Any Early 40s Declining Tamoxifen?
Comments
-
Sooooo, I see my MO tomorrow.
I'm as nervous as a cat on a hot tin roof. Ugggh.
Dreading telling her I'm declining Tamoxifen but I know this is what's best for me.
Not sure what other options she may outline, but really feel that for now, all I can mentally and physically handle is taking DIM, eating right, and exercising as much as my conditions allow.
Totally looking forward to getting back on my Cymbalta though, LET ME TELL YA!
 Psych won't rx it for me until after my MO has informed her of whatever is the next step. Can't wait to get off this dang Pristiq and the hellish ride it gave me. According to my homeopath's testing my liver and gallbladder had basically cut their work load to just a trickle in protest over the drug. Uggh. Can't wait to wave buh-bye to that pill.
Psych won't rx it for me until after my MO has informed her of whatever is the next step. Can't wait to get off this dang Pristiq and the hellish ride it gave me. According to my homeopath's testing my liver and gallbladder had basically cut their work load to just a trickle in protest over the drug. Uggh. Can't wait to wave buh-bye to that pill.Anyway, wish me luck tomorrow yall.
0 -
Spoonie77,
Good luck with your MO app't. tomorrow. You'll do fine. Try and get a restful night's sleep. Let us know how it goes.
0 -
Spoonie - wishing you luck! We're there with you in spirit. Keep us posted on how it goes.
Domino is sending her best concerned look:
0 -
Good luck! Thinking of you!
0 -
PebblesV - Domino is truly one of the cutest pups I've ever seen!
Spoonie - easier said than done, but don't let the MO make you feel guilty, or stupid or frightened. You've done the research. You've taken the time and given it consideration. You're content with your decision.
I just made the decision to stop hormonals after 9 months of misery. I was really surprised how much my MO supported my decision.
0 -
Thanks everyone and thank you Domino!! (Gosh she is so freakin adorbs!!!
 )
) VL22 I really appreciate the extra advice you offered. In my younger days I was such a people pleaser and telling people NO used to be difficult. I've come a long way on that, but it's still difficult at times. But you are entirely right, I've done the research and this is my choice. Thanks again.

I'll keep ya all posted. Appt is at 1pm. Hopefully I'll have encouraging news to report later this afternoon.
Hugs and healing to you my friends.
0 -
I'm upset. I'm depressed.
That meeting with MO did not go well. Not at all.
She sure is friendly but she seems so set in her ways and not open to hearing any other evidence, studies, or ideas. Let alone taking all of my other chronic conditions into account.
I'll post more when I can. Just in between tears and anger right now. This is too much. Am so tired of always having to fight so hard for the correct medical care all of my life. I thought, maybe with cancer it would be different, it started off that way but in the end it seems the fight is still the same, only life and death at risk this time.
Le Sigh.
 0
0 -
OMG Spoonie I was waiting with baited breath to hear how it went. Feel free to let it all out here, sometimes writing about it is cathartic.
Is there any way you can get a second opinion or different oncologist?
A LOT of people have said no to tamoxifen FYI and been just fine. A lot have said no to chemo when doctor's recommended it and they had to walk alone but the cancer never came back, they succeeded. I know it's funny writing this when I plan to give tamoxifen a try, but honestly I'm not even sure that's the right decision and I support you 100% behind yours. You have analyzed this, you know your own body best, you have to make the right decision for yourself and you are!
FYI I said no to a deeper axillary node dissection when they found cancer in my sentinel nodes. I feel right about it because, like you, I did a lot of research and found these studies that showed similar cases to mine where women who did just the sentinel node dissection had similar or better survival rates than the ones that did the full axillary node dissection. But I had to hold strong, the surgeon pushed back, the radiologist did too before I started radiation because he's friends with the surgeon. But I held my ground, and interestingly enough when I did the follow up with the same radiologist weeks later, I brought him a print-out of some of the studies and he claimed he was aware and told me it was all fine, that he only wanted to make sure beforehand because it would effect his treatment plan on the radiation, but that he treated the nodes since I didn't do the extra surgery and felt really confident that we "got it". So I don't know if he caved a little because I didn't budge but anyways just wanted to share that.
We do a lot more research for ourselves and our individual cases I think. These were the things I found that help reassure me on my decision re: sentinel node biopsy vs. axillary node dissection... https://www.ncbi.nlm.nih.gov/pubmed/28898379 and https://www.everydayhealth.com/breast-cancer/treat... and https://jamanetwork.com/journals/jama/article-abst...
By the way, I did that consultation with Theresa Dinallo and she told me not to take tamoxifen. She's all holistic so she didn't do anything, not even surgery, but she beat it! The first consultation is free, maybe in your case you might want to connect with her? After that she has a program that costs a fortune though, I'm not going to do anything further with her, I just wanted her POV to weigh in with everything else, but there are others with your point of view.
A Domino PUPPY PIC for you!!!
 0
0 -
So, after much thought, and trying to not think...ironic I know...I still can't put it all down on "paper". I will try to get some of it out....
Sorry in advance, this is probably going to be long.
Thanks Pebbles for the support. At least I have the appt over with. She knows I'm not taking Tamoxifen though she doesn't believe in any of my reasoning what so ever. I'll touch on that tomorrow maybe. I'm still trying to wrap my head around that part of the appt.
In general, as I was driving home I decided that I need to get a second opinion, to look for a doctor that specializes in cancer in patients with other conditions maybe, if that even exists. IDK.
One good thing that came from the visit is that I finally convinced my MO to order a bone scan for me.
It went like this....
"How am I supposed to know if I have symptoms of metasis/distant recurrence since I ALREADY have symptoms that would be signs of such every single day throughout my body?". She said that it would increase and not decrease over two or three weeks. I told her that would be a problem then since sometimes my symptoms flare for a month or more and then decrease. Sometimes just for a few days. It all changes. Plus I have a history of MRI abnormalities, white-matter lesions, lymph nodes enlarged near my spine, poly-arthrical degenerative disease, diminished bone density, benign calcifications in my jaw, nodules in my right lung, a barky cough that comes and comes over the last 2 years, trouble breathing, fevers on a daily/weekly basis, and C4 plus TGF Beta labs that have been off the charts elevated for years (like in range is around 3,000...some of mine have been in the 32K range!), and CD57 levels that don't even register on their scale they are so low (range is at least >60 cells and/or 1-4%, mine are <5 cells and <1%) and have been that way for the past 10 years no matter what I try to beef them up.
So you can see, or at least most people I'd think would see, that there is history here to take into account.
After that, she reluctantly agreed to order a bone scan for me to get a baseline. I think more to get me to shut up than because she believed me. IDK. Just my impression. I have that tomorrow, so should know results next week I'm guessing.
She said there was NO way she would ever order a PET scan for me. EVER. Unless I have specific symptoms, which I don't according to her at this time, so therefore no PET SCAN. In general, she stated she doesn't do them and thinks they do more harm then good.
I understand her reasoning for probably 95% of patients, meaning that you end up chasing rabbits, increasing costs, and mental anguish all to come up with "nothing" or benign results, which is great news but at a cost.
But what about that 10%, especially in younger women (according to study 1 & study 2 ) that end up being upstaged by PET Scans finding distant metastasis that did not show up in the lymph nodes, etc or have symptoms that are masked by other conditions or masked in screening by dense breasts?
She didn't want to hear it. And that's when "IT" happened....
When she said (and I quote)
"What?! Do YOU want to FIND Stage IV?! What then?!"
in reply to my questions about PET Scans....I was taken aback. Tremendously.
My response to her was that I would rather know than not know.
She said "Why? What would you do with the information since you don't want any treatment?".
Again, shocked. I replied, "Well, if I knew I had Stage IV that's very different than Stage I or II. I would agree to any treatments that would help since I had evidence of disease."
Anyway, that whole part of the conversation was really abrupt, shocking, and disturbing. It's going to linger with me for a long time.
We went on to talk about other topics ---
She had no clue about many of the studies I've been reading. Especially ones about alternative treatments like DIM or concerning the latest studies on Tamoxifen gel. Which to me seems like she should be aware of but she said she'd actually never ever heard of it. Ok, not everyone probably reads tons of studies. But then she said she doesn't pay attention to any trials or studies in general until they are approved by the FDA, third arm studies. Which I get, yet, it seemed she would not even look at the logic and information presented in studies involving small mammals and such. That the evidence that's there doesn't matter. I could be wrong but that was my impression.
