Starting/declining hormone therapy Nov, Dec, Jan 2018
Comments
-
 Spoonie, good to hear from you but we are here for you! So don't be shy! I too have also hi jacked as I can't be on them either, so I don't think that's the criteria!
Spoonie, good to hear from you but we are here for you! So don't be shy! I too have also hi jacked as I can't be on them either, so I don't think that's the criteria!In my world got out of hospital yesterday for the hysterectomy. Slowly recovering, praying for good pathology. But a big Ray of sunshine I had a good mammogram and ultrasound!
Love those pups!
We got to dog sit the new boy, he's all grown up!
0 -
I'm feeling all frustrated because I can't get my oncologist and surgeon appointments on the same day - it's just impossible. And the surgery NP doesn't have any evening hours. So it looks like I have to take at least two half days off of work.
I have sick time but apparently they look at your use of sick time days when they're deciding about making you permanent, and I'm in an important time window for that.
0 -
Spoonie and Bennybear, this thread is for women starting OR DECLINING hormone therapy, whether you are declining by choice or not. We started out in similar situations, even if many of us have taken different paths. No one’s voting you off the island!
Bennybear, what a gorgeous dog! My husband and I had to put our dog to sleep right after Christmas. We’re not ready for another dog yet, but have had an opportunity to dog sit, which has been very therapeutic.
Salamandra, it’s good to hear from you! So frustrating that you have to take that much time off from work.
I’m doing well, just trying to kick a bad cold. Coronavirus news is making me nervous. I’m trying hard to be calm and realistic. And washing my hands ALL THE TIME. Sending virtual hugs to you all!!
0 -
Good point Green Harbor, but I just feel guilty posting SOOO much about my own issues here. It's alot. LOL. But I PROMISE I will still post here too.

Bennybear that's a handsome puppers!! Pets are just the best, so much unconditional love. Even in small babysitting doses, their snuggles have a lasting effect! Congrats on the clear scans. Glad surgery went smoothly. I'm wishing you a super recovery without issues. Do you have an idea of when you'll hear about Pathology results??? You are in my thoughts.
Salamandra, I'm with you on the scheduling issues. Many of these drs have booked schedules and it's a jigsaw puzzle of sorts to try to get them scheduled in the same week let alone same day. I'm sorry you have to use time off, especially when you are looking for more stability in your job position. Eeek. Hopefully they will be understanding and not hold it against you. How are you fairing on the Tamoxifen? Did you ever find one that worked decently for you? I know you were having so much trouble for months.
Oh.....so here is some good news that I totally forgot to share. My mom, being a mom, was stubborn and surprised me with a kitten a few weeks after Ari went to the Rainbow Bridge. I wanted to be upset but who wouldn't fall in love with this face????
So please, meet Raya.
She's a Ragamuffin baby girl. When she arrived she was 3 lbs 15 weeks old. Just a ball of fur. Her and Gypsy act like sisters and play so well together. It's all so lovely. Ms Rayay got her name because she is silver and white, but dappled on her back. The patterning reminded me of how light in a forest filters down through the canopy onto the forest floor. She is a Ray Of Light, Love, Healing....so Raya.

I love her to pieces. Her and Gypsy give me so much joy and love. They are priceless.







This one should have a caption....."MooooooMmmmmmmmm, Gypsy won't share!!!!!!"



 0
0 -
Oh my goodness, I am SWOONING over your kitten! So gorgeous and yay Spoonie-mom for doing that!
(IMO loving another cat is the best way to honor Ari, says you loved your kitty so much that you have more to give.)
0 -
Spoonie, that kitty face! So adorable!
I never got tamoxifen to work for me but my MO was finally willing to let me try toremifene instead, and so far that's going fine. She was worried my insurance wouldn't cover it but maybe they were satisfied by all my tamoxifen attempts.
It's a huge relief.
I hope you feel better soon! I keep thinking I'm coming down with something but so far have been ok. I'm sure the stress about Corona virus doesn't help.
0 -
wow spoonie, Raya is a sweetie! And I have never had a cat, husband with allergies. Good for your mom! Of course Ari will never be replaced but you have a lot of love to give and receive from Raya. Our pup also a replacement for an irreplaceable treasure, but he is own guy and we have fallen in love too!
