Starting/declining hormone therapy Nov, Dec, Jan 2018
Comments
-
Hi MDRR,
In response to what I am taking now for my bones, I take the usual recommended supplements for bone stability. I recently added Strontium, this was a suggestion by one of our fellow BC survivors. I ordered it from Health Concerns, it is call Biostrong, I take 2 pills on an empty stomach, 2 hours in between meals. I have been off the Arimidex for a couple of weeks now because of the bone pain and stiffness. I see my MO on Wednesday, I had thought about switching to Tamoxifin but I have been reading some pretty scary things about it including Lupus. I was totally unaware of liver issues. I recently had bilateral mammograms and ultrasounds everything looks good after two years. We all just take one day at a time!
0 -
Purplecat
I see both a medical oncologist and an oncologist at an integrative cancer center. The MO monitors my arimidex intake and effects; the other meets with me every 4 months to discuss nutrition, lifestyle, monitor my blood work, etc -- it's a fabulous resource and I learn so much. We have not discussed soy, but she definitely wants me to introduce flaxseed into my daily intake. It can be a hassle to grind it yourself but there is a kind of sprouted ground flaxseed that she said is the best, already ground, has good shelf life, and I add about 1 tbsp per day to one of my meals - very easy. While my estrogen is quite low due to the meds, it is metholating in a way that is not ideal, so we are working on how to have my body process in a different way, and a good bit of that is through nutrition and supplements.
0 -
Dear Spoonie, Thank you so much for picking up the torch and running with it. I am so tired due to my liver condition I have some days that I can hardly get out of bed. I was 6 weeks out of rads when my liver failed and I haven't had a chance to catch my breath since BC diagnosis before I was thrown into another (potentially terminal) diagnosis.
I asked my specialist (head of Hepatology at the transplant clinic at Toronto General Hospital) why wasn't the impact on the liver ever mentioned when I was prescribed Tamoxifen? He said there is much debate about it. Oncologists prescribe in the context of cancer and for now, Tamoxifen is the most effective drug to reduce risk of recurrence. Hepatology feel that liver monitoring should be a gold standard of care while on TX but oncologists don't want to scare people away. Interestingly, it is only approximately half of women on TX actually complete 5 years due to the side effects.
I can't thank you enough for listening. I have felt so marginalized as I am now straddling two chronic diseases and the BC support handed me off to hepatology and hepatology are frustrated as oncology won't change their policy. My liver specialist said he wants to make an example of my case to say "see this is what can happen without appropriate monitoring." Mine is an extreme case wherein I went right to stage 4 cirrhosis as I built up a toxic level of TX. Adequate monitoring would have seen elevated liver enzymes and TX would have been stopped immediately. I could have been caught at the early stage of NAFLD. The bottom line is: for the women that do experience NAFLD induced by TX it is life altering. You then have to deal with BC and a second life threatening condition. The breast cancer clinic where I received treatment just seem to want to sweep my case under the rug so as not to dissuade other women from taking TX.
It also strikes me that big Pharma do not like cases like mine as TX is a multi-billion dollar business. I am not anti-drug but I am anti-irresponsible prescribing and monitoring. I sure wish I could turn back time. A simple blood test would have alerted my oncologist to my critical response to TX. My greatest fear is that if my BC recurs I can't have chemo. Even if I hold on long enough for a transplant the immunosuppressant meds required to prevent organ rejection roll out the red carpet for BC reactivation. I'm just focusing on nutrition and exercise when I can plus living each day to the fullest. Thank you again for sounding the battle cry. We are sisters in our strength to speak up in unison. Cheers, Liz
0 -
Canada Liz, patients have the right to know all of the side effects so they can make an informed decision. Additionally since this is such a serious side effect with multiple implications, every patient that is on tamoxifen should be having their liver functions monitored especially if they've been on previous chemo. I am so sorry this is happening to you!
0 -
And kudos goes to dear Spoons for helping us all get educated! Those were some heavy hitting research projects! Thank you.
The take away is that if tamoxifen is on the table for your tx, talk to your MO about your liver. Ask how often they will monitor your liver function.