She did agree with me on one study that shows women with personal history of BC & dense breasts should have alternating breast MRI's and Mammos. So going forward I'll have a BMRI 6 months after my surgery date (Feb) and then in Aug I'll have a Mammo. Rinse and repeat for the next 3 years. AFter that she said I could go down to a mammo every year. I am going to push for a 3D one maybe or every other year add a BMRI in there with the mammo. IDK. But I feel good about this agreement her and I reached.
Well, there is lots more I could post, but need to sleep, will finish up tomorrow when I get home. Bone scan early in the morning. At least there was some progress but mainly this just showed me that I need to search out someone who is more like me, wanting to branch out where reasonable, ensuring all my conditions are taken into account, and to be open to listening on both sides. Thanks for reading anyone and everyone....maybe this all might help someone else someday. Guess that's why I write all down and send it into the Interwebs instead of just processing it on my own.
Sending lots of hugs to all my fellow BC warriors....keep fighting!
0 -
Hi Spoonie77,
Sorry to hear you had such an upsetting appointment with the MO. You were able to negotiate follow up treatment with alternating mammograms and Breast MRI's so that's good. It seems the MO was way out of line with her attitude and response to you. Getting a second opinion sounds like a good idea. Anymore if providers refuse to listen or help me then I'm done with them. Not always easy to switch depending on what resources are available in your area.
0 -
I'm so angry on your behalf.
I hope you can find a different doctor who will work with you instead of at you.
We can all Google the current standard of care and treatment recommendations. What's the point of a doctor if they are just regurgitating that at you, regardless of your personal situation
0 -
hi spoonie, I am sorry you are going through this. I am as well. I have started on the tamoxifen and started originally at 20mg and it was horrible, since then I stopped and restarted at 5mg. I am due to go up to 10 this week. I will say I have acclimated to 5 so I hope This process works. In reading your story I am wondering did you have the Mammaprint or oncotype? Mammaprint from my understanding speaks more to statistics without tamoxifen? Maybe that’s something to discuss with MO? I feel for you and am right there too
0 -
Thanks Salamadra. I'm still processing everything. It was much to take in...
Samnjb - I needed to have both the Onco & Mammoprint done in the beginning. Onco was in a gray area for me and I asked for confirmation before agreeing to no chemo. Mammo did indeed confirm. Just got my hard copy of the results yesterday from my appt and you are right, my recurrence rates without Tamox are listed. Thank you for that.
I'll be posting more later about the appt on another thread i think because Im curious what others would say about some of her practices.
Thanks again for offering some support. I needed it after yesterday's appt. Le Sigh.
0 -
Hi Spoonie,
I really think your MO was out of line. We are stressed enough when it comes to fighting this breast cancer and all the treatments, and for her to have said all that stuff to you (what you put in bold and quotes) was terrible. I am SOooo sorry that dealing with everything you are dealing with in the spoonie life that happened too. Sending hugs!
I just met with my MO this morning and my experience was complete opposite yours. I wish you could see him! I feel very reassured on my plan of action and feel good that he's the one I'll be following up with regularly, that he's the right 'fit' for me - the most important thing he said was we can be fluid, we have a plan of action, but there's no lock and key saying you have to stick to that plan, and if at any point tamoxifen doesn't work for me, we'll change it up. It got be thinking on the drive back how important having the right oncologist to be your partner in this is, so I really hope you can find another that you can also feel reassured and supported with. If you live in CA, let me know and I'll PM you who my doctor is!
Here's the summary of a few key things from my visit:
- He let me lead it. He didn't start in with what to do, but wanted to know my update and where I was at.
- I thought he would pressure me to start tamoxifen right away. Instead, when I told him my husband and I wanted to do one more IVF cycle, he said it was fine to wait to take tamoxifen until we finish that cycle (in January) and while he didn't have any concerns with me starting right after the egg-pulling surgery, if it made me more comfortable, I could wait a week after surgery to start tamoxifen.
- While his recommended dose is the standard 20mg, I told him about one of the woman on these boards who had built herself up, starting at 10mg for several weeks and then going to 20mg. So he said he could prescribe to me at 10mg so that I could do the same. He just asked I take no more than 6 months to 'build up' to the proper dosage, I told him my plan was to do a month like this other woman.
- He told me if I was super nervous about tamoxifen, we could try a newer medication (arimidex) instead. However they would have to induce early menopause to do that, which was a bit drastic. But it's an option if I wanted to take that option.
- I told him about the women who get hysterectomies (uterus taken out) and for me at 43,that was not something I would be willing to do if I didn't need to. Much to my reassurance, he scoffed at the idea of a hysterectomy just to manage tamoxifen and told me that was way too drastic if not necessary. That reassured me as I've seen other doctors pressure their patients into a hysterectomy (happened to my friend).
- On blood clots, he said it tends to happen with older women, more obese, who are sedentary. And there are ways to minimize the chance of that side effect - exercise is huge, he really believes in that. And some women take baby aspirin, but then there are other risks of bleeding easily. For me, he might recommend a baby aspirin if I travel on a long flight but don't need it daily. Unless I want it! He left it all up to me.
- On the risk of uterine / endometrial cancer, unfortunately it's a risk but he said it's less than 1%. I asked if any of his patients have gotten it and he said just one, a woman in her 70's. He thinks the risk is higher for older post-menopausal women. The only way to manage for it is to get yearly gyno exams. He said if I wanted an annual ultrasound instead, he's order that for me.
- I did ask about tamoxifen's impact on the immune system. He said he hadn't seen a link (that from what he's seen, tamoxifen has no effect on the immune system. I didn't have time to print all your studies but I do feel that I can present them to him and he would objectively review them.
He explained a bit more about tamoxifen, he says it's a hormone that acts like estrogen but doesn't stimulate breast cancer, so that's why it's prescribed to help reduce the risk of breast cancer - because it will compete with estrogen to bind to the cells instead of estrogen, providing some benefits too like increased bone density aka bones will be stronger.
He believes exercise is a clear risk factor for breast cancer, as is obesity (he was impressed and pleased that I'd lost weight!). On nutrition, he didn't have any specifics on what to eat, just that it's about losing the fat percentage.
He also made sure to say, "It's not like we're going to lock you in a room, say take tamoxifen for 5 year, and throw away the key! If something is not going well, we stop it. We can be fluid. We have a plan, but the plan can always change."
With that, I felt SOooooo reassured that I'm with the right oncologist. I was so nervous before this meeting. So, here is the plan for me - since we are doing one more 'pull eggs' cycle, I have a bit of reprieve and don't have to take anything yet! Going to enjoy this time. There is no pressure to start tamoxifen now, even though I just got done with radiation. Around a week after the IVF surgery, I will start tamoxifen, and then make an appointment with him 1 to 1.5 months after I started (which he says is to do a check up and see how I'm tolerating it). After that, it's a check-up every 3 months which will include a breast exam, and the thing I'm happiest about is no barrage of tests! Hurrah! (note - I already did a CT scan and bone scan after my surgery and before radiation because of the two positive nodes... I was SO afraid he would want to do another CT or bone scan now and I don't want that, plus I hear you shouldn't do these more than once a year because of the radiation exposure, so I'm SOooo relieved at no more tests and scans and all that now).
For me, I actually want the forward path one where I can be left alone to my own devices to do what I've learned to keep this cancer from coming back through nutrition and exercise and lifestyle - and I'm OK with giving tamoxifen a try. But I also feel reassured that if at any point I feel it's not working for me, we can switch gears.
I feel so relieved and reassured on my personal plan of action after this meeting, and that's how you should have felt. I really hope that you will be able to find someone else who can work with you. I think integrated oncology is starting to grow so hopefully they have that option near you! There are some more naturalist doctors too that you might want to reach out to?
Hoping you find the right MO for you Spoonie. Hugs and healing.
0 -
Ohhhhh Pebbles.....I'm in tears of joy for you! What a great appointment you had. I feel reassured and I'm not even his patient!!!
 You are right, I wish I had had a similar experience. Your MO sounds heavenly. I'm ecstatic at how fluid, flexible, and "just for you" your treatment plan sounds. What a blessing.
