Interpreting Your Report
Comments
-
There a lot of info to unpack in your post.
An US bx is called "discordant" if the path finding disagrees with the imaging diagnosis. It doesn't matter that they are both benign. If I suspect a "benign fibroadenoma" and just "benign breast tissue" is found on path, then I have to assume I missed the target during the biopsy. Depending how sure I was that its benign, the choices are a) re-biopsy by US or other imaging b) look at it again in 6 months or c) excisional biopsy. After explaining all the options, I always complied with the wishes of the patient. If the US biopsy was very difficult because of the position / size / location of the target one might lean toward an excisional biopsy to make sure the area was adequately sampled.
When I recommended an excisional biopsy, I would only refer them to a qualified breast surgeon on staff, one that did nothing but breast surgery both benign and malignant varieties. The ones I worked with had fellowship training in breast surgery which included techniques in plastic surgery to make the scar as invisible as possible by placing it correctly and using many many fine sutures to close as if one was repairing a wound on someones face. This method of breast lump removal is referred to "oncoplastic" surgery.
It is a common myth that a benign result means it was an unnecessary procedure. The purpose is to answer the question "is it cancer or not?" and that question was answered by your excisional biopsy.
0 -
Thanks for the article, djmammo. I don't know why my onc is so concerned. (This was the spot where I had a strange unexplained bruise on the breast a while back). I know there's some distrust of the radiology department ever since they labeled my femur lesion as being on the right and followed me for months and months on the right side, re-imaging and continuing to say everything was fine, when in fact I had a lesion on the left side.
My onc is sending me to a new breast surgeon to look at this area that was noted as "magnetic susceptibility artifact", but I'm now considering cancelling if it's really nothing, as I'm getting sick of all these appointments.
0 -
thanks edj3 and djmammo!
that makes sense djmammo. I think what mostly bothered me about this was that the radiologist didn't speak to me, just put his recommendation on the patient portal and I assume sent that recommendation to my primary care physician, but I contacted my pcp first since I saw it on the portal immediately. My primary care physician then recommended a surgeon to me. Hard to tell how bad the scar will be since it's still healing, but it's around the nipple and I was told that this method can create less visible scarring in the end? "Oncoplastic" surgery wasn't mentioned, but this surgeon specializes in "Surgical Oncology and Breast Cancer Surgery" and came highly recommended by my PCP. So, the radiologist didn't explain the options to me at all, just recommended an excisional biopsy and I went with that as a result. During the ultrasound guided needle biopsy, he seemed very sure that he got a good sample, so maybe he thought that an excisional biopsy was the way to go, rather than repeat the procedure. I have no idea since he wouldn't return my call. I feel like I rushed into this without all the information and without knowing that "oncoplastic" surgery existed, but I guess time will tell what the end result looks like.
The breast surgeon who did the excisional biopsy was affiliated with a different medical establishment than the place where I got the initial ultrasound and initial needle biopsy. I might just look to switch to that place for future screenings. It's ridiculous that a radiologist will just put a recommendation on a portal and not actually speak to me to tell me my options. His recommendation was just excisional biopsy with no explanation, and that's it. Hoping this other place is different. The radiologist who did the scavi scout procedure the day before at the place where I got the excisional biopsy claims that she returns calls and seemed appalled that he didn't.
0 -
Hi Djmammo,
I was wondering if you had any insight to my Ultrasound report? Here ate the findings: A hypoechoic area with slight irregularity and increased color flow at the 3:00 position of the left breast, 4 cm from nipple is now appreciated. This is an indeterminate nodular density. Birads 4C.
I had a biopsy last week. Results will be in later this week.
I thought is was odd that I was a 4C. Thoughts?
0 -
Can I please ask for some help with my report?
I know I have cancer in my left breast. I have a tentative date for lumpectomy which will be followed by radiation. But then they wanted an MRI to determine if I am "high risk". If I am, surgery will be delayed to do the genetic testing and if that comes back positive, they may recommend full bilateral mastectomy. I should just sit back and wait till I see the doctor but I need to arrange work and kids if I'm having surgery next week.
The MRI report reads:
Findings
Background breast parenchymal enhancement is extensive which does reduce the
sensitivity of the investigation. There are numerous cysts scattered in both
breasts consistent with fibrocystic change.