0 -
CanadaLiz - I think this is a common thread in the ONCO community. Can't recall reading about many posters saying that their MO did a blood panel for the liver before handing out the Tamox rx. But then again, maybe they did and just didn't mention it in their post. In any case, I know mine didn't. It's a scary thing. And in your case, it must be so disheartening and angering to know that with proper surveillance this could have been prevented! I am just so sorry that you are dealing with all of this on top of breast cancer.
It's a shame that MO in general seem to prefer not to scare us away, yet by doing so, they potentially put our lives in other forms of jeopardy. I agree with Wised wholeheartedly, that no matter what, patients have the right to know all pertinent info, and to deprive us of that is a violation of rights IMO. Sending you my best wishes and I will continue to speak out in your name my sister in arms. I too know the fatigue, drain, and stress/depression of straddling multiple conditions, so my heart goes out to you. It is not something anyone dreams of doing, that's to be sure.
0 -
CanadaLiz, I am so sorry for all that you are going through. Thank you for sharing such valuable information. I don't see my MO until February so I will have time to research hormone therapy and I will ask for baseline testing. Thanks for all of the links, Spoonie. You are making the research task easier.
Pebbles, my MO never mentioned tamox and I guess I thought it was used only with premenopausal women. Are results supposed to be better/different with AI? Is it indeed an age thing, or is it chosen based on the amount of estrogen? I had the feeling that AI was recommended for me because I turned down chemo, but now I will ask. I like the idea of easing into AI that was suggested by Ingerp and I will ask about that as well.
Wised, did I read correctly that you were told that Zoloft is not compatible with Tam, but okay with AI? I will see a nurse on Wednesday and ask more about that.
It's great to have new voices on this thread. Welcome!
This thread is really helping me to know what I need to ask about.
0 -
I also thought the Tamoxifen/AI decision was based on whether you were pre- or post-menopausal. T shuts down the production of estrogen in your ovaries but post-menopause it's made in other areas of the body so the AI is a different mechanism.
But all of this reading about liver impacts makes me want to ask if the same thing potentially happens with an AI? I've never heard of that. I did find this: https://livertox.nih.gov/Anastrozole.htm .
0 -
From what I understand, they usually prescribe AIs for post-menopausal because it’s slightly more effective short term (although seems long term both are equal), not because you can’t take tamoxifen post-menopausal. They actually did a study on post-menopausal women taking both. Article here: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)61074-1/fulltext
“In the comparison of 5 years of aromatase inhibitor versus 5 years of tamoxifen, recurrence RRs favoured aromatase inhibitors significantly during years 0–1 (RR 0·64, 95% CI 0·52–0·78) and 2–4 (RR 0·80, 0·68–0·93), and non-significantly thereafter.“
So if it’s like our friend’s experience, they start with the AI first but if side effects are too hard to tolerate thenswitching to tamoxifen is an option.
When you’re pre-menopausal, AI is not an option as it’s not effective. https://www.ncbi.nlm.nih.gov/m/pubmed/16002281/
“In women whose ovaries are active, a temporary inhibition of E2 production will raise gonadotropins and in turn, stimulate follicular growth. In cancer patients, this property precludes the use of AIs in women whose ovaries are still active...”
I’m pretty amazed at the liver damage association with tamoxifen like the rest of us and plan to reach out to my MO and see what he says. Weird that we haven’t heard more cases with a high 30-40% risk of it. Here’s how Domino feels about us not being properly informed of that!
 0
0 -
Hi everyone, anyone who's ovaries are not functioning can take an AI. If you are premenopausal, they shut down your ovaries with Lupron or something similar. I am allowed to take Tamoxifen as a post menopausal woman but it is slightly less effective and I cannot take it with Zoloft.
I love the exchange of info on this board!
Oh and I love the picture of Domino playing with poop! I must resist the temptation of looking for a little Domino for myself!
0 -
Everything we put in our mouth effects the liver. Look at acetaminophen and a host of other things we use Hence, warning about mixing alcohol and meds.
0 -
JoE777 - You're definitely correct.