You are right, I wish I had had a similar experience. Your MO sounds heavenly. I'm ecstatic at how fluid, flexible, and "just for you" your treatment plan sounds. What a blessing. I can't thank you enough for taking the time to share how things went in your world. I know it takes awhile to type everything out and what you shared really outlines the differences we experienced and what was lacking in mine. Additionally confiming my gut feeling that I do have to search for a new MO. One who is willing to listen and adapt, as your did.
Honestly, I can't stop smiling for you my friend! What a great member to have on your team! I sooooo wish I lived in CA so I could see him. And welp, for other reasons too --- sun, ocean, no snow, and hey, I could hang out with Pebbles! LOL!
Good luck on your 10mg start and my fingers are crossed for you egg pull! May everything go better than and according to plan!
 0
0 -
Oh and Pebbles -- I had found more studies, there are a ton (when you know what to search for eventually), and I will send you a PM with a few of them. In case you'd like to add them to the others when you see your MO next. Thanks again for the lovely post! It was so encouraging! I'm on a mission to find me a gem like him!

Posting some of the studies here for anyone that would like to research them or discuss them with their own team...
Tamoxifen Induced Lupus Erythematosushttps://www.omicsonline.org/tamoxifen-induced-lupus-erythematosus-2157-7609.1000138.pdf
Tamoxifen SLE Immune Study
https://ard.bmj.com/content/62/4/341
In Vivo Modulation of Natural Killer Cells By Tamoxifen
https://www.ncbi.nlm.nih.gov/pubmed/8334683
Immunomodulatory Effects Of Anti-Estrogenic Drugs
https://www.ncbi.nlm.nih.gov/pubmed/22750814
(the article that this references is a PDF which can be found here:https://content.sciendo.com/view/journals/acph/62/2/article-p141.xml
or if that doesn't work, by searching for this "Acta Pharm. 62 (2012) 141–155 Review DOI: 10.2478/v10007-012-0012-3 Immunomodulatory effects of anti-estrogenic drugsAMITABHA RAY* MONICA FICEK Saint James School of Medicine Anguilla, British West Indies "
Tamoxifen Augments The Innate Immune Function
https://www.ncbi.nlm.nih.gov/pubmed/26458291
The Effects of Tamoxifen on Immunity
0 -
Spoonie77 - I’m so glad all that detail helped! Yes I was as nervous as you before the meeting and feeling so good and reassured after that I thought of you and that terrible experience you had so I wanted to share mine and encourage you to find an MO that supports you and is flexible and adapts to YOUR needs.
BTW my husband is from MN and I lived in MN for 2 years for work! Worked in Eden Prairie and lived in Minneapolis.
And is CA to see me, or see this little Domino? LOL - she’s sending you puppy kisses for the weekend. Hope you can just relax and recoup this weekend.
Thx for the immune articles too, I will read them and share with my onc and see what he thinks!
 0
0 -
Hi Spoonie,
I took a look at some of the articles you posted tonight. I could be wrong in how I'm reading these, but it's sounding like tamoxifen enhances immunity? Below are my notes on the articles you posted... I'm *not* an expert, I didn't understand a lot of these terms so I googled them LOL. But I'm not as worried about tamoxifen and the immune system based on this... I'm a nit re-assured actually. Although for you I still support your choice, as you have so many things going on that tamoxifen might just mess with them. But for me, I think I'm a little encouraged that tamoxifen might actually help not hurt my immune system? Unless I'm reading this wrong?
Honestly I had to look up terms to better understand the studies, and some had too many terms to google so I just focused on the ones I could really understand... thoughts?
Tamoxifen SLE Immune Study
https://ard.bmj.com/content/62/4/341
-- This article seems to be saying that tamoxifen was beneficial in helping to increase immunity - see quotes: "At 6 months of age, 40% of the untreated mice died spontaneously, whereas all the tamoxifen treated mice were still alive... The results clearly show the remarkable therapeutic effects of tamoxifen on SLE of (NZB×NZW)F1 female mice and suggest that these beneficial effects are related to the specific reduction of IgG3 autoantibodies."
Later on it says, "Table 1 shows that at the age of 6 months all untreated mice had significant thrombocytopenia and proteinuria, whereas the tamoxifen treated mice had a normal number of thrombocytes and only mild (near normal) proteinuria, similar to the control young (2 months old) (NZB×NZW)F1 female mice... Our studies clearly demonstrate significant therapeutic effects of the oestrogen antagonist tamoxifen on the course of SLE in (NZB×NZW)F1 female mice. Tamoxifen treatment led to remarkable improvement of all lupus related clinical manifestations, including survival, thrombocytopenia, proteinuria, and glomerular immune depositions."
I looked up "thrombocytopenia" and that's a a condition with low blood platelet count, while "proteinuria" is exactly what is sounds like - abnormal quantities of protein in the urine which could damage the kidneys. So tamoxifen seems to help avoid these issues, which actually makes me feel a little better about taking it!
Immunomodulatory Effects Of Anti-Estrogenic Drugs
https://www.ncbi.nlm.nih.gov/pubmed/22750814
- This one seems to be saying that tamoxifen can help modulate (or manage) the immune system and might be considered a solution for that in the future? "In recent years, a growing body of evidence suggests that these drugs can also act as immune modulators by altering the function of various leukocytes and the release of different cytokines. Moreover, there is evidence that anti-estrogens may prove to be beneficial in the treatment or prevention of some autoimmune diseases due to their effects on immune function."
"immune modulator" seems to be a term to help treat things that result from an overactive or otherwise less functioning immune system, lhttps://www.ncbi.nlm.nih.gov/pubmed/21089249 - "Targeted immune modulators, commonly referred to as biological response modifiers or simply biologics, are a relatively new category of medications used in the treatment of certain types of immunologic and inflammatory diseases, including rheumatoid arthritis, juvenile idiopathic arthritis, ankylosing spondylitis, psoriatic arthritis, plaque psoriasis, Crohn's disease, and ulcerative colitis. "... ?
Tamoxifen Augments The Innate Immune Function
https://www.ncbi.nlm.nih.gov/pubmed/26458291
- This one says tamoxifen augments - aka enhances - the immune system...? : "Here, we find that tamoxifen stimulation enhances several pro-inflammatory pathways in human neutrophils, including chemotaxis, phagocytosis and neutrophil extracellular trap (NET) formation... Our results suggest that tamoxifen, and the lipid signalling pathways it modulates, merit further exploration as targets for boosting host innate immune function.
- I looked up 'neutrophils' and that's white blood cell count to fight off infections, so if tamoxifen is stimulating that, it's a good thing? https://www.verywellhealth.com/what-are-neutrophil... - "Neutrophils are a type of white blood cell (WBC or granulocyte) that protect us from infections, among other functions."
- "pro-inflammatory" is not always bad, sometimes good? https://www.researchgate.net/post/Inflammation_vs_...
- I looks up other stuff since it says tamoxifen enhances these, it seems like
Chemotaxis (from chemo- + taxis) is the movement of an organism in response to a chemical stimulus
phagocytosis is the process by which a cell - often a phagocyte or a protist - engulfs a solid particle to form an internal compartment known as a phagosome... Phagocytosis is involved in the acquisition of nutrients for some cells. The process is homologous to eating at the level of single-celled organisms; in multicellular animals, the process has been adapted to eliminate debris and pathogens.
Neutrophils are the most abundant type of granulocytes and the most abundant (40% to 70%) type of white blood cells in most mammals. They form an essential part of the innate immune system.
So this study seems to be saying that tamoxifen helps all these things, which actually helps the immune system be stronger!
The Effects of Tamoxifen on Immunity
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902982/
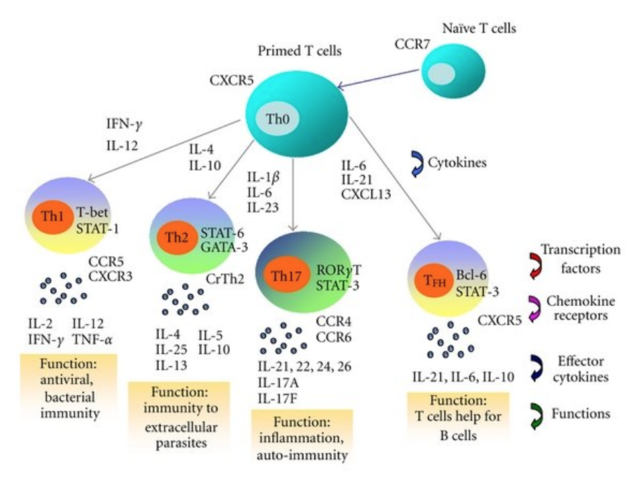
Says this... "We review the growing body of evidence which demonstrates immunomodulatory effects of tamoxifen, including in vitro and in vivo studies as well as observations made in breast cancer patients treated with tamoxifen. Taken together these studies suggest that tamoxifen is capable of inducing a shift from cellular (T-helper 1) to humoral (T-helper 2) immunity."
