Will 30% of Early Stage (1-IIIA) go on to metastasize??
Comments
-
Thank you! I definitely didn't see the treatment options before .. very helpful. And thank you for the Oncotype explanation. This has definitely perplexed me. I never knew if the "9" would go up to something much higher. Before my ALND my MO told me I had an > 80% likelihood of additional lymph node involvement. I think at that point (4+ nodes) the Oncotype may not have been valid. I was lucky enough to have none of those additional nodes test positive. He said he would place more weight on the Oncotype from biopsy if I stayed at 3 nodes.
0 -
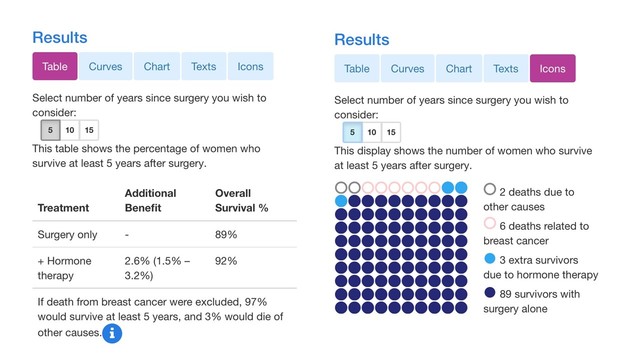
5 yrs:
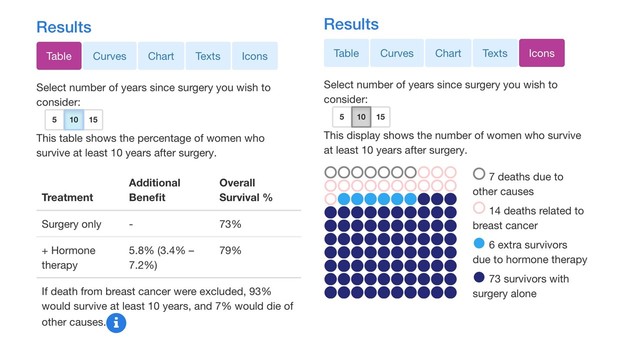
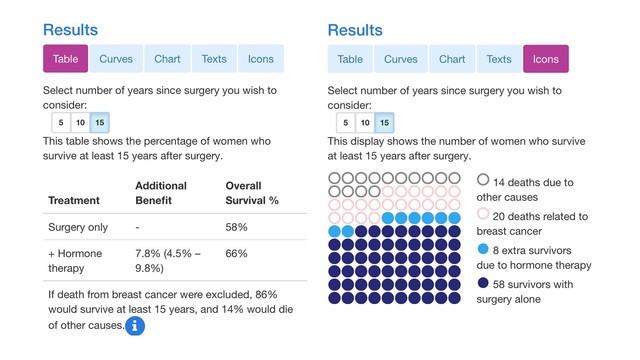
+ Hormone therapy 2.6% (1.5% – 3.2%) 92% 10 yrs:
+ Hormone therapy 5.8% (3.4% – 7.2%) 80% 15 yrs;
+ Hormone therapy 7.8% (4.6% – 9.8%) 68% I hate stats, mostly because I too have a hard time understanding. My GP said to me local recurrence usually occurs in the 1st 3 years. As we can tell from our fellow posters here, the distant mets seem to occur years later. Not all but most.
I've played around with the predict tool as I just want to know overall survival. Right now I'm at 92% which is wonderful, but why is my therapy only giving me 2.6% added benefit, yet in years to come the added benefit percentage goes up, but survival goes down (which I realize age has alot to do with that). I was 56 when diagnosed. I don't know my Ki67. Doing 10 yrs therapy adds 1% to OS.
I can never figure out the criteria either. This tool isn't for the "in situ" people? Only an invasive tumor? I have an "in situ" on each side so that's not considered bilateral disease? I think not, but reading that made me ask. TIA
0 -
Exactly because of all the recent & continuing GREAT informative posts - I don't want to see the thread disappear. It's a question after all. People can open & read to find the answers - old & new - will it or not? Maybe a bit of a shock will prod them to learn more. Personally this thread has been in my favorites forever. I'm interested in the historical changes of the disease over time & I like seeing Susan's Garden and some of the other older members.
0 -
ctmbsikia,
"why is my therapy only giving me 2.6% added benefit, yet in years to come the added benefit percentage goes up, but survival goes down"
The reason why you get added benefit from the therapy over time is because the risk of a metastatic recurrence spans 15 to 20 years (or even longer), so the amount that hormone therapy reduces this risk over 5 years will be less than the amount that it reduces this risk over 10 years or 15 years.