 Everything in our body passes through our liver and could possibly affect its ability to function.
Everything in our body passes through our liver and could possibly affect its ability to function. My bottle of Tylenol warns me that if I take too much or too often or with other meds/alchohol my liver is in for it.
That being said, there is no risk to my liver if I take the recommended dose as directed. Conversely, taking Tamoxifen, as directed and at the recommended dose, does in fact pose actual risk to my liver.
I've not seen studies that say we have a 30-40% risk of acquiring non-alchohlic fatty liver disease from Tylenol but I have for Tamoxifen. Unlike my bottle of Tylenol, my rx of Tamoxifen did not warn me of this. Nor did my MO warn me of this.
That fact ticks me off. IMO we should all be made aware of the risks before we take a med and unfortunately it seems many MOs are not informing their patients of this risk nor monitoring this liver test. To me that is a violation of my rights to be informed. Know what I mean?
It breaks my heart that CanadaLiz basically lost her liver to Tamoxifen and it could have been prevented by a few simple lab tests and her being informed about liver risks. It's just not right. Le Sigh.
Wised - I too cracked up at Domino's toy, her little "poop emoji"!
 And no need to say thanks about the reference studies and such. I like to investigate. Information is power and that sort of thing. Just glad to help us a little along the way.
And no need to say thanks about the reference studies and such. I like to investigate. Information is power and that sort of thing. Just glad to help us a little along the way.Pebbles & Wised - Thanks for the explanation about Tamoxifen for post-meno women. Cleared my confusion right up.
 0
0 -
Well, I am pre-meno, but my doctor put me on anastrozole with Lupron shots. She believes it being more effective for intermediate risk patients.
0 -
Spoonie,One thing that has concerned me is how many I've heard that don't have liver panels done every visit With their oncologists. My first go around I had liver panels every 3 months, after radiation which was once a week, now I have them once a month while I'm on kisqali. I don't know what the majority of girls protocol is. Thanks for the info. Jo
0 -
Jo - that's so great that you have liver panels done. I agree that it's odd that with this potential side effect, they don't do that for all of us!
Spoonie / Wised - LOL I love that you totally "got" that Domino thinks us not being informed of this risk of fatty liver disease is a whole lot of poop.
InnaB - that's super interesting. Have you started the anastrozole with Lupron shots yet and how have the side effects been if so? Did your doctor say anything about side effects for that vs. tamoxifen?
I e-mailed my MO this morning so I haven't heard back yet but I thought I would post one more pic - representative of how we all feel of starting hormone therapy, and not being told about this potential for fatty liver disease! This one also has a cameo from Kit Kat, our most adorable and littlest of the little ones who "crossed the rainbow bridge" in March earlier this year. Still miss her everyday!
 0
0 -
I was supposed to take an AI because I'm 68 and had a hysterectomy ten years ago. Not only has that ship sailed, but the dock was completely demolished 😀. But, I already have osteoporosis and can't take Prolia, at least for now. So my MO said we'll give Tamoxifin a try. I'll start it next week, and she'll see me later in January - at which time I'll ask about liver issues. Sigh.
0 -
Pebbles, I started Lupron shots last months and Anastrozole last week. I believe it takes a few months for side effects to appear. Your dogs are adorable
0 -
I've been on Anastrazole since the end of October and started getting hot blazes right away. Seriously, this is hotter than I've ever felt. (And not the good hot) I has mild headaches when I first woke up in the morning that went away and some achiness. My most concerning side effect has been a worsening of the chemo induced peripheral neuropathy that I got three years ago. That is the side effect I will be addressing again with my oncologist next week. They had me start taking gabapentin last month and it helps with the symptoms I just don't like taking another pill.
0 -
Good morning all. Thank you for creating this group. I will be getting my first lupron shot on 1/2, coupled with femara I believe. Like Inna, I am premenopausal but it is recommended that I try for the AI first as new research, studies, etc. believe it is more effective than tamoxifen and will cut my risk even further. I should say that I'm highly ER/PR + (95% each). I will have a detailed discussion on 1/2 about side effects but I decided to schedule the shot at the same time. As with chemo and radiation, you cannot predict side effects ahead of time. They want the option of the AI and then if I really cannot tolerate it I could perhaps consider tamoxifen. Pick your poison I guess. For now, the AI seems to have "better" bad side effects than the Tamoxifen.