Which does say that tamoxifen can have a modulating effect on the immune system, but appears to be a good one, like it helps regulate the immune system...?
Then this is a little confusing though:
"First, tamoxifen may be utilized in the treatment of immune-mediated disorders, particularly of those arising from aberrant T-helper 1 cell activity, including allograft rejection, Crohn's disease, and Th1-mediated autoimmune conditions such as diabetes mellitus, scleroderma, and multiple sclerosis. Second, given that cellular T-helper 1 immunity is targeted against cancer cells, the tamoxifen-induced shift away from cellular immunity represents a significant step in fostering a cancerogenic environment. This may limit the anti-cancer effects of tamoxifen and thus explain why tamoxifen is inferior compared to other anti-estrogens in preventing disease recurrence in early-stage breast tumors."
So I read into the details, seemed to be saying that on the one hand, tamoxifen could help treat immune disorders and autoimmune conditions. However, then it says it might foster a cancerogenic environment because it moves from one type of immunity to another?
It sounds like all these articles are considering whether tamoxifen can also be used to help treat immune disorders. I don't know if any of this is reassuring to you or not, or maybe I mis-interpreted it. I honestly had to look up a lot of these terms to understand the articles LOL.
OK too much information for a Friday night, let's enjoy the weekend!
0 -
Hi Spoonie77,
In terms of absolute benefit (as opposed to relative benefit), most studies I have come across indicate 1-4% benefit for Tamoxifen. These benefits will vary depending on the underlying pathology of your BC. Most doctors I have engaged with during my treatment have quoted the relative benefits which can often be misleading to a layperson. I have just stopped taking Tamoxifen after almost two years due to Gyne issues (thickening of my uterus) and bad joint/bone pain. I am trying to establish whether my symptoms are in fact due to the Tamoxifen or resulting from the fact that chemo has pushed me into early menopause. If I find no relief from symptoms after stopping the Tamoxifen for 6 months, I may decide to go back on it, although I'm doubtful that it offers me much more than 2% benefit as my Allred score was 5 (4+1). I have read that as a rule, breast cancers do not respond to tamoxifen with an Allred score of < 6 or toletrozole with a score of < 3. It's not a decision I take lightly but like yourself, I want to consider the quality of life I have at present. There is no right or wrong way to go. You need to do what feels right for you.
Best Wishes
Emma
0 -
Thank you so much to all of you doing this thinking and researching 'out loud.' It's really useful for me and I assume others to be able to read and learn along side.
I started tamoxifen almost a month ago and so far haven't had any lasting side effects. But I was definitely frustrated that the docs were so focused on the relative benefit.
I almost got the impression that they're worried that if they discuss the more nuanced full picture and the details of side effects, that I would refuse to even try it.
But like Pebbles experience, the more respectful and honest and thoughtful they are with us, the easier it feels to trust them and try the treatments they recommend!
IMO there must be not nearly enough psychology and human relations training in medical school and professional development.
0 -
Hi Pebbles -- LOL how was your Friday night?


 My Saturday has been interesting! LOL.
My Saturday has been interesting! LOL. I like research though and information has always given me peace of mind, so this of course, became wayyyyyy longer than I intended. Learned ALOT along the way today. Pretty interesting how far and wide one drug can travel and leave its footprint as it were.
Here's what I took away from the articles and again, not knowing your health concerns, only mine, in your case some of those studies may be beneficial. Hooray if so! We can all use more good news! For me they spell bad news.
This is how I approached them...
1) Tamoxifen SLE Immune Study
https://ard.bmj.com/content/62/4/341
"Conclusion: The results clearly show the remarkable therapeutic effects of tamoxifen on SLE of (NZB×NZW)F1 female mice and suggest that these beneficial effects are related to the specific reduction of IgG3 autoantibodies."
------> Ok, so knowing this study shows Tamoxifen reduction in IgG3 antibodies, I asked myself what are these important for? Here's what they do...
"Antibodies are major components of humoral immunity. IgG is the main type of antibody found in blood and extracellular fluid, allowing it to control infection of body tissues. By binding many kinds of pathogens such as viruses, bacteria, and fungi, IgG protects the body from infection.
It does this through several mechanisms:
- IgG-mediated binding of pathogens causes their immobilization and binding together via agglutination; IgG coating of pathogen surfaces (known as opsonization) allows their recognition and ingestion by phagocytic immune cells leading to the elimination of the pathogen itself;
- IgG activates all the classical pathway of the complement system, a cascade of immune protein production that results in pathogen elimination;
- IgG also binds and neutralizes toxins;
- IgG also plays an important role in antibody-dependent cell-mediated cytotoxicity (ADCC) and intracellular antibody-mediated proteolysis, in which it binds to TRIM21 (the receptor with greatest affinity to IgG in humans) in order to direct marked virions to the proteasome in the cytosol;[2]
- IgG is also associated with type II and type III hypersensitivity reactions."
-----> Next I asked myself, what is SLE (systematic lupus) and how does that work on the immune system?
Answer: It's one of many disorders of the immune system known as autoimmune diseases. In autoimmune diseases, the immune system turns against parts of the body it is designed to protect. This leads to inflammation and damage to various body tissues.
------> Then, what is Thrombocytopenia?
"Although doctors don't know what causes ITP, they know that it happens when your immune system -- your body's main defense against disease -- doesn't work right. Your antibodies, which are supposed to attack infections, instead mistakenly destroy your platelets."
Ok, put it all together and I take it to mean that this study shows Tamoxifen decreases IgG3 antibodies in a person with an OVERACTIVE immune system, thereby reducing symptoms & resulting in decreased inflammation to tissues/organs/blood/etc by stopping said overactive antibodies from attacking the patients own self.
Super for anyone with that going on, right?

For me, that means, that my immune system, which is literally not on the map for many lab results, including iGg complements, would be further suppressed leading to a spread of the 4 chronic infections I fight. Bad for me.
2) Immunomodulatory Effects Of Anti-Estrogenic Drugs
https://www.ncbi.nlm.nih.gov/pubmed/22750814
and the article you linked was https://www.ncbi.nlm.nih.gov/pubmed/21089249
"In recent years, a growing body of evidence suggests that these drugs can also act as immune modulators by altering the function of various leukocytes and the release of different cytokines. Moreover, there is evidence that anti-estrogens may prove to be beneficial in the treatment or prevention of some autoimmune diseases due to their effects on immune function. "
You're right, Pebbles, in that these do help people with overactive immune systems. But the problem IMO is how it "helps" in the system, especially if you have ongoing infections. I have experience here, since I've been on "immune modulators" aka "biologics" for my Sero Neg Rheumatoid Arthritis.The short version is "Genetically engineered proteins originating from human genes, biologic drugs target specific parts of the immune system that fuel inflammation."
Here's the breakdown of what a biologic is and does and the down-regulating effects on the immune system....
https://www.arthritis.org/living-with-arthritis/treatments/medication/drug-types/biologics/drug-guide-biologics.php
The side-effects of these biologics/modulators lead to serious infections and lowered white blood cell counts because again, these drugs (modulators) are taken to reduce certain aspects of immune system activity, in order to stop it from incorrectly battling itself. Put these in a person that is not dealing with an autoimmune disease and their cell counts drop and they have an inability to fight off infections because of the suppression.
So this snippet, to me, is saying that Tamoxifen/Anti-Estros may help prevent auto-immune disease because of this "biologic" effect. Again, great if you have the disease in question, probably not so great if your immune system is struggling. I believe this is why the CDC lists Tamoxifen as an immunosuppressant on their Travelers Page and Vaccination Warnings list: "Some of these agents are less immunosuppressive than others, such as tamoxifen or trastuzumab given to breast cancer patients, but clinical data to support safety with live vaccines are lacking."