Thanks green harbour! We're all in it together also bound by a love of animals!
0 -
In 2017, I refused Tamoxifen. While I have changed so my diet dramatically and many lifestyle changes, I still worry about it. Recently, I met a woman whose mother is a 22 year stage II survivor. I don’t know for sure if she took Tamoxifen, I assume she did. She also changed her diet to plant-based during chemo, and does so well. Is it crazy to start it so late? I see the MO in April and I can ask. Just wondering if anyone has heard of women waiting so long to start.
0 -
GoKale4320 I'm curious to know what your MO says about a plant-based diet, and whether it's specifically recommended. In my "Survivorship Training" from my MO clinic, they said that although eliminating meat does somewhat lower the incidence of colon and stomach cancers, they did not see conclusive data about that diet improving breast cancer outcomes or reducing recurrence rates. They did urge low sugar, limit fats/trans fats, eliminate simple carbs, limit alcohol 0-2 drinks per week, and eat nutritiously with lots of fiber and a wide array of vegetables and fruits, etc. Also regular exercise, and not be overweight. I'm doing okay on my AI. Some creakiness, but I've stayed comfortable with regular exercise.
0 -
Hiking Lady - it’s encouraging to know that you are doing well on the AI. I have a bone density scan tomorrow so it will be interesting to see those results, but I have a family history of osteoporosis so if I were to take anything it would probably be tamoxifen.
I made my decision to go plant-based from reading The China Study, ElynJacobs.com and her article about alternatives to Tamoxifen, and from watching Forks Over Knives. Animal products contribute inflammation in the body and add estrogen. Cutting out meat, dairy, fish etc I am hoping to also reduce my cholesterol.
My MO just shrugged his shoulder when I explained my new diet. His opinion is that drugs are the best (and only ) chance to avoid recurrence . So no, he doesn’t support plant-based diets. But nutrition is not emphasized in medical school.
0 -
GoKale,
That is an interesting question about starting tamoxifen years after treatment. I would love to hear what your oncologist says. I know that they now prescribe prophylactic tamoxifen to women considered at high risk for breast cancer, to it seems to me like it could be a good option and not crazy at all. Having had prior breast cancer, most of us are considered at high risk by default.
0 -
Hey ladies...I need help. I'm falling apart today. I just can't handle this continuing stress iwth drs.
 Any words of advice?
Any words of advice?Also, Salamandra that is super good news that you found a med that is working! Happy for you. Truly. Fingers crossed it stays that way for the rest of the time you need therapy.
BennyBear -- any word yet about the pathology? HOping for the best possible news for you.
Thanks all for the love for Raya. I'm holding her close today and her furr and purrs is giving me much needed love
-------
Help....
The disaster with my current MO continues.
I sent a portal msg this weekend asking after info about why/how my recurrence rate had somehow changed from her assessment of 25-30% from our prior visit in Sept 2019, to now as MO stated "nothing to worry about". (read above posts for the horror that appt was IMO) FWIW, when is CANCER HX ever NOTHING to worry about? UGGGh.
MO was out of office until today. Her nurse replied the following:
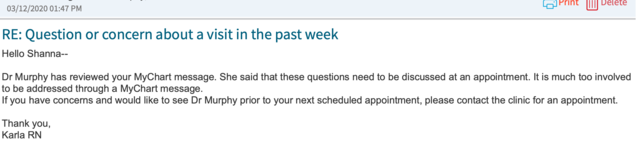
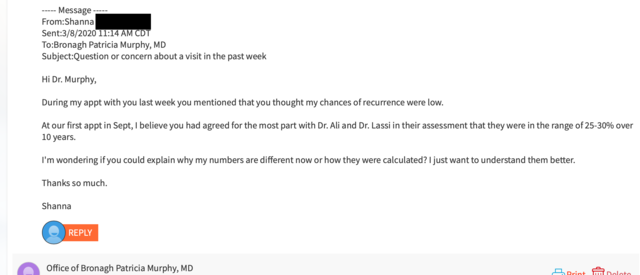
I cannot get in for an appt to discuss this until Aug. I don't get it. What am I supposed to do between then and now?