For example, if 10 years of hormone therapy reduces metastatic recurrence risk by 30% over the 10 years that the patient takes the meds, plus an additional 5 years beyond that (i.e. the patient sees a consistent risk reduction benefit for 15 years), you might see numbers something like this:
- Risk of mets at 5 years without hormone therapy: 6%
- Risk reduction benefit from hormone therapy at 5 years: 2% (a 30% reduction of the 6% risk)
- Risk of mets at 5 years for someone taking hormone therapy: 4%
.
- Risk of mets at 10 years without hormone therapy: 12%
- Risk reduction benefit from hormone therapy at 10 years: 4% (a 30% reduction of the 12% risk)
- Risk of mets at 10 years for someone taking hormone therapy: 8%
.
- Risk of mets at 15 years without hormone therapy: 15%
- Risk reduction benefit from hormone therapy at 15 years: 5% (a 30% reduction of the 15% risk)
- Risk of mets at 15 years for someone taking hormone therapy: 10%
.
As for why survival is going down over time, this is because the figures you are looking at reflect Total Survival. As we get older, there are more things that are going to get us. So the numbers you are seeing aren't just Breast Cancer Mortality but All Cause Mortality.
I mentioned above that the Icon view is the easiest to understand. I went into PREDICT and played around with it to come up with results that almost perfectly match the numbers you mentioned (the 15 year numbers are off just a bit). Here are the two views of the same results, the first being the Table view that you were looking at, and the second being the Icon view. I think you will find the Icon view to be much clearer. I've got the 5, 10 and 15 year results.
Lastly, PREDICT doesn't include in situ conditions (DCIS or LCIS) because technically the mortality risk from these conditions is 0%. It is true that the overall mortality rate from DCIS is not 0%, but generally a DCIS patient will have a local invasive recurrence prior to the development of mets. Since PREDICT doesn't measure local recurrences, the model therefore cannot reflect the presence of DCIS (or LCIS).
Edited to correctly name the first view from PREDICT as the "Table view" rather than the "chart view", in paragraph above.
0 -
"As for why survival is going down over time, this is because the figures you are looking at reflect Total Survival. As we get older, there are more things that are going to get us. So the numbers you are seeing aren't just Breast Cancer Mortality but All Cause Mortality.
I mentioned above that the Icon view is the easiest to understand. I went into PREDICT and played around with it to come up with results that almost perfectly match the numbers you mentioned (the 15 year numbers are off just a bit). Here are the two views of the same results, the first being the chart view that you were looking at, and the second being the Icon view. I think you will find the Icon view to be much clearer"
As always Beesie, thank you. I did not know that tool is all cause mortality.
0 -
This thread is very informative and I bookmarked it soon after I joined this site some seven plus years ago. I notice however, my own perception and interest in prognostic type of information continues to godown as the time moves on. Purely psychological thing I guess. But at this point in my life, I absolutely don’t care which bucket of survival stats I fall under. I guess it’s a good thing. 😆
0 -
Here's a question for you, Beesie (or anyone else willing to help me dig into the stats).
As you can see by my stats, I had more than one kind of cancerous or precancerous cells. Five kinds to be exact, including triple negative IDC and ILC. They found seven tumors, spread across both breasts. I also had a single node with micrometastases. My KI67 was 95%. I did BMX and 11 months of neoadjuvant and adjuvant chemo, but no radiation or hormone therapy.
How the heck do I even begin to calculate my reoccurrence risk? I've tried more than once and gave up in frustration each time.
Any suggestions?
Trish
0 -
Trishyla, I *think* you go with the most serious one - which my guess would be your tnbc grade 3 IDC. Your chemo is 3rd gen. You could also see what each of them comes out to individually. I don't know if the risk is additive or increases due to multiple tumors of different pathology - that's something I'm guessing we don't have a lot of data about. Did your MO go over recurrence risks at all?
0 -
Trishyla, what I'm about to tell you is utterly UNscientific and will probably have Beesie choking on her coffee. But here is how I have pondered things, the things I have taken into consideration when assessing my risk. Or rather, these are the issues I looked at to try and form an overall picture of my 'situation'.
First, I had an Oncotype. 11. This seems to be the high end of the low range. My oncologist felt that chemo would be pointless and more damaging than beneficial in the face of this score. BUt there were other things that I feel (purely personal ) contribute to the picture. My age and menopausal status at time of diagnosis. Overall it seems the younger you are, the worse off you are. Breast cancer seems, in younger women, to sometimes be a different beast. I was not young. I was 53. But I was not in menopause. I was having regular periods. So I wasn't old enough to be on the 'good' side of menopause, but I wasn't exactly young either. So... not sure how to feel about that. AGE was something I looked at. MENOPAUSAL status was something I looked at.