Left Breast
1. 4:00 - 67 mm from the nipple, in the posterior one third of the
breast, there is an intensely enhancing mass measuring 15 x 13 x 13 mm (AP x
TV x CC). This demonstrates rapid wash-in and rapid washout on CADstream
analysis indicating a malignant pattern of enhancement and corresponding to
the biopsy-proven carcinoma.
Several foci of enhancement are seen throughout the left breast, difficult
to differentiate from the extensive background parenchymal enhancement.
Right Breast
No overtly suspicious mass or area of non mass enhancement. Similar to the
left breast, there are several foci of enhancement with intermediate
enhancement characteristics which are difficult to differentiate from normal
background parenchymal enhancement.
No axillary or internal mammary lymphadenopathy. No osseous lesion in the
anterior thorax.
Conclusion
Solitary mass at 4:00 in the left breast measuring up to 15 mm in size.
Background parenchymal enhancement is extensive with evidence of fibrocystic
change which does reduce the sensitivity of investigation. Followup
recommended.0 -
"Surgical Oncology and Breast Cancer Surgery" and "Oncoplastic Surgery" are basically the same title. The problems that I have personally seen is when someone goes to a general surgeon who does one or two breasts every month or two, and who cuts directly over the lump instead of cutting around the areola (circumareolar incision which is the best way to hide the scar) and uses large interrupted sutures. A friend had that happen to her and had to have a plastic surgeon revise the scar.
0 -
Can you post the complete mammo and the complete US reports?
0 -
Sure. Thank you!
MG Digital Diagnostic Bilateral with TOMO with CAD, US Breast Bilateral Complete
Clinical History: Dense breast parenchyma. Family history includes breast cancer in grandmother. Gail score 9.9%
Comparison: Prior studies dated 2/20/2013 through 02/18/2019
Technique: Craniocaudad and mediolateral oblique views of both breasts are digitally acquired. 3D tomosynthesis was performed. C-view technology was utilized. Images are reviewed with the R2 Image Checker CAD system. Breast ultrasound was performed.
Findings: The breast are composed of heterogeneously dense fibroglanduar tissue, category C, which may obscure small masses. There is no suspicious mass, calcification or architectural distortion. There are no skin thickening or nipple retraction and no evidence of abnormal axillary adenopathy.
Ultrasonography to include the entirety of both breasts, all 4 quadrants, the retroareolar zone and both axilla is performed.
-a hypo echoic area with slight irregularity and increased color flow at the 3:00 position of the left breast, 4 cm from the nipple is no appreciated. This is an indeterminate nodular density. Ultrasound guided biopsy is recommended.
-Cysts on the right at 1 and 6 measure up to .5 cm each
-There is no suspicious axillary adenopathy
Impression: Indeterminate nodular density left breast, 3:00. Ultrasound guided biopsy is recommended.
BI-RADS: 4C
0 -
So from the MRI they can't say I'm high risk? That sounds good to me! Lets get this thing out of my body!
0 -
The abnormality is poorly described in the report. No size is given, no mention of shadowing or through transmission, they use the word "area" and not mass so not I'm sure what to make of this. They made it a 4c so they must be concerned. Let us know what happens.
0 -
Thank you for taking the time to read the report. I thought it was weird. I will let you know when I find out!
0 -
thanks, djmammo. glad I went to the right surgeon!
0 -
djmammo - just a quick question as to Aviva's experience.
I may be incorrect, but I did not think the radiologist usually talks to the patient. The reports are done for the requesting doctor, and that doctor is the one to speak with the patient. In my experience, if you have a radiologist who takes the time to sit down with you and explain what they saw & why - you have a real gem.
Edited to say - am I misinformed?
0 -
DJMAMMO: Final reports from today. I guess what concerns me is intramammary lymph nodes. Because for 3 years I have complained about them. They swell Then move to my armpit then my breast will start itching and go away. Also, it is normal For the area to grow 1 mm the original mammogram had it at 6 mm thank you for your time
Mammogram: MAMMOGRAM FINDINGS: Spot compression images in the CC and MLO
projection demonstrate a persistent 7 mm circumscribed mass in the 12:00 subareolar region. This is believed to correspond with a benign-appearing intramammary lymph node on today's ultrasound. No suspicious finding is noted.