3) Tamoxifen Augments The Innate Immune Function
https://www.ncbi.nlm.nih.gov/pubmed/26458291
full article https://www.nature.com/articles/ncomms9369
This one is super techy/sciency. Ugggh. I think you are correct that it does boost a facet of immunity here. Mainly in producing NETs and increasing the levels of Ceramide. But Ceramide is a double-edged sword it appears.
So, maybe there are good things and bad things about increased NETs, increased levels of Ceramides.....the good it seems by inducing cell death and creating these NETs pathogen reactivity/bactericide is seen. Especially in regards to cancer cells. Good news! Sick em'!
Yet, the increased levels of Ceramides that Tamoxifen brings on to do this, seems to have three downfalls.
One, it may actually lead to drug resistance in the long run (science explanation down below ~5.3). Two, causes increased levels of Amyloid-β (Aβ) resulting in memory/brain fog/possibly even other diseases such as Alzheimer's'. Lastly three, "Ceramides impact the way the body handles nutrients and they impair the way the body responds to insulin, and also how it burns calories." (Buildup of Toxic Fat And Diabetes) "The resulting accumulation of byproducts of cellular metabolism (e.g., reactive oxygen species [ROS], ceramides, diacylglycerols, etc.) impairs function of peripheral tissues (e.g., heart, vasculature, etc.), giving rise to the panoply of defects that underlie diabetes and heart disease " (Adipocyte Ceramides Regulate Subcutaneous Adipose Browning, Inflammation, and Metabolism) (Association Of Tamoxifen Use and Increased Diabetes Among Women Diagnosed With Breast Cancer)
Maybe this is why many people taking Tamoxifen report brain fog and memory problems and weight gain??
IDK. The possibility doesn't seem out of this world after reading some of the science.
There are a few articles I read that helped me understand what's being talked about.
- Breast Cancer Drug Beats Superbug (layman explanation
 )
)https://www.sciencedaily.com/releases/2015/10/151013095402.htm
- Neutrophil extracellular traps (NETs): Double-edged swords of innate immunity
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3439169/
- ETosis: A Novel Cell Death Pathway
http://stke.sciencemag.org/content/1/21/pe25
- Ceramide
https://en.wikipedia.org/wiki/Ceramide
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4610010/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307283/
4.2.3. Ceramide
"Ceramide is capable of triggering apoptosis in almost any cell, including tumor cells.
Ceramide can be generated by a de novo pathway (ceramide synthase) or by sphingomyelinases in response to various stress stimuli, such as cytokines, heat shock, growth factors, vitamin D, TNF-α, CD95/Fas, chemotherapeutic agents, toxin, irradiation, UV-light, and infection by different signaling pathways [72]. Elevation of cellular ceramide levels directly or indirectly regulates the activities of a number of enzymes and signaling components, including MAP kinases, ceramide-activated kinase, ceramide-activating serine/threonine phosphatases such as protein phosphatase 1A and 2A, protein kinase C ζ, phospholipases such as phospholipase A2 or D, CPP32-like caspases, cathepsin D, transcription factors such as NF-κB, and kinase suppressor ras [117,118,119,120,121,122]. These enzymes and signaling components play an important role in the regulation of apoptotic signaling.
On the other hand, an irreversible step in apoptotic processing is mitochondrial outer membrane permeabilization which releases critical proteins such as cytochrome c. The channels for protein release are controlled by Bcl-2 family proteins based on cell physiological function: anti-apoptotic proteins (Bcl-x, Bcl-w, and others) destabilize the channels whereas pro-apoptotic proteins (Bax, BAD, Bak, Bok, and others) act synergistically with ceramide to increase membrane permeability [123]. Ceramide can self-assemble in the mitochondrial outer membrane to form large stable channels capable of releasing cytochrome c [124].
Cytochrome c further interacts with Apaf-1, activates several caspases and forces cell to undergo apoptosis. The role of ceramide in apoptosis indicates that ceramide could be a potential anticancer drug."
5.3. Lipid Metabolism and Drug Resistance
"In spite of many significant progresses in cancer therapy, cancer is still a major disease that causes more than 8 million deaths, or about 15% of all human deaths around the world every year because most cancer patients eventually develop drug resistance [172]. Drug resistance of cancer cells represents a serious barrier to successful clinic treatment, and inherent drug resistance of cancer cells is caused by multiple mechanisms.
The molecular mechanisms of drug resistance can be caused by gene mutations which can enzymatically deactivate the drug, alter the drug-specific binding site, decrease drug permeability and/or increase active efflux (pumping out) of the drugs across plasma membrane, and/or change of the metabolic pathway to yield different non-cytotoxic products. Many of these processes are associated with the alteration of lipid metabolism. Ceramide is a center of sphingolipid metabolism, and more than eleven different enzymes use ceramide as a substrate (ceramidase, ceramide kinase, glycosylceramide synthase, galactosylceramide synthase, and sphingomyelin synthase) or directly convert other molecules to ceramide (dihydroceramide desaturase, sphingomyelinase, ceramide-1-phosphate phosphatase, glucocerebrosidase, galactocerebrosidase, and ceramide synthase) [75,163].
One of the best examples of how changing metabolic pathways may lead cancer cell to drug resistance is that ceramide-generating cancer chemotherapeutic drugs impact the accumulation of ceramide [163] and the increased levels of cellular ceramide drives cancer cell death [73]. Accumulation of cellular ceramide also activates glucosylceramide synthase which converts ceramide to glucosylceramide, thereby reducing ceramide levels in the cells [75]. Glucosylceramide has been demonstrated to stimulate cell growth and DNA synthesis which drive cancer cell resistance to chemotherapy [173]. Other ceramide derivatives such as ceramide-1-phosphate and sphingosine-1-phosphate also regulate cell survival and proliferation pathways, and could lead to drug resistance, as well [161]."
- Ceramides in Alzheimer's Disease: Key Mediators of Neuronal Apoptosis Induced by Oxidative Stress and AβAccumulation
"Alzheimer's disease (AD), the most common chronic and progressive neurodegenerative disorder, is characterized by extracellular deposits of amyloid β-peptides (Aβ) and intracellular deposits of hyperphosphorylated tau protein. Ceramides, the major molecules of sphingolipid metabolism and lipid second messengers, have been associated with AD progression and pathology via Aβ generation. Enhanced levels of ceramides directly increase Aβ through stabilization of β-secretase, the key enzyme in the amyloidogenic processing of Aβ precursor protein (APP). "
- Amyloid-β (Aβ)
https://www.alzforum.org/alzpedia/amyloid-v-av
"Excess amounts of Aβ can induce a variety of pathologic processes. Aβ can impair neuronal and glial function, synaptic physiology, neurotransmission, and cognition. Evidence points to transcellular spread and templated seeding, and the resulting deposition of aggregated Aβ into extra-neuronal amyloid plaques is a pathological hallmark of AD."
4) The Effects of Tamoxifen on Immunity
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902982/
------
Important things to know...
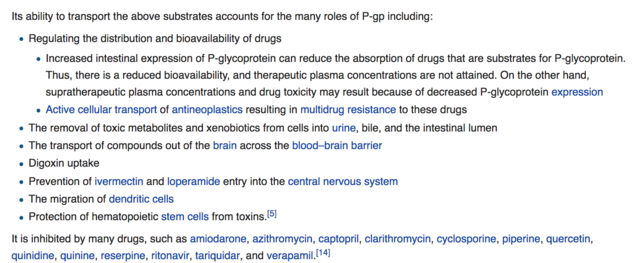
"Estrogen agonism and antagonism give rise to a variety of beneficial and adverse effects including: protection of osteoporotic bone, postmenopausal symptoms, an increased risk of endometrial cancer, thromboembolism, and strokes [5,6]. In addition to its action on the ER, tamoxifen is an inhibitor of P-glycoprotein, a 170-kDa protein located both within the cell membrane and in the cytosol [10]. P-glycoprotein is a member of the ATP-binding cassette superfamily of active transporters [11], and it has been proposed that tamoxifen inhibits P-glycoprotein through interference with its ATPase activity [12]. Traditionally associated with multi-drug resistance of certain mammalian solid tumors and hematological malignancies, a role for P-glycoprotein in immunity has recently emerged [13]. Its (P-GP) function in various immune cells has been demonstrated, including lymphocytes and dendritic cells [14–17]. The role of P-glycoprotein in immunity is particularly interesting for the present discussion because P-glycoprotein inhibition may account for some of the effects of tamoxifen on immunity."
