When do most recurrences for HER2 happen
Comments
-
Another study to watch for results, this one offered for stage IIIa HER2 positive breast cancer patients who have had no previous treatment, that has been completed. This one was offered mostly it appears outside the US in Brazil, Columbia and Peru:
6 Weeks Treatment of Locally Advanced Breast Cancer With BIBW 2992 (Afatinib) or Lapatinib or Trastuzumab
http://clinicaltrials.gov/ct2/show/NCT00826267?term=neoadjuvant+herceptin+breast&rank=53
0 -
This trial is in the United Kingdom, for early breast cancer. It is currently recruiting participants. It does include conventional treatment, but I it appears that is given after either the trastuzumab or the lapatinib ditosylate:
NCT01104571
Trastuzumab or Lapatinib Ditosylate in Treating Women With Early Breast Cancer
http://clinicaltrials.gov/ct2/show/NCT01104571?term=neoadjuvant+herceptin+breast&rank=61
0 -
This one in France has been running for a while, and is still recruiting participants:
NCT00674414
Trastuzumab With or Without Everolimus in Treating Women With Breast Cancer That Can Be Removed By Surgery
http://clinicaltrials.gov/ct2/show/NCT00674414?term=neoadjuvant+herceptin+breast&rank=68
Note:
Criteria
DISEASE CHARACTERISTICS:
Histologically confirmed diagnosis of invasive breast cancer
- Previously untreated disease
(If these studies prove worthwhile, it looks like the US will be behind the curve since most of them appear to be happening elsewhere....)
A.A.
0 -
I just realised it is the 2nd anniversary of my first chemo treatment - yippee!!!
Sue
0 -
Sue - happy chemoversary! I calendared all that stuff 10 years ago - still have it all as recurring events in my calendar so I can celebrate being done with that junk. Do something nice for yourself today!
Sarah
0 -
Yayy Sue!0
-
AlaskaAngel - I am interested to hear about the results of the PHARE and Persephone and SOLD (NZ) which compare short and long duration of herceptin therapy. It looks like there aren't any completed herceptin treatment alone clinical trials in early BC, but they are working on combining herceptin with anti-estrogen treatment - is that how you would summarize the trials that you found?0
-
At least the one trial is doing that, yes.
Here's my personal hypothesis. If they separate out the data from these trials I think they would find that there are two basic steps that would have to be done to bring about the highest success rate.
What chemo does that makes some difference at times, IMHO, is to blast the ovaries and bring about chemopause.
So, to get the best success with trastuzumab alone, they still would need to add in some form of ovarian ablation other than by chemotherapy.
I hope they don't miss the boat with these studies by continuing to require chemotherapy AFTER surgery.
But can they, will they, see that far ahead of their nose?
Correct me if I am wrong, but the DCIS study indicated that the use of trastuzumab primarily boosted the immune system response. This is the opposite of what chemotherapy does. The question is, would boosting the immune system with trastuzumab and making sure to add in ovarian ablation produce as good or better outcomes than the current treatment with chemotherapies and trastuzumab? Is part of the problem that they have been holding trastuzumab back from having its full beneficial effect by adding the chemotherapies? And what role is involved here in terms of inflammation and cancer in terms of the support drugs used for chemotherapy, such as steroids?
AlaskaAngel
0 -
AA - I wondered about that last year - that one way herceptin is thought to work is by antibody dependent cell-mediated cytotoxicity (I think that's right) and then chemo was basically messing with the immune system at the same time (though with neulasta that effect may not be as strong). From what I have read cancer cells can be really wacko in their physiology so it does makes sense to me to hit them with chemo. Since they are so wacko they can't recover from the chemo-damage. It's just that chemo affects so many normal tissues as you know. There are some older studies that look driectly ovary ablation as a treatment. I don't have them here but if you are interested I could check when I get home.0
-
I think that the decades-old technique of using the sales pitch of the image of applying highly toxic substances in the hope that it "wipes out" enough cancer cells so that the immune system can then handle the rest is a sales pitch that works because it is very simple and easy to understand. (It reminds me of the image of spraying a cleaner on the counter that is intended to wipe out all the nasty organisms on the countertop, and that makes people feel better about the countertop.) In real life, I don't think the result of the application of chemotherapies is that simple or that effective.
If, for example, you use a spray on the countertop that works for only a very limited type of organism, it may make you feel better to spray the countertop but it may not do much to get rid of the variety of organisms -- and some sprays may even feed some of the organisms on the countertop.
Since most of the time the chemotherapy that is chosen either 1) isn't needed at all in the first place, or 2) doesn't work on everyone's particular cancer very well, like the spray for the countertop it makes people tend to feel like they have more protection than they actually have.
Some are lucky enough that they never needed it in the first place, and for some others it happens to match their particular cancer well enough (in combination WITH the endocrine effects of chemopause) that it helps.
What we have desperately needed (and haven't had) is not oncologists, but endocrinologists trained in dealing with cancer, to sift through all this with us together with other specialties in applying treatment.