The chemo has put me into early menopause so I am having muscle weakness, stiffness, knee pain, and hot flashes. I'm not sure if it is residual chemo effects or because of the lack of estrogen. That's a question I have for MO regarding AI, what will be the drug and what will be the result of the lack of estrogen/progesteron?
FYI, I had my liver levels checked every chemo round (amongst other things).
I am also seeing a naturopath re supplements and nutrition. I wanted a second opinion so to speak and while I'm at one of the best hospitals in the country, they are not as nutrition oriented as I hoped for. I do have an appointment with a nutritionist at the hospital tomorrow so I'll see. But per the naturopath and my own research I'm avoiding soy, flax, hemp, CBD, a number of supplements like evening primose, and commercial meats (which I did anyway) and non-organic dairy. Largely because of my estrogen status. The nutrition stuff is frustrating and I would freak out if I eat an errant flax seed, but I'm avoiding it as best I can.
I am looking forward to taking tumeric and chaga mushrooms again post chemo and radiation. The MO and the pharmacist did say to stop these until after active treatment, but I hear that they can really help with the muscle pain/stiffness.
0 -
Hey all!
Tigerlily, I'm really interested in your path because I was thinking about whether I should do that because it does seem to be more effective. My docs didn't think the extra benefit would make a difference in my case... That said, my tumor was larger than yours and also stage 2. Can I ask why you ended up having chemo with your size tumor? Did you have a high oncotype or something?
CanadaLiz, I'm so sorry for your crappy experience. That is really not right. Thank you for sharing and thank you Spoonie for expanding. I will definitely ask my MO about liver monitoring at our next appointment in a couple of months. Now I'm picturing an internet board for the oncologists and they're like, 'hey, what's up with all these patients asking about livers now?'
Wised, thank you for starting this group.
I think I hadn't really wrapped my head around how long it would take for all the side effects to play out. I had some side effects when I was first starting. Like, two days of really dry eyes/mouth, then two days of my old ankle injury acting out again. Then it seemed fine for a while.
I understand why docs want to separate out the radiation and hormonal therapy, since I've gotten all this heartburn that the radiation oncologist denies is from the radiation and is pointing me at the MO for. (Of course, the nurse at the radiation clinic said she sees this all the time with ladies getting breast radiation and tbh I kind of trust her more. Where do the doctors get these absolute convictions about lack of side effects?) I've also had headaches but again, I don't know if that's related to the radiation fatigue and me not sleeping enough or to the tamoxifen.
But I really wanted to start the tamoxifen while I was off of work for radiation so I could get as many of the SE either over with, treated, or at least familiar, before I go back to work. So it is what it is.
I had a moment where I got really hot. I was wondering if it was a hot flash, or if I was just especially ensconced in the covers. But then I was wondering if it were, I'd truly know. Is there such a thing as subtle hot flashes? That's the closest i've got to that. But it has been just about 3.5 weeks and I know other SEs could come into play as my estrogen levels keep adjusting.
Pebbles - thank you for sharing Domino and Kitkat with us. They brighten my day every time. I will try to step up my cat pictures game
 0
0 -
Hi Salamandra, first, re hot flashes. A lot of times they are very subtle. Sometimes I can prevent them if I have a glass of ice water nearby. I had some really intense ones but acupuncture, not drinking hot tea at night, and theamine are either working or the effects of chemo are wearing off (I'm 7 weeks PFC). As for the chemo, my oncotype was 20 so that's why I agreed to do chemo. I am 45 and it came back as a 13% recurrence risk and I as told that chemo would cut it in half. The 13% assumes tamoxifen and I'm also told they believe that AI will cut it further than tamoxifen. My oncologist was close to the study that was released in June and was very detailed in explaining the flaws in it, what they should have done differently, and what's next. I will ask a lot more questions when I go back in a couple of weeks, but that's how I ended up where I am. I am also not sure how the fact that 95% of my receptors were estrogen/PR positive factors in. I'll know more soon and let me know if you think of any questions I should ask. I believe you're at MSK? Why are they saying it wouldn't benefit you?