Size of tumour was something I looked at. Mine was 2.5 cms. Not small. Larger tumours seem to have worse overall outcomes. (I can hear Beesie rolling her eyes at me, sorry!)
Vascular invasion was something I looked at too. My surgeon only found one, lone, pitiful lymph node. She said she looked, she dug, she cut deeper, I had no lymph nodes that showed up and one is not considered a very good sample. She yanked out some vascular type bits just to have something more to submit for testing. The one node was clear. But I have always wondered if she'd got more, if they might have shown cancer? But the pathology report said no sign at all of lymphovascular invasion. This is one thing I considered when trying to decide my situation.I looked at whether or not my tumour showed necrosis. Necrosis means the cells in the tumour have died off, most likely for lack of food and when that happens the tumour grows and goes off searching for a food supply. This is vascular invasion, when the tumour starts exploring other places to set up housekeeping. I had no necorsis, no invasion. So my tumour was bigger than I was happy with, and I was younger than I could have been, but likewise the tumour seemed pretty happy where it currently was and hadn't apparently gone looking for a new place to live.
In trying to figure out how I feel about things, what my 'chances' are, I took ALL of these variables into account. It's a puzzle, put togehter the pieces, step back and assess the picture as a whole. An Oncoscore is a big piece of it but not the only piece of it. Hope this helps. Apologies to Beesie!0 -
Thanks for the very thoughtful replies, moth and runor. I did initially use my triple negative tumor as my guide. With that, taking into consideration my age at diagnosis, 58, my TNBC tumor size, 2.5cm and my lack of node involvement on that side, I had a 5 year reoccurance rate of about 38%.
Taking the oral chemo, Xeloda, reduced my rate to under 20%. Yay! Kinda. With TNBC the likelihood of having a distant reoccurrence, metastasis, is extremely high. So, boo. But your risk after five years drops to about 8%. The same as the general population. Yay?
Which brings me to my current dilemma. I'll hit my five year mark 8/29/21. So then TNBC recedes into the background as a risk But my ER/PR positive cancer will just be starting to gear up for reoccurrence/metastasis. I've refused hormone blockers up to this point because of horrendous side effects, and because they do nothing for my highest risk cancer, the TNBC. I need to know how to calculate my reoccurrence rate from that point forward to see if hormone blockers are worth it. And I have no idea how to go about it.
Any ideas?
0 -
Trish that tool isn’t for bilateral disease. There’s no way to plug it all in.
I’m all for trying to understand and I appreciate all I’ve learned here. I’m not uncommon but mixed type cancer which is better than straight IDC Er+ but I’ve read a study that it has a higher percent of 2nd primary. Hopefully years down the road when I’m dead from another cause. To have a 4 cm tumor with ductal and lobular features with one node a micro met - that sucker was in there growing for quite a while. For me, the only reason it wasn’t found earlier is because i was never screened!! I’m lucky and I hope fear of it appearing again will keep getting better with time.
Thanks for the thread. Interesting stuff.
0 -
Trishyla, there's not much I can add to what moth and runor have said. There is not a lot out there on situations like yours, and what is out there isn't clear and consistent.
As moth said, my understanding is that when there are multiple tumors, prognosis is based on the largest/most aggressive tumor. But there is concern that this might under-estimate risk. However adding together the tumor sizes appears to over-estimate risk. No easy answer. My question is the same as moth's - did your MO talk to you about your recurrence risk?
Multicentric Breast Cancer, Multifocal and Contralateral Breast Cancer https://breast-cancer.ca/multi-tumrs/
Review on Practical Approach in Multiple Breast Carcinomas: Does Each Focus Matter? https://www.revistachirurgia.ro/pdfs/2017-4-418.pdfThe prognosis of bilateral breast carcinoma compared to unilateral breast tumor. 5- and 10-year follow-ups https://pubmed.ncbi.nlm.nih.gov/7740408/
Multicentric and multifocal versus unifocal breast cancer: is the tumor-node-metastasis classification justified? https://pubmed.ncbi.nlm.nih.gov/20454925/
runor, no apologies necessary. I am neither choking on my coffee (my wine, actually; I just can't drink coffee after noon or it keeps me awake at night), nor am I rolling my eyes. Everything you wrote makes perfect sense to me. It's not all about stats. Clinical and pathological factors are very important. It's why I take Oncotype scores with a grain of salt and why I often suggest the people ask their MO to run the Oncotype RSPC model, which adjusts Oncotype recurrence risks by incorporating patient age and clinical/pathology factors.