What is P-Glycoprotein and what does it do? https://en.wikipedia.org/wiki/P-glycoprotein
"An important protein of the cell membrane that pumps many foreign substances out of cells. More formally, it is an ATP-dependent efflux pump with broad substrate specificity.
P-gp is expressed primarily in certain cell types in the liver, pancreas, kidney, colon, and jejunum.[11] P-gp is also found in brain capillary endothelial cells.[12]
P-gp is extensively distributed and expressed in the intestinal epithelium where it pumps xenobiotics (such as toxins or drugs) back into the intestinal lumen, in liver cells where it pumps them into bile ducts, in the cells of the proximal tubule of the kidney where it pumps them into urinary filtrate (in the proximal tubule), and in the capillary endothelial cells composing the blood–brain barrier and blood-testis barrier, where it pumps them back into the capillaries.
The protein belongs to the superfamily of ATP-binding cassette (ABC) transporters. ABC proteins transport various molecules across extra- and intra-cellular membranes. ABC genes are divided into seven distinct subfamilies (ABC1, MDR/TAP, MRP, ALD, OABP, GCN20, White). This protein is a member of the MDR/TAP subfamily. Members of the MDR/TAP subfamily are involved in multidrug resistance. P-gp is an ATP-dependent drug efflux pump for xenobiotic compounds with broad substrate specificity. It is responsible for decreased drug accumulation in multidrug-resistant cells and often mediates the development of resistance to anticancer drugs. This protein also functions as a transporter in the blood–brain barrier. "
+++ Basically, my understanding is that PGP transports "substrates" aka medicines/toxins/etc throughout various tissues/organs/brain/etc through the cell membranes. It also has the function to be able to cross the blood brain barrier. For some reason I'm not exactly clear on here on the molecular process, but Tamoxifen inhibits the activity of this protein, which is important in battling cancer, in that PGP activity decreases the intracellular concentration of cancer drugs, enabling resistance to develop to them. +++
https://academic.oup.com/cid/article/32/1/76/311106
"Like glucocorticoids, estrogens and progestins have been shown to suppress type 1 immunity in favor of type 2 immunity. Both estrogens and progestins inhibit IL-12 and IFN-γ secretion from antigen-presenting cells and T cells, while stimulating IL-4, IL-10, and IL-13 secretion [ 137–139 ]. "
P-glycoprotein and T-cell activationhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121004/
"Thus, recent investigations have challenged earlier notions that P-gp functions as an IL-2 transporter in human T-cells, but instead indicate that P-gp serves a regulatory role in T-cell survival, and hence possibly in the selection of an appropriate lymphocytic repertoire in the course of immune activation. Altered cytokine expression profiles, such as have been observed under conditions of P-gp blockade by many investigators, may in this regard reflect phenotypic differences in the selected T-cell repertoire, rather than resulting from inhibition of P-gp-mediated transport. ""In our studies, we found that the pharmacological P-gp inhibitor tamoxifen and the MDR1 P-gp-specific mAb Hyb-241 blocked alloantigen-dependent IL-2, IFN-γ and TNF-α production and T-cell proliferation in the mixed lymphocyte reaction (MLR). ""In addition, selective P-gp inhibition on CD4+ T-cells diminished IL-12 production by allogeneic APCs, suggesting that T-cellular P-gp blockade dysregulated the IFN-γ/IL-12 positive feedback loop and, as a result, T-cell differentiation into IL-2/TNF-α-producing Th1 cells. "
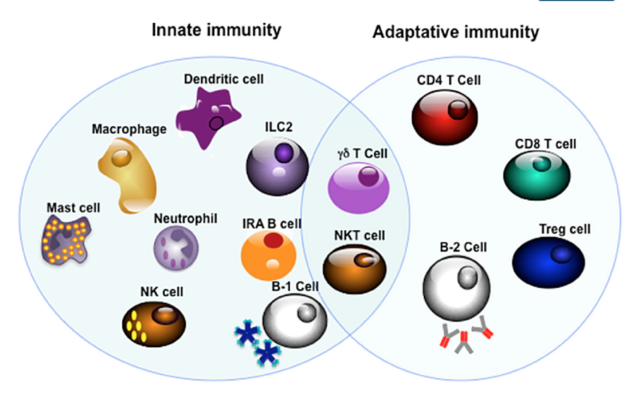
The main article goes on to say that "P-glycoprotein inhibition induced a shift from Th1 to Th2 activity in vitro."So now secondly, what are T1 & T2 cells and what are their jobs? (very oversimplified)T1 cells lead to an increased cell-mediated response, typically against intracellular bacteria and protozoa.
T2 cells lead to a humoral immune response, typically against extracellular parasites.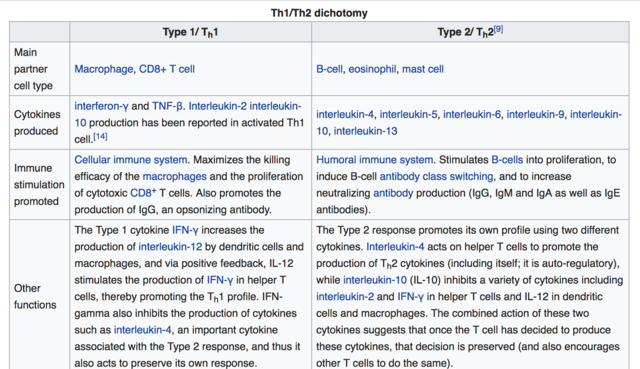
----- So what does this mumbojumbo mean and do we need PGP for our immune system to function correctly?
It's very very complicated.....UGGH. I honestly don't know in regards to the PGP. I've been reading and there seem to be differing opinions and thoughts. You're guess is as good as mine at this point! Suffice it to say there aer so many roles T Cells, Lymphocytes, PGP, and the rest all play in our immunity. Best to talk it all over with a doctor you trust and who is willing to listen and take a look if your immune system and/or medical history is more complicated than the Average Jo/Joe.
Suffice it to say there aer so many roles T Cells, Lymphocytes, PGP, and the rest all play in our immunity. Best to talk it all over with a doctor you trust and who is willing to listen and take a look if your immune system and/or medical history is more complicated than the Average Jo/Joe.  0
0 -
I'm just going to add this link, it goes to a thread where a member posted her experience with Tamoxifen.
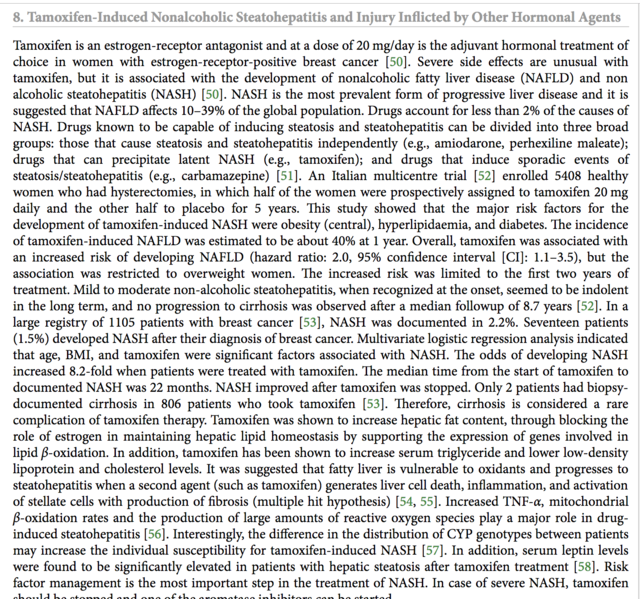
I feel like anyone deciding on this hormone treatment should be aware of possible damage and risk to their liver, as I was never made aware of this by my MO or team. There is a 30-40% risk of developing NAFLD (non-alcoholic fatty liver disease) due to Tamoxifen.
Please, as her story illustrates, at the very least, before starting Tamoxifen, insist on having a liver enzyme test run.
Better safe than sorry and needing a liver transplant because of the damage!