ULTRASOUND FINDINGS: Targeted ultrasound of the right breast in the 12:00 subareolar region demonstrates a 7-8 mm oval hypoechoic nodule with central echogenicity most consistent with an intramammary lymph node. No suspicious finding is noted. A benign-appearing
calcification is seen in the 2:00 axis.
IMPRESSION: BI-RADS 2 or 3
RECOMMENDATION: Continue routine annual mammographic screening
Ultrasound: Spot compression images in the CC and MLO projection demonstrate a persistent 7 mm circumscribed mass in the 12:00 subareolar region. This is believed to correspond with a benign-appearing intramammary lymph node on today's ultrasound. No suspicious finding is noted.
ULTRASOUND FINDINGS: Targeted ultrasound of the right breast in the 12:00 subareolar region demonstrates a 7-8 mm oval hypoechoic nodule with central echogenicity most consistent with an intramammary lymph node. No suspicious finding is noted. A benign-appearing
calcification is seen in the 2:00 axis. IMPRESSION: BI-RADS 2-benign findings.
RECOMMENDATION: Continue routine annual mammographic screening as per ACR guidelines, monthly self breast examination, and annual clinical examination by a physician unless signs and symptoms prompt earlier evaluation.
0 -
djmammo,
My primary doc called today to say I need a biopsy after results of initial mammogram and ultrasound. It's my first mammogram to date. I stopped by and picked up a copy of the ultrasound report. I'm assiduously avoiding googling beyond this site, but I'd sure appreciate any help making sense of this report...maybe more realistically looking for reassurance that it's not very worry-worthy. 🤔 Besides...wth is a plantar? wider?
Findings:
Just lateral to the right nipple is a well defined plantar (sic) than tall lobulated solid heterogeneous dense nodule with prominent inferior marginal vascularity. 2.9x1.9x1.4 cm.
3 other much smaller similar appearing not significantly vascular nodules are present.
1:00 position .9x.7x.6 cm
11:00 position, 1x .8 x .5 cm
9:00 position, .8 x .5 x .5 cm
dense breast: no
Birads 4
I'm soon to be 51, no menopause yet!
0 -
If what MinusTwo says is true, it seems like a bad way to do things. The radiologist understands his results a lot better than the referring physician who is just my primary care physician. This isn't her specialty. I'm not sure she understands this stuff much better than I do. I retrieved the results from the patient portal before my PCP even got them and called my PCP myself with the results and emailed them to her. I think the radiologist just sends her a report though with those same results. I don't think he would talk to her unless she makes the effort to call him, which why not just talk to me directly in that case? There is a doctor to doctor phone line on the report my PCP gets, but me asking her to call him for her to get his opinion to then call me just seems ridiculous.
0 -
I was surprised last week when the radiologist actually came talk with me. When the tech left the room saying I’m going show HIM and I’ll be back. Little later he came back in with her to look at the ultrasound and get her to do a little more and take measurements. Then tookthe time to talk with me and explain what he thought the lump was that the doctors were feeling.
0 -
In every place I have practiced the breast radiologist always spoke to the diagnostic patients after all their studies were reviewed and compared. They were told the findings, the recommendations, and all their questions would be answered. On the rare occasion of a shortage of staff, I would have the Nurse Navigator speak to the pts with a negative or completely benign study and offer them the opportunity to wait to speak to me if they weren't in a hurry to get somewhere. Then again I am one of a small community nationwide that does nothing but breast imaging and I chose to practice in freestanding breast centers associated with a major hospital instead of just a mammo section within an xray department in a small community hospital. All were ACR Breast Imaging Centers of Excellence and centers such as that in your area can be search on line.
0 -
Intramammary lymph nodes are common and normally found in the breast. As long as their cortex remains normal in thickness over time they are left alone. As far as a 1mm difference is concerned you could measure it on two different machines on the same day or have it measured by two different techs on the same machine the same day and get a 1mm difference.