0 -
Bloody hell......why do we have to be our own advocate for our health care??? Seems like your liver should be monitored with any med that's used long term.....I questioned my oncologist as to why estrogen levels weren't checked to make sure the meds they give us are working.......she said they do and then scheduled me for a bone scan, but no labs.......geezzzz......
0 -
Thanks TigerLily. That's helpful to know about subtle hot flashes. In that case I'm pretty sure I've had at least one and maybe a few.
I am at MSK. The MO had offered me OS+AI if it were important to me to stay on the antidepressant I've been on. I asked her if there would be a therapeutic benefit for me over tamoxifen to doing that, and she said no, not in my case. (So, not that there would be no benefit from the AI, but not a greater benefit than tamoxifen, or at least, not big enough to be worth the drawbacks?) She didn't explain but I assume it's because I'm considered low risk. I had a 9 on my oncotype. Still, diagnosed at 39 and family history.
To me it seemed like the SE profile was more intense with the AI than with tamoxifen, and I didn't push on her answer, to be honest, because I think I was happy to hear it and avoid the decision.
The June study you mentioned, it's the one that showed greater benefit for high risk women with femara+AI?
0 -
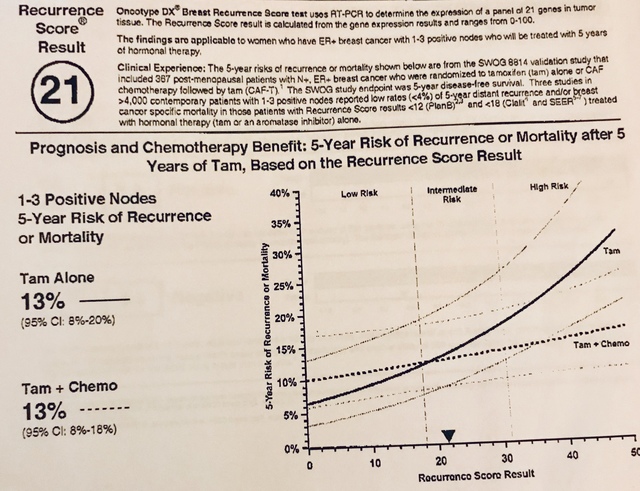
Tigerlily - super interesting that we have similar oncotype and opposite recos from our MOs! I'm 43, premenopausal, oncotype 21. For me it said risk of recurrence with tamoxifen 13%, and risk of recurrence with tamoxifen plus chemo 13%. So my MO said that he would no longer recommend chemo due to the added toxicity it could introduce to my system and the fact that the oncotype score indicated it would be of no benefit. I asked him how accurate the oncotype was and he really believes in it, said the stats are based on thousands of women with the same oncotype who were treated one way or the other and their results.
I hope your MO shared the actual oncotype report with you vs just making a blanket statement about chemo cutting the recurrence risk in half. I noticed on the chemo boards that a lot of women with higher oncotype scores had something closer to 18-20% recurrence risk with tamoxifen alone vs. 12-13% with tamoxifen plus chemo so they chose to do chemo to bring their recurrence down to the 13% that ours is already at with tamoxifen alone.
My MO said my rate of recurrence without doing anything is prob around 20%, then the radiologist said with having done radiation that knocks it down to 14-15% and hormone therapy might bring it down another 3% after that, so down to 11-12%. There are studies that show with proper diet and exercise, we could improve our odds further, possibly by another half, so my 13% with tamoxifen could knock down to 7% with the right diet and exercise.
I don't know, it's all a numbers game and you really don't know what side of the coin you'll land on, which is why I go back and forth on even taking tamoxifen sometimes. I guess we just have to do what we can and hope for the best.