I called her nurse to see if I could get in sooner or if MO could portal msg me. She said she would ask but it is doubtful since her response was "It's too complicated to address via msg.". Honestly I call BS on MO. Prior drs have explained MUCH more intense info dense topics with me, if they choose. I feel like she is CHOOSING and it hurts my care as a patient. IDK. Maybe off base but sure doesn't feel like it.
I am falling apart. I think drs don't want to deal with me because I have too many health issues and I ask questions.
She has refused to order my CA 27-29 and my CEA markers, stating that "She does not order these for breast cancer patients."
Anyone else have these issues with the MOs? Or am I the only one??????
Losing my mind and for today I want to give up and quit fighting and just let the drs pass me off and let whatever happens, happen.
I fucking hate this. Sorry. I just continue to feel so belittle for having a disability and having cancer, drs just don't understand.
I'm heartbroken today.
0 -
I'm so sorry Spoonie, that sucks!
I think there are lots of relatively mediocre doctors out there, and it's super frustrating to run into this. To me, waiting until August for an appointment would not be okay. If she feels like it needs to be a conversation, she could also telephone you.
It is frustrating to feel so disempowered. Actually it's past frustrating and into terrifying and infuriating.
0 -
Ack August? That's a really long time away. Will you be able to see the new MO before then?
0 -
Spoonie, that makes no sense to me that you can’t get an appt until August. They wouldn’t ask a new patient to wait that long. I made this offer when you were seeing your previous MO, and it still stands... I will happily drive there and kick them in the shins for you. Sending love, and wishing I could do more.
0 -
My MO phoned me personally during difficult things, like giving me the news that I had #2 breast cancer, and he has always been responsive to my questions. Another way to view this, though, might be that truly, you can relax a bit, and your MO has re-assessed the risks and has this better news for you, and GREAT, take it! It's weird that you can't discuss this with her, though....In my clinic, a PA handled such phone conversations, and if I ask for something to be explained, they do it. I am sorry for your clinic's lack of responsiveness.
As far as tests for markers, some of that truly is NCCN guideline protocols; my MO has spent a good amount of time explaining how and when and why they order tests. The protocols that I've had explained to me have always been backed up by tons of data, and they were acceptable, once I understood them.
0 -
No appts available until Aug?!? That’s ridiculous! It seems like at least a phone call would be offered. I’m so, so sorry.
0 -
Spoonie, can you get in to see a nurse practitioner? You could also see another oncologist. I just saw a second one at the 5 year mark. Attime of diagnosis I saw three.
None of my docs do the tests you want.
Did you have an Oncotype test done? You can also get a Breast Cancer Index.
In fact, to go back to the original topic on this thread, when I got my Breast Cancer Index, they told me that I do not benefit from continued aromatase inhibitor treatment. They explained that this test, metaphorically, tests how fast or slow the traffic on the road moves, whereas pathology and Oncotype measure how many cars on the road.
The BCI is approved for years 5-10 for risk of recurrence and benefit of extended meds. However, I asked if the assessment of benefit could possibly also be true at time of diagnosis, since nothing has changed with estrogen responsiveness. They said absolutely but they are not FDA approved for years 0-5. My take away is that I may not have been getting benefit from Femara this whole time, according to BCI. But Oncotype says my risk was halved with meds. Geez!
Interestingly my risk of recurrence with BCI without meds was exactly the same as risk of recurrence WITH meds on Oncotype.
0 -
Thanks everyone.
Heard from her nurse. MO is now on vacation for 2 weeks. At my appt last eeek you'd think she would've mentioned that and who to follow-up with regarding my urgent Mammo & US. Anyway, her nurse said that because of lack of appt availability she would "try" to call me sometime in April. Wtf. It's BS.
As to the tests, since I am young, my prior 2 MOs both ran them & said these marker tests SHOULD be part of my continuing care due to my risk factors.
If you Google either one Breast Cancer surveillance comes up. So the fact that MOs reasoning for not doing them in her msg that "these tests are not run for breast cancer" is again BS.
I'll be seeing new MO on 3/24. I don't wan't to start over, again, but I refuse to go to a MO who won't even explain basic things to me or find 5 minutes for a phone call. These questions are not out of line, they are basic.