0 -
I'm going to go out on a limb and say that "plantar" is a voice recognition error (typo). In context the intended phrase was probably "wider than tall" which is in general a benign feature when describing a solid mass. A bad sign would be "taller than wide". If I remember correctly "plantar" refers to the bottom of the foot.
I would call and ask them to correct the report. That is an important feature and should be made clear .
0 -
Thank you, I'll do that. So glad it is a benign sign! Any insight into why I need to see a general surgeon before the biopsy? The radiologist suggested an us guided biopsy...the rad would do that wouldn't he? I think I'm not worried but then get lightheaded and realize I'm fretting more than I thought.
0 -
I have practiced in places where they require a visit to their fellowship trained breast surgeon on staff prior to a biopsy just so that you are already a patient of theirs and they are familiar with your case in the event you need surgery. Surgeons like this who do nothing but breast surgeries usually leave the least noticeable scars.
Yes the radiologist is they one that usually performs the image guided biopsies since they are the ones that do more of these procedures per year than anyone else.
0 -
ok, I 'll just hope it's a fibroadenoma and doesn't need surgery. Thank you.
0 -
In looking up "ACR Breast Imaging Centers of Excellence" both the center where I got the initial screening/follow-up needle core biopsy and the place that the surgeon practices where I got the excisional biopsy are listed. Sounds like not all of them are the same in terms of patient communication. I might try and switch to the place my surgeon practices and see how that goes. The staff there seemed nice and when I got a scavi scout put in, the radiologist and technician gave me a card with their info. The other place where the radiologist didn't call me back never did that. I had to get his info from the patient portal.
0 -
Good morning

I am quite confused over the report from the radiologist. At the end of the appt on the 17th, he told me there was no US correlate. Now apparently there is. His report lacks information in my opinion and seems contradicting. No comments on margins or density or shape seen on US. And he got my age wrong also lol
Ultrasound from a year ago showed no abnormalities in my left breast.
I am debating pushing for a second opinion and look at the images, both past and current. As i feel his interpretation is bias (he has always disregarded me with comments i am too young and even after this last appt, he was incredibly nonchalant and dismissive).
Looking for a second opinion of his report to make sure i am not overthinking or overreacting in any way. I do have pictures of the most recent mammogram as they let me see them while i was waiting.
Biopsy is scheduled for the 3rd.
Thank you so much for your time.
Impression
1. Stable right mammogram with no evidence of malignancy identified.
2. Somewhat suspicious mammographic and sonographic findings left breast at 1:30 position; see details/discussion above and suggest ultrasound-guided core biopsy for diagnosis.
3. Findings and recommendations discussed with patient and relayed to Dr. Avena's office staff. Patient will be scheduled for biopsy procedure.
These results and recommendations were communicated directly to the patient.
BI-RADS CATEGORY 4: Suspicious.
Exam images have been permanently archived.Narrative
PROCEDURE: MAMMO DIAGNOSTIC TOMO W CAD BILAT, US BREAST LEFT
REASON FOR STUDY: 47-year-old female with history of benign core and excisional left breast biopsies for follow-up of probably benign findings left breast and annual examination. Patient reports recent identification of left upper outer breast
lump/fullness.
CLINICAL HISTORY: Patient with no reported family history of breast carcinoma. History of ovarian carcinoma in mother at age 42.
COMPARISON: 7/30/2019 and earlier.
TECHNIQUE: Digital mammography with 3D tomosynthesis was performed. Diagnostic images of both breasts were obtained. Additional left laterally exaggerated CC view was performed. This study was interpreted with the benefit of an R2 computer-aided
detection (CAD) system. Limited left breast ultrasound was also performed.
FINDINGS: The breasts are heterogeneously dense, which may obscure small masses.
Some minimal distortion is again noted in the left mid outer breast region in area of prior excisional biopsy. In the left deep upper breast on MLO view, projecting over the pectoral muscle, there is an oval-shaped area of asymmetric parenchymal density
identified. This appears to lie in the deep outer breast on exaggerated CC view. This was not noted on study of 12/2017. It is more apparent than on studies of 1/2019 and 7/2019. Tomo images demonstrate no worrisome calcification or distortion and given
current mammographic appearance alone, an island of normal asymmetric tissue is a consideration. Apparent interval mammographic change, however, does raise concern. There are some additional areas of subtle stable asymmetry. There are a few small
benign-appearing rounded calcifications. No definite discrete concerning mass, worrisome calcifications, or other secondary signs of malignancy are noted. No significant change is noted on the right.