BTW for all - I have NOT heard back from my MO yet regarding tamoxifen and liver disease and he usually emails me back within 24 hours Hmmm... 😮🤔😡
Salamandra - looking forward to seeing the cats!
Wised - I get it, I don't want to have to take a pill to manage a pill and so on. Have you considered acupuncture to help with the neuropathy? My mother-in-law had chemo induced neuropathy and acupuncture helped immensely. And more Domino (plus Tucker) below
InnaB - thank you for letting me know! It's good to know there's an option if I get concerned with potential side effects of tamoxifen
AliceBastab - our friend in her 60s is also on tamoxifen, having switched from an AI and she's really happy she made the switch. She says she was miserable on the AI and doing great on tamoxifen.
Typing this while I have these two pups on either side of me.

 0
0 -
Pebbles, I have the full report. It says that for women under 50 (premenopausal), the benefit of chemo for women who have an oncotype btw 13 (I believe) and 20 is 1.6% and then women starting at 21 have a benefit of 6.5% reduction in risk, with chemo. These numbers assume tamoxifen. But that is what the oncotype report says and they are ranges. I am at 20, which is closer to the 6.5% benefit tha say being at 13 which is lower in the 1.6% range. So it was strongly encouraged that I do chemo and that by btw that and the AI I could cut the 13% in half. Also my Individual characteristics are taken into account. That said, it is all percentages and ranges and people with an oncotype of 0 can have a recurrence. The study released in JUne did not look at diet and exercise and I was told it will not change percentages. But i am still focusing on it
0 -
hi thecargirl
what did the MO say? Did you switch meds?
0 -
Tigerlily sounds good and it seems like the nutrition helped get you through chemo really well so that’s great!
I have a useful link to share with all - https://foodforbreastcancer.com/amp - this evaluates certainly foods / nutrition science backed, based on studies that have been done to showcase the efficacy of certain foods to help fight breast cancer. Based on what I see here, it does seem nutrition can be additive!
Here’s their intro: “Current evidence-based information on how to reduce risk and survive breast cancerFood for Breast Cancer provides information on how various foods and other factors affect breast cancer risk, prevention and prognosis. The findings are drawn exclusively from scientific studies and updated as new research becomes available. Our goal is to provide breast cancer patients, survivors and those at high risk for breast cancer with information to help prevent and survive breast cancer.“
Also here is one of many studies on the benefit of exercise to help prevent recurrence:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127611/
“The preventive effect of exercise for breast cancer has been shown in epidemiological studies[6,7]. Risk reduction with physical activity for breast cancer in females is estimated to be up to 25%-30%[1,6]. To achieve such an effect, women are recommended to follow a 150-min per week exercise regime of moderate to vigorous intensity consisting of sports or other physical activity[4].“
So my onc does believe in the link between exercise and preventing a recurrence, but on nutrition he is more about overall fat vs. what you eat. Interesting how different docs have different opinions! It’s true what ghostie13 said that we have to be our own advocates for health care to a certain extent!
Anyways here’s my oncotype report. Maybe for me it’s a different thing because this report is specific to positive lymph nodes.
 0
0 -
Salamandra, the study I was referring to is the TAILORx study from June:
https://www.cancer.gov/news-events/press-releases/...
So Pebbles, I was looking on my phone before and didn't see the picture you posted. My graphic is different. It doesn't repeat the 13% and doesn't show the second percent, but it shows a gap between the two lines. Mine don't cross like your's did and it shows the benefit of chemo. So that means the reports are specific, again, I had no node involvement and have my high ER/PR. What I find interesting is that they told me if it was in the nodes, chemo was definite. Going into surgery they were pretty confident it was not in the nodes (and were correct) and were hopeful no chemo, but the oncotype came back higher than they thought. But again, I guess we know that the reports are very specific. I pulled mine out this am to look at it again based on this discussion.
I am back at work. My boob is throbbing. It's pissed. But not red, so will take the good and the bad.
0 -
Hmm, I had one node with a smidge of involvement, but my oncotype was 17 so no chemo.
0 -
My oncotype was 16, no nodes involved. No chemo, finished with rads and still debating on AI's. ....
0