(Reference post is written by CanadaLiz on 12/15/2018)
https://community.breastcancer.org/forum/78/topics/868854?page=1#idx_29
(symptoms and Studies listed below)
I am utterly staggered by the studies that show the impact Tamoxifen has on the liver and the very direct statements made in them that EVERYONE should be clinically advised and monitored regarding their liver, as a baseline, and every 4 months thereafter due to its toxicity to the Liver.
Especially of note (mentioned in several studies) are pre-menopausal women with & w/o concurrent depression, apparently of higher risk of developing NAFLD.
Yet, it seems to me, no one has really been told this or been tested for this?
---------(cross posted)
Symptoms to be aware of:
https://www.breastcancer.org/treatment/side_effects/liver_probs
Here are a few studies for info:
A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462391/
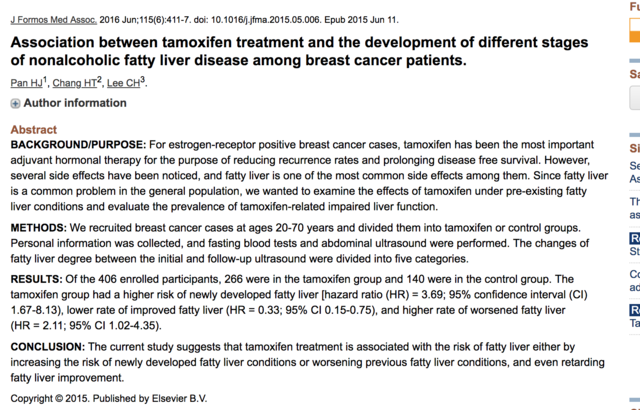
"In addition, fatty liver disease, also known as non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH), was observed in more than 30% of patients with breast cancer who received tamoxifen as adjuvant therapy.10,11 The first anastrozole-induced hepatotoxicity case was reported in 2006.12 A retrospective study demonstrated that fatty liver disease detected using ultrasound was more frequently seen with tamoxifen than with anastrozole (30.4% vs 6.25%).13 "Association between tamoxifen treatment and the development of different stages of nonalcoholic fatty liver disease
https://www.ncbi.nlm.nih.gov/pubmed/26071793
https://www.sciencedirect.com/science/article/pii/S092966461500176X
"Several studies showed that taking tamoxifen may incur a 30–40% risk of developing nonalcoholic fatty liver disease(NAFLD), according to different diagnosis instruments."ConclusionThe current study suggests that tamoxifen treatment is associated with the risk of fatty liver either by increasing the risk of newly developed fatty liver conditions or worsening previous fatty liver conditions, and even retarding fatty liver improvement."
"Our study suggests that tamoxifen is associated with the risk of NAFLD development, either by increasing the developed fatty liver or worsening the previous fatty liver condition and even retarding fatty liver improvement. The severity of fatty liver is associated with higher rates of abnormal LFT. During the follow-up period, regular abdominal ultrasound checkup, not just for detecting liver nodules, but also for identifying fatty liver change, is crucial. Further checking of liver function and other metabolic conditions once the fatty liver condition has progressed is essential."
Drug Record: Tamoxifen
https://livertox.nih.gov/Tamoxifen.htm
"Outcome and ManagementWhile fatty liver arises in at least one third of women treated with tamoxifen for up to 5 years, clinically significant steatohepatitis is less common. Nevertheless, monitoring of serum aminotransferase levels during tamoxifen therapy is appropriate. In women with persistent elevations in ALT levels, the relative benefits and risks of continuing tamoxifen therapy must be weighed. Factors to help in the decision, include noninvasive tests for hepatic fibrosis (platelet count), imaging of the liver and, in some instances, liver biopsy. Other approaches short of stopping tamoxifen therapy include nutritional advice and weight loss, abstinence from alcohol, and possibly medical therapies for nonalcoholic steatohepatitis (which are currently investigational and have not been shown to be specifically helpful in tamoxifen induced fatty liver). The possible development of serious hepatic fibrosis and portal hypertension can be assessed noninvasively by serial determinations of platelet count, but may require liver biopsy to document."
Tamoxifen induces hepatotoxicity and changes to hepatocyte morphology
https://www.spandidos-publications.com/10.3892/br.2015.536
"Clinically, patients who accept the endocrinotherapy are instructed to reexamine their liver function every 4 months due to its hepatotoxicity. Numerous research and clinical studies have illustrated clearly that TAM causes the inhibition of mitochondrial β-oxidation and subsequently leads to macrovacuolar steatosis (21,22). The early symptoms were characterized by the presence of a single, large lipid vacuole within the cytoplasm of the hepatocytes (23)."
"In conclusion, the present data showed that a relatively low concentration of TAM (6 mg/kg/day) for a short time treatment (2 weeks) would cause hepatotoxicity and change morphology at the microscopic and ultrastructural levels. Although the liver function may compensate or reverse the injuries gradually, the damage that occurred in the short-term TAM therapy has been shown. Thus, there is a necessity to obtain measures for monitoring liver function and protection at the early stage of the TAM endocrinotherapy, prior to apparent and undesirable clinical symptoms occurring. Furthermore, as DNA damage also occurs at this early period without clear clinical symptoms, which in the long-run increases the risk of hepatocarcinoma, exploring alternatives for TAM in long-term clinical endocrinotherapy is required."
Liver Injury Induced by Anticancer Chemotherapy and Radiation Therapy
https://www.hindawi.com/journals/ijh/2013/815105/
Death due to liver failure during endocrine therapy for premenopausal breast cancerhttps://www.tandfonline.com/doi/full/10.3109/0284186X.2010.484813
"In the tamoxifen product information, liver-related side effects are listed and it is recommended to perform periodic liver function tests, although in clinical practice blood tests are no longer performed routinely during follow-up for women with early breast cancer."
"Young women, in particular between ages 26 to 35, seem to be—for yet unknown reasons—more frequently affected by acute liver failure, and the use of antidepressants (metabolized primarily via liver enzymes CYP 3A4, 2D6, 2C19), other potentially hepatotoxic drugs (e.g. acetaminophen-type analgesics and NSAIDs), and alcohol are more frequent in younger breast cancer patients than generally presumed and reported. We therefore advise physicians to pay special attention to patients treated with endocrine therapy for breast cancer who have concurrent depression and who potentially or actively consume hepatotoxic drugs and alcohol. Such patients should have their liver function monitored and liver imaging should be performed if indicated."
The Association of Nonalcoholic Steatohepatitis and Tamoxifen in Patients With Breast Cancer
https://onlinelibrary.wiley.com/doi/pdf/10.1002/cncr.24374
A prospective, randomized study on hepatotoxicity of anastrozole compared with tamoxifen in women with breast cancer
https://pdfs.semanticscholar.org/3aa1/d236d38c20f3a9377dea6f9d5ad8235221c6.pdf
G.L.O.W.N. - Tamoxifen
https://www.glowm.com/resources/glowm/cd/pages/drugs/t002.html
"Effects on lab test results
• May increase BUN, calcium, and liver enzyme levels.
• May decrease WBC and platelet counts.Special considerations
• Tamoxifen acts as an antiestrogen. Best results occur in patients with positive estrogen receptors.
• Adverse reactions are usually minor and well tolerated. They usually can be controlled by dose reduction. ALERT Serious, life-threatening, or fatal events associated with tamoxifen in the risk reduction setting include endometrial cancer, uterine sarcoma, stroke, and pulmonary embolism.
ALERT Serious, life-threatening, or fatal events associated with tamoxifen in the risk reduction setting include endometrial cancer, uterine sarcoma, stroke, and pulmonary embolism.  ALERT Discuss the potential benefits versus the potential risks with women considering treatment to reduce their risk of developing breast cancer. Benefits of therapy outweigh risks in women diagnosed with breast cancer.
ALERT Discuss the potential benefits versus the potential risks with women considering treatment to reduce their risk of developing breast cancer. Benefits of therapy outweigh risks in women diagnosed with breast cancer.
• Clotting factor abnormalities may occur with prolonged tamoxifen therapy at usual doses.
• Variations on karyopyknotic index in vaginal smears and various degrees of estrogen effect on Papanicolaou smears have been seen in some postmenopausal patients. May increase serum thyroxine concentrations and may be explained by increases in thyroxine-binding globulin.
• Initial adverse reactions (increased bone pain) may be a sign of good tumor response shortly after starting tamoxifen therapy.
• Monitor WBC count, platelet count, and periodic liver function tests results.