**Trishyla, I just saw your latest post as I was finishing off this post. This might not make sense (and statisticians might roll their eyes), but can you use something like the PREDICT model and input your largest ER+/PR+ cancer, and look at the 5 year and 15 year results? If you subtract the 5 year results from the 15 year results, this might tell you what risk you face from your ER+ cancer from next year (year 5) through the next 10 years. Maybe ask your MO if something like this would be a reasonable way to assess your future risk?
0 -
Question on a tangential topic: what percent of women (with "Western" diets and ethnicity, as US and Canada) are diagnosed with breast cancer in their lifetime? I have long seen a number that was about 12%. But does that include women diagnosed with "Stage 0" forms such as DCIS and LCIS? Or only those with invasive forms?
Thanks in advance for any insight.
0 -
Great question MountainMia. I hope Beesie will chime in.
0 -
ha. I answered my own question:
- About 1 in 8 U.S. women (about 12%) will develop invasive breast cancer over the course of her lifetime.
And because the info is good, I'll copy and paste it here.About 1 in 8 U.S. women (about 12%) will develop invasive breast cancer over the course of her lifetime.In 2020, an estimated 276,480 new cases of invasive breast cancer are expected to be diagnosed in women in the U.S., along with 48,530 new cases of non-invasive (in situ) breast cancer.About 2,620 new cases of invasive breast cancer are expected to be diagnosed in men in 2020. A man's lifetime risk of breast cancer is about 1 in 883.About 42,170 women in the U.S. are expected to die in 2020 from breast cancer. Death rates have been steady in women under 50 since 2007, but have continued to drop in women over 50. The overall death rate from breast cancer decreased by 1.3% per year from 2013 to 2017. These decreases are thought to be the result of treatment advances and earlier detection through screening.For women in the U.S., breast cancer death rates are higher than those for any other cancer, besides lung cancer.As of January 2020, there are more than 3.5 million women with a history of breast cancer in the U.S. This includes women currently being treated and women who have finished treatment.Besides skin cancer, breast cancer is the most commonly diagnosed cancer among American women. In 2020, it's estimated that about 30% of newly diagnosed cancers in women will be breast cancers.In women under 45, breast cancer is more common in Black women than white women. Overall, Black women are more likely to die of breast cancer. For Asian, Hispanic, and Native-American women, the risk of developing and dying from breast cancer is lower. Ashkenazi Jewish women have a higher risk of breast cancer because of a higher rate of BRCA mutations.Breast cancer incidence rates in the U.S. began decreasing in the year 2000, after increasing for the previous two decades. They dropped by 7% from 2002 to 2003 alone. One theory is that this decrease was partially due to the reduced use of hormone replacement therapy (HRT) by women after the results of a large study called the Women's Health Initiative were published in 2002. These results suggested a connection between HRT and increased breast cancer risk. In recent years, incidence rates have increased slightly by 0.3% per year.A woman's risk of breast cancer nearly doubles if she has a first-degree relative (mother, sister, daughter) who has been diagnosed with breast cancer. Less than 15% of women who get breast cancer have a family member diagnosed with it.About 5-10% of breast cancers can be linked to known gene mutations inherited from one's mother or father. Mutations in the BRCA1 and BRCA2 genes are the most common. On average, women with a BRCA1 mutation have up to a 72% lifetime risk of developing breast cancer. For women with a BRCA2 mutation, the risk is 69%. Breast cancer that is positive for the BRCA1 or BRCA2 mutations tends to develop more often in younger women. An increased ovarian cancer risk is also associated with these genetic mutations. In men, BRCA2 mutations are associated with a lifetime breast cancer risk of about 6.8%; BRCA1 mutations are a less frequent cause of breast cancer in men.About 85% of breast cancers occur in women who have no family history of breast cancer. These occur due to genetic mutations that happen as a result of the aging process and life in general, rather than inherited mutations.The most significant risk factors for breast cancer are sex (being a woman) and age (growing older).0 -
Another thing I wondered about was the number of women diagnosed with non-invasive DCIS or LCIS. This answer is from another bco page:
"There are about 266,120 new cases of invasive breast cancer and 63,960 cases of non-invasive breast cancer this year in American women. " https://www.breastcancer.org/risk/factors/woman
0 -
Since this thread popped back up, I want to thank everyone who answered my query about how to calculate my risk. I think you're right, Beesie. I have to treat them as separate cancers, and run the numbers consecutively rather than concurrently.
0 -
So, I know some people will be grinding their teeth about this thread being bumped up but I was JUST sent this Medscape article and I have to say..... I was thinking that 30 was a big over-estimate but now I'm doubting myself on that.