Limited left breast ultrasound was performed. Real-time examination was performed. In the left breast at the 1:30 position, 7 cm from the nipple, images demonstrate a flattened heterogeneously hypoechoic solid appearing entity which measures
approximately 2.2 x 1.5 x 0.5 cm and corresponds to area of patient concern. Subtle palpable abnormality is noted in this area and this is felt to likely correspond to the asymmetry in this area on mammography. Sonographic appearance is similar to
heterogeneous breast tissue noted elsewhere in this patient, however, palpable nature and apparent mammographic change does raise some concern. Other solid breast masses/processes cannot be entirely excluded. No worrisome blood flow, acoustic shadowing,
or other concerning features are noted. No other significant abnormalities are identified.
Further diagnostic options including continued close interval follow-up and ultrasound-guided core biopsy were discussed with patient. Patient prefers ultrasound-guided biopsy at this time and this seems a reasonable approach.0 -
First of all if there are ANY inaccuracies in the report ask them to correct them now, and reissue the report prior to your biopsy appointment. Let's make sure this is your report.
Second, the dimensions make this more oval than round and that leans more toward the benign side of things.
Third when you call to have the report corrected ask them to include the following information: a) Is the "flattened entity" parallel to the chest wall? parallel is good b) Does it have internal flow on Doppler? no flow or minimal flow is good c) Was there any "posterior shadowing" or "through transmission" noted when scanning the mass? through transmission is good.
These questions may make them a bit more careful next time.
0 -
thank you so much for your reply. I am happy to know it is lacking important information as i thought. Especially happy to have guidance and what to ask for specifically.
Do islands of regular breast tissue typically present as solid "entities " on an US? To my non professional knowledge, i thought it would show normal breast tissue in an US.
0 -
"Do islands of regular breast tissue typically present as solid 'entities' on an US?"
No. I think "entity" was used because they were hesitating to say "mass" but who knows.
For now, take it as a win as it didn't say "irregular shadowing mass with internal vascularity".
Keep us in the loop.
0 -
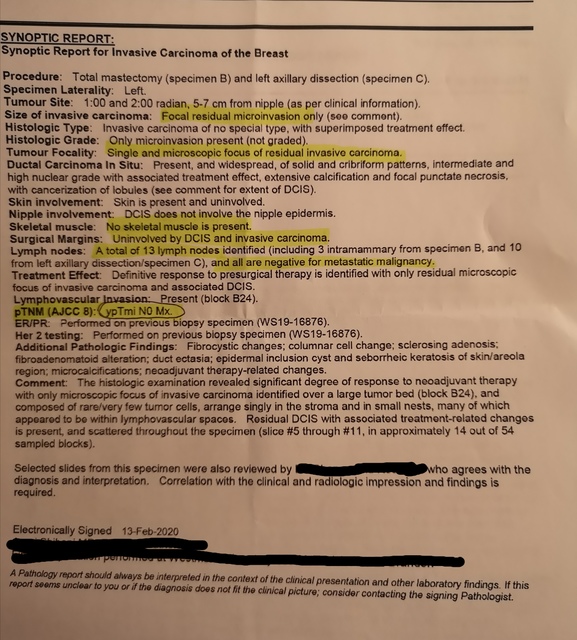
I had dose dense neo adjuvant chemo (4 AC and 4 T) started in September 2019 and a left side total masectomy and axillary node dissection on January 30, 2020. I have just received my pathology report, and though my surgeon seemed quite pleased with the report, the more I read it, the more I worry about what it means.
I had 2 tumors that responded well to the chemo, but I didn't get a complete response. I had only 1 lymph node biopsied before chemo and it was positive so my surgeon decided to do an axillary node dissection.
Any info you can provide would be super helpful. I don't meet back with my oncologist until March 12 to decide the next part of the plan, which I'm assuming will include radiation. Hoping for no additional chemo.
I will try to add a photo of part of my report, as I don't have an electronic version.
Thanks very much for any further clarification you may be able to provide.
 0
0