- A.A.
0 -
The real problem is we just don't have enough information about cancer. Cancer is not just one disease. As we see not all breast cancers are treated the same way nor do they all react the same way. They are getting better we just don't have all the answers yet. I see tests like oncotype being the answer but they have yet to be developed.
We do have to have some faith in our doctors and the research. I've always considered myself a person lacking in (blind) faith. I need things explained to me in order to get on board. At the same time with this disease and much of medicine there is no 100%. We all have to have a little faith in medicine at times.
0 -
Ha ha lago - great song!0
-
Lago - I totally agree with you.
0 -
Here are 2 trials offering trastuzumab alone for the elderly:
NCT01104935
Evaluation of Trastuzumab Without Chemotherapy as a Postoperative Adjuvant Therapy in HER2 Positive Elderly Breast Cancer Patients (RESPECT)
http://clinicaltrials.gov/ct2/show/NCT01104935?term=elderly+trastuzumab&rank=1
and
NCT00796978
Trastuzumab in Treating Older Women With Early-Stage Breast Cancer
http://clinicaltrials.gov/ct2/show/NCT00796978?term=elderly+trastuzumab&rank=4
0 -
Good spotting AA !0
-
Nicely said hillck. I think reading 'The Emporer of All Maladies' helped me understand the nature of cancer and the role of mutations. It's a great book. Thanks for sharing.0
-
Thanks hillck for the very articulate explanation.
0 -
Thanks, hillck/Cindy. Every contribution based on genuine information helps to get closer to making better decisions.
It sounds like you are connected with the research process. The info I got on the percentage of those whose chemo matched their cancer in some way (enough to slow or hold off progression) was less than 20%, and I'm wondering if you know of any more current factual information about that?
If that is still accurate, it means that 4 out of 5 get no known benefit from doing chemo -- which isn't to say that one out of five won't get lucky, but it does mean subjecting the rest to it and to early aging and to all of the support drugs and cardiac risks, etc. for nothing. The lack of open information as to the actual percentage adds to the tendency to believe that chemotherapy is more effective (i.e, for one person, even if not others) than it actually is.
However, given the heterogeneous nature of cancer as pointed out, and the fact that chemotherapy is carcinogenic, we don't know how many patients have a return of cancer due to including chemotherapy in their treatment. Since there is still no way to know which chemotherapy affects which individual patient's heterogeneous cancer in a positive way, there is also the unidentified and unacknowledged risk that, as just one additional variable, chemotherapy can also cause cancer development.
That is the difference between using targeted noncarcinogenic drugs such as trastuzumab alone or in combination with other noncarcinogenic drugs, and using noncarcinogenic drugs in combination with carcinogenic drugs (chemotherapy).
This continues to be a helpful discussion.
A.A.
0 -
What I saw was an estimate indicating that about 17% of those who get chemotherapy have a helpful response to chemotherapy, and I think but am not certain that I saw it in one of the Research to Practice discussions done somewhere around 2006. It stuck in my mind because it is something patients don't think to ask specifically when they are trying to decide risk vs benefit, and it is a concept that is clear enough to allow a person to use some judgment in making the decision. The basis for the 17% would be important to know, but at the time I was thinking it would mean that 17% of the the group of ALL general types of bc patients treated with chemotherapy do better than the members of that same general group of all types of bc patients who receive no chemotherapy. (As I understood it, that 17%, by the way, included those who get brief respite with it who are only NED for a short time.)
Since chemotherapy is the major expense of treatment (as it comes only with all of the costs for blood testing, support drugs, IV treatment, doctor visits, and sophisticated staffing required inside expensive medical facilities) and is so toxic to the environment, and is not available to so many in the worldwide reality of breast cancer, I can't feel quite so enthused about how great it "works", particularly if it is being wasted on 4 out of 5 patients who are able to afford it.
AlaskaAngel
0 -
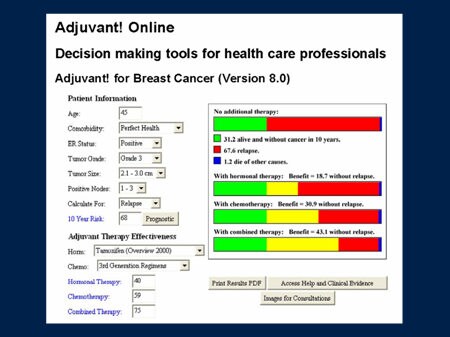 Here are a couple examples that might be helpful
Here are a couple examples that might be helpful 0
0 -
At the time I read it, the oncs participating in the discussion were not in disagreement with the estimate. Given that chemotherapy in one form or another has been used for decades now, if there is much genuine critical analysis about the use of chemotherapy for breast cancer, that number should be well known, unless they don't like to admit it publicly.
A.A.
0 -
I think in the second figure only 12 of the 100 treated women 'benefit' and in the first figure 43 women benefit from treatment. So the benefit of treatment seems to depend on the specifics of the cancer.