Have we talked about this yet? I didn't see it on the thread but maybe I just missed it https://www.medscape.com/viewarticle/849644#vp_1
"The Mystery of a Common Breast Cancer Statistic"
"Dr Brawley worked with two ACS epidemiologists to examine the issue. They looked at breast-cancer-specific mortality (as identified on death certificates) in 12 health districts in the United States from 2008 to 2012. They were surprised by the finding: "28% of the women who died of breast cancer during that time period had localized disease at diagnosis," said Dr Brawley.
The result was unexpected. "We all thought 30% was too high," said Dr Brawley." (it's on page 3 of the Medscape article).
So.... that's a surprising turn of events for me. Maybe 30% is not wrong after all? I wish we actually had more numbers on this. It seems absurd that we don't.
0 -
Moth, you are right. I was told from my MO that my recurrence rate is 30% with 3mm cancer and 2 nodes positive. That's why I get worried when I have strange pains in strange places.
0 -
Moth, I think it's important to keep everyone informed! I was stage 1, node negative, oncotype score of 23 in 2008 (44 years old, no family history). At that time, that oncotype score was in the "gray area" to determine if there was a benefit from chemo. I did do chemo - weekly CMF chemo for 6 months, lumpectomy/radiation and 7 years of femara. I was told that all this treatment brought my risk to around 10% (or even less?) of having a recurrence yet - here I am, dx stage IV 11 years later (10 years after radiation was complete - almost to the day). Personally, I wonder if I had stayed on femara longer would I be here but who knows? At the time, I was told that my risk from bone loss/osteoporosis was greater than my risk of a breast cancer recurrence so they had me stop taking it after 7 years.
0 -
Yup, I'm grinding my teeth that this thread has yet again been resuscitated.
I don't think anyone has disagreed that the 30% stat used to be correct. But it's not correct anymore. That's the reason why this thread should be left to the archives.
What we have to remember when we look at mortality data is that there is a time lag. moth, the article you've linked is from 2015, and it looked at cause of mortality for women over the period of 2008 to 2012. So these are people who died during the period from 9 years ago to 13 years ago. These women died of breast cancer during this time, but they had started off with a localized diagnosis. So when were they first diagnosed and treated? Since the 5 year survival rate of those with a localized diagnosis is in the high 90% range, and since most people survive 2-3 years with mets, with some exceptions, the most recent diagnosis dates would be between 2001 to 2005, i.e. 16 to 20 years ago. Of course for many with early stage disease, particularly those with ER+/PR+ disease, the time to mets is longer, sometimes as long as 15 or even 20 years. And the length of survival after the diagnosis of mets is also longer for many patients. This means that some of those who died of metastatic breast cancer between the years of 2008 and 2012 might have been diagnosed as long ago as 1988, if not earlier. In other words, for the most part this study reflects what happened to those diagnosed with breast cancer somewhere between the years of 1988 and 2005.
Having been diagnosed in 2005, just from my observations I can say with 100% certainty that treatment has changed, and survival rates have improved since that time. Just for a start, there is Herceptin, there is the broad use of Tamoxifen for early stagers, there is approval of AIs for early stagers....
So let me again copy and paste the information I provided previously, which compares current rates of metastatic recurrence to the rates during earlier time periods, such as the time period covered by the study linked above:
"The observed fifty percent relative decline in distant breast cancer recurrence over time may be related to both improved treatment for initial disease at diagnosis decreasing recurrence risk (hormonal therapy, polychemotherapy, dose-dense chemotherapy, taxanes, and trastuzumab) and stage shift to more early and less late stage disease at diagnosis with improved screening technology and screening program participation. Distant recurrent disease incidence decline over time differed by phenotypic characteristics. We observed a 70% decline in distant disease recurrence among hormone receptor-positive patients and a 50% decline among hormone receptor-negative patients over time. We observed a 60% decline in distant disease recurrence among HER2 positive patients from 1999 to 2006. The differential decline associated with phenotypic subtype creates a new profile of recurrent metastatic breast cancer with fewer HR and HER2-positive cases and relatively more TNBC cases. Ten-year cumulative incidence comparisons to accommodate the longer interval to distant recurrence among HR-positive versus HR-negative disease did not significantly differ from 5-year rates." Source: Examination of a paradox: recurrent metastatic breast cancer incidence decline without improved distant disease survival: 1990–2011https://link.springer.com/article/10.1007/s10549-018-05090-y
From Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990–2010, here's a graph showing, over 3 time periods, the percent who have developed recurrent MBC, by stage at time of