I surely hope NCCN guidelines or criteria or sone study has come out that explains why this MO suddenly changed her view on my RR but until I know more, I'm going with my surgeon and prior 2 MOs consensus that my RR is 28-35% remains at because of many factors they explained to me...young age, oncotype, stage, weight, and that I cannot be on hormonal treatments or go thru surgery due to my MS.
This whole situation is messed up. I just need to get through it & move past it. Hopefully new MO will be willing to take her time to explain things and answer questions if needed. That's all I'm asking for; consideration, respect, and understanding given the big picture of my extensive medical history.
Thanks again everyone for the support and consoling me as I run through yet another obstacle course. Its grueling.
0 -
I'm glad you have the chance to see a new MO, though I wish you didn't have to. I hope the next one will be better.
Now I'm imagining like a Yelp for oncologists...
0 -
I’m just catching up on all this. It’s been crazy with coronavirus updates and now CA is in lockdown aka “safer at home”. Luckily my company is e-commerce and I can work from home but work is nutty, we are assessing demand daily and making changes.
Anyways - SPOONIE - I am glad you got a new MO! Not answering your questions until an August appt. is not right. My MO emails me (when I send emails through the system I just have to say I want to hear from him directly and he always responds within 1-2 days) and calls on the critical things outside of the in person check-ups. In fact I just emailed him about a completely random request to see if he can help prescribe some asthma medication so I could have it on hand.
I had the luxury of meeting Raya already through our emails, my she is the cutest cutest kitty!! Ray a sunshine indeed.
GOKALE and HIKINGLADY - I’ve heard both sides re: plant based is best vs eating meat is fine. I would probably go plant based if I could but the fact is I like meat too much so that decides it for me. I am going to have to have faith in studies that showed Mediterranean diet cultures and Japanese cultures eating lots of fish are some of the healthiest with the lowest incidences of cancer. My MO also thinks it’s more about reducing sugar and weight but my regular doc believes a lot in plant based.
SALAMANDRA, GREENHARBOR, EDJ3, BENNYBEAR, YOGATYME, WINDINGSHORES and others - so glad you’ve been in this thread to support Spoonie and one another. I really value our community and I don’t check in as often as I’d like because work and life gets busy. Although now with CA Safer at Home mandate for at least the next month you may hear more from me!
I am still on tamoxifen, fine on tamoxifen except for the frustration that it’s near impossible to lose weight on it. The husband and I are hunkering down and the one upside of this stay home mandate are that the pups love us being home! Stay safe everyone.
 0
0 -
I had a mastectomy on right side in October. Oncotype was a 6 but they put me on Chemo because of lymph node extensions. Starting radiation next week. My Dr. wants me to start taking 2.5 Mg of Letrozole as soon as radiation is done. I am post menopausal. I sailed through menopause with hardly any symptoms at all. I had 1 mild hot flash. Not looking forward to a second, more intense menopause. The chemo I had was Taxotere which can kill the hair folaccols resulting in permanent hair loss. I finished chemo in February and I was told to wait until May to see if I will ever have any hair growth or not. I also struggle hard to control my weight. I wanted to loose at least 10 pounds once treatment was over. Letrozole has the longest list of side effects I have ever seen, including hair loss and weight gain and that’s the least of it, but still concerns me. Isn’t weight gain a cancer risk factor? I will be having a DIEP, so what is the point of taking away the stomach fatand then taking a pill to gain weight? Anyone on Letrozole? What has been your experience?
0 -
Hi Padug, I had a DIEP (Feb 18) and then started ovarian supression (Oct 18) and anastrazole (Dec 18). I also went into hormone therapy with about 7-10 pounds to lose. I was told I would gain weight. I have had to be much more mindful of what I eat, how much exercise I get, I weight myself a few times a week to keep an eye on it, etc., but I have not gained weight, and my stomach is still flatter than before as a result of the DIEP (much of my stomach, I learned, was from a "severe" undiagnosed diastis recti from my pregnancies which they repaired while they had me open for the DIEP). I gained maybe 3 pounds over the holidays and have re-lost it. Haven't made any progress on losing the 7-10 lbs I went into hormone therapy wanting to lose, but haven't really tried. It is definitely possible to not gain weight.
0