0 -
Here are some facts for you to ponder - retrospective study into chemo/herceptin for smaller tumours
0 -
hillck neoadjuvant chemo isn't only given for better surgical outcomes. They thought my tumor was 7cm before surgery (actually 6.5 cm if including the DCIS part) and I had surgery first.
Another woman treated at my center had the same size tumor and also HER2+ but had mets to her nodes but not ER/PR+. I'm sure since chemo/herceptin were her only guns I bet they wanted to be sure it was working. If it wasn't they probably would have switched treatments. If she had surgery first they would never know… and given that she wouldn't have endocrine theorpy to follow up… well you get what I mean. I also think her node involvement might have also been part of the decision.
0 -
The first onc I went to wanted to do neo-adjuvant chemo to "downstage" the tumor. if I was downstaged, perhaps less treatment. I ended up doing surgery then chemo. I often wonder if I had done chemo first, would all these nodes have been positive and what treatment course I would have wound up with. I had a re-excision post chemo for bad margins, and all was clean. That helped me mentally a bit.
In my head, I am glad I threw every available option at it.
0 -
Neo chemo was absolutely the best option for me-even though at the time all I wanted was for that big honkin tumor to be removed. Since I was Stage IV with very large and numerous mets we decided that starting chemo right away would be best. I have had almost CPR-and I will alway be convinced it was the combination of chemo with the Herceptin.
I have read all the links you have posted and have followed this conversation with real interest as I think several of the posters are some of the smartest BC people I have seen on this site. I never questioned my oncs advice to do chemo-and I had done some preliminary reading at that time-remember back when you were first dxed and there were a million questions and an urgency to just get started?? I just can't imagine any circumstance where I would ever say I won;t do chemo on the off chance it MIGHT not help me. The day is coming when they will be able to take our biopsies and determine which course of therapy is the best tool for fighting our individual cancer-until that happens I will take whatever drug they offer that kills some kind of cancer. Ask the ladies who are taking Avastin in combo with other drugs-FDA says Avastin doesn;t help BC- the research proves it. But if you are stable or NED while taking it do you think you are going to just let them take it away from you? Emotion is so involved in these decisions despite what science says.
I will be on herceptin til my heart says no or I get progression-hopefully a long way from now. With new Her2 drugs being developed I figure I will be in tx for the rest of my life-and thanking God and good science for it.
So no big intelligent thoughts or links-just the emotional part that worries that people would say no to chemo based on "what might happen".
0 -
I just saw my oncologist and we talked about this very issue! I had surgery first and then chemo back in 2007. She said now HER2+ gals are given chemo first, then surgery. If there is no sign of cancer at surgery time, after two years they are considered good to go. If they still have cancer after chemo, they know to watch them more closely.
Also, now they don't use the Red Devil anymore (unless someone is allergic to all the other choices). That evil drug damaged my heart!
The bottom line.... she said most HER2+ folks would recur within 2 years if the chemo didn't work, because it's such an aggressive cancer.
Good luck to all!!!
Miss S
0 -
Miss Shapen I think that is true for HER2+ ER/PR- but not so sure about us triple positives. My onc was involved in the initial trials for Herceptin (found out when I read the book the making of Herceptin). She knew about my case but did not recommend chemo first. But the other gal I mentioned (same onc and BS) who is HER2+ ER?PR- got chemo first. Also that 2-3 year window is correct (although not 100%) for HER+ Hormone negative but not quite the same for us triple positives. Granted all HER2+ is more likely to recur in the first 2-3 years but the risk doesn't go down quite as far for the hormone positive gals.
At least that's what I have read. I have yet to discuss this with my onc. Not sure I want to know at this point.
0 -
The holidays sucked 4 years ago - I had "the" mammo in mid-December, had gotten the letter saying to follow up and I could feel the lump - was scheduled for us-guided biopsy in early January. Just had to keep it all together during Christmas for the kids who knew nothing.
Needless to say, I LOVE all the oncs who discuss the 2-3 year window for hormone neg/Her2+. And it amazes me how much has changed in the 4 yrs since my dx. I was in the Neratinib trial, and it seems that new approaches to our disease and new treatments for it are in trials now and on the horizon.
Happy Thanksgiving and best wishes to all (and lilylady - hopefully a LONG, long run on the current drugs and then new ones to come!)
Sue
0 -
Hi Ladies
So timely. I just saw my onc a couple of weeks ago--in fact, I may have posted afterward. I posed these very same questions.
Basically, she said the 2-3 year window is typically accurate if you are HER 2+ but hormone negative. I'm triple positive, and she said that, as a result, cancer could conceivably come back outside that window, at any time, since it is hard to strip the body of hormones entirely.
That lead into a discussion about having an ooferectomy vs. hysterectomy. Which is a separate discussion. I'm very curious being on the Neratinib trial for 6 mos, whether the recent drop in WBC counts is a result of the drug. Thanks for the feedback ladies!
0