• Monitor serum calcium levels; hypercalcemia may occur early in therapy in patients with bone metastases."0 -
Hi everyone-
This is my first post, so forgive me if it is in the wrong spot. I'm also having a hard time with starting Tamoxifen. I have to wonder why the rx and dose seem to me the same for everyone? My IDC tumor was less than 2 mm and my oncotype was a 3.
I was supposed to start today, but didn't. I'm flying this weekend and would rather wait until after the new year. I don't want to worry about blood clots during my flights and don't want to deal with possible side effects during my trip.Could delaying my start be problematic?
I've cried before starting each treatment - surgery, freezing my eggs, radiation, and now this. I guess it's the new normal.
Thanks for listening!
0 -
Hi MPND, and welcome to Breastcancer.org,
We're so very sorry to hear you're having such an emotional time with your treatment, but we can assure you there are many others here who are struggling as well -- and many others who will tell you that it will get better! Not everyone experiences extreme side effects of tamoxifen, and it just might not be as bad as you think. Have you talked to your doctors about your concerns and the potential drawbacks of delaying treatment?
We're all here for you! We look forward to supporting you more. Come back often and ask as many questions as you'd like!
--The Mods
0 -
Hey MPND,
I think those are great questions and I see them coming up regularly here.
My non-expert guess is that the burden of proof for showing that different, especially lower doses would be equally effective is quite high and difficult to meet because it requires following women for such a long period of time (the tricky thing with the ER+ breast cancer is that you are trying to control for risks 10+ and 20+ years out) and purposely putting some women on a dose without clinical proof of efficacy, which may make it challenging to design studies that pass ethics reviews. I guess there isn't enough motivation for risk adverse practitioners to try to mess with something that seems to work.
OTOH, now there are studies coming out that show how poor compliance rates actually are, and I hope that will light a fire under some butts to do further research. So far I think they are only promoting lower dose tamoxifen for women at risk fo cancer who wouldn't have taken any at all before, not for women who have already had a diagnosis.
I think it's a huge problem across the medical field that generally women's reports of symptoms, experiences, and side effects, and pain, aren't taken seriously enough.
That is a lovely low oncotype score and such a tiny tumor. I think it makes sense for you to speak with your doc and maybe a second opinion about your personal risk profile and trying to make an educated guess about the impact of a lower dose for you personally. I wouldn't expect any doctor to actually recommend or officially approve of a lower dose for you because there are well documented/supported standards of care, but they should support you making a decision for yourself.
It is also very reasonable to reach out to them with your questions about traveling, either delaying starting or skipping certain doses to minimize blood clot risks.
That said, it really is the case that plenty of women don't have quality of life impactful side effects on the standard dose of tamoxifen, and that the only way to know the impact on you personally is to try it.
This illness feels like a mental/emotional challenge as much as a physical one. I think tears with every new stage of treatment makes sense, and can be a sign of healthy emotional processing. Wishing you peace and strength and happy travels!
0 -
Following this thread.... I too am considering refusing Tamoxifen .. and chemo.
In my case I'm 38, stats almost identical to yours, minus the dcis. I've had a dbl mx already. Had a followup Pet scan on Monday & received results today that shows NED from head to toe.
So why do I need further treatment... to prevent recurrence? Yet I see ladies on this board who still had a recurrence with chemo and/or hormone therapy. Sometimes the cancer returns with a vengeance. & I've also read the SEs from Tamoxifen include other cancers.. wait, what?! .. seems my risk is the same either way I choose. Why expose myself to more? ...i'm with you Spoonie.
0 -
Hey y’all! I posted this in another hormone site-but it seems to fit here! Goodbye Tamoxifen

I started tamoxifen on 12/10 and just stopped on 12/26-due to my side effects. The Onco said to stop taking it until they see me-on 1/24. I've always been a healthy person...hiking, running, boot camp classes-lots of fruits and veggies. I've had a high tolerance for pain and I'm not a complainer
 I like to go with the flow in life.
I like to go with the flow in life.This is just what happened to ME on tamoxifen and obviously we all have such different journeys 💕:
About 5 days after starting it I had some minor SE's (headache, hot flashes/night sweats, itchy, dry eyes). But my NECK and back felt like a steel board that I couldn't move-I could barely turn my head the tiniest bit. I called the Onco and they said try and stay on it for two weeks-it should get better. I kept taking it and I DID get better by two weeks. Just a tiny tightness in my neck, on the right side.
I hate to say it- but on 12/26-out of the blue-my neck/back pain came back worse than it was before. Super extreme pain. It hurts to walk, and I can barely turn my head-I'm in bed with a heating pad right now. Even though I stopped two days ago-my neck and back still have shooting pains and are really tight (seized up kind of tight).
I'm hoping with lots of water and heat-this pain will go away by today or tomorrow? I'm interested to see what the next steps will be-but I won't be returning to tamoxifen. It’s been worse than post surgery AND drain tubes! I'm 47, just for reference.
I wish you strength and luck...Sorry for the long post!
0 -
Hi Oya and SugarMaple - thanks for sharing your experiences and journeys. This battle is so difficult, on SOOO many fronts, all we can do is make the best choices we can live with going forward. Totally respect where you are both at.
What's next SugarMaple? Do you see your MO soon and figure out an alternative?
Oya, I hear ya. Even if we do everything our MO's ask, there is never a guarantee that we got it in time or that it won't come back. Case in point, the link below. Not to scare anyone, but just to inform and make aware, I share this link...
Wish more docs would be open about this fact, but seems they are not. This is why I am pushing so hard to have baselines established and dot/cross all my i's and t's.
Research Worth Watching: Overview from San Antonio 2018
https://www.drsusanloveresearch.org/blogs/research-worth-watching-overview-san-antonio-2018
"As a surgeon, I was struck by the fact that the role of surgery and the value of mastectomy in breast cancer treatment has significantly diminished. There are several drivers of this shift but the key is the change in our understanding of the disease and its progression. When I started as a breast surgeon, we believed that after a cancer started growing in the breast, it slowly moved from one lymph node to another and then, after invading all the nodes, went into the blood stream, where it traveled to other parts of the body. We thought if we got there soon enough, and did a big enough surgery, we could slam the door before the migration to the nodes and blood stream began.
Now we understand that most, if not all, breast cancers have sent cells out into the blood stream way before we are able to diagnose the disease. Up to 40 percent of breast cancer patients have detectable disseminated tumor cells already in their bone marrow at the time of diagnosis. The fact that we can find these circulating tumor cells (CTCs) in the blood or disseminated tumor cells(DTCs) in the bone marrow at the time a person is first diagnosed with an early-stage breast cancer shows that what we have termed early detection is not really very early."
0 -
Hey Spoonie!
I’m supposed to meet with my MO on 1/24. She said just hold off the tamoxifen and we’ll discuss then. I’m not really sure what’s going to happen. I also have an MRI scheduled for my right breast on 1/30...so if something’s changed there-who knows...my alternative may be removing that breast too. I’m just living in the moment
I hope we all have some beautiful moments this year-sending everyone peace and love!
0 -
Hi Spoonie,
I'm older than you, 55 now. I was diagnosed at 54 last February. I had a lumpectomy and radiation. My oncotype was 27, considered high by my MO and she put me in the "young" range when considering my treatment. I declined chemo and I have also, at least so far, declined Tamoxifen. I have the same concerns as you. I am also single and no kids and that makes a big difference for those of us struggling with this decision.
I just wanted to chime in since I'm still on the fence myself with this one. And, to let you know you are not alone. I battle my doctors everytime I see them on this issue. I know I should take it, but I just can't bring myself to do so. My family has strokes. Stroke is a possible side effect of tamoxifen. Then, they say AI instead, well, in my 30s, I was always in pain from constant joint pain. I have no idea why and it subsided around age 40. I feel better today than I have in my entire life and I don't want to take a drug to mess that up.
Also, I thought I had gone through menopause. No periods for 3 years now. Some hot flashes, but nothing awful. Not even sure if that's what it was. I figured I had sailed through. FouND out I'm not totally through menopause yet. But, I can tell you, at age 50, people thought I was in my 40s. I looked young. At 52, things changed drastically. That's natural menopause. I can't imagine speeding this aging thing up even more.
So, good luck with your decision. But I hear you and understand your stance.
0
