rituximab) agents, the waiting period is ≥6 months, although many experts believe the waiting period should be ≥1 year. For steroid regimens considered immunosuppressive (see above), wait 1 month. Zoster vaccine is exceptional and may be given 1 month after any highly immunosuppressive agent, although many experts advocate waiting ≥1 year for anti– B cell antibodies and other lymphocyte-depleting agents. For agents not considered highly immunosuppressive (see Table 8-02), consultation with the prescribing clinician (and possibly a hospital pharmacist) is recommended to manage individual patients and estimate degree of immunosuppression. No basis exists for interpreting laboratory studies of immune parameters to evaluate vaccine safety or efficacy. Restarting immunosuppression after live vaccination has not been studied, but some experts would recommend waiting at least 1 month."
0 -
Thank you, thank you, thank you spoonie! You have certainly contributed to the case in favor of “questioning” authority! (politely of course) and of being your own advocate. In my humble opinion, MOs are so invested in following the current “standard of care” that they have no time to research how their individual patient differs from the norm.
0 -
"In my humble opinion, MOs are so invested in following the current "standard of care" that they have no time to research how their individual patient differs from the norm."Sara -- > I agree with you 100%. Maybe some day that will change. We can hope. Wishing you the best on your own journey.
0 -
I was on it for 6 months before switching to ovarian suppression and aromasin. I was TERRIFIED but I had zero side effects except brain fog the first week. I just wanted to share because I think we hear a lot more from people that struggle.
0 -
LovestoFly - I am meeting with my MO tomorrow to discuss making that switch; I’ve been off of Tamoxifen for 5 weeks fue yo various SEs, the worst being bad joint and muscle pain.
Why did you make the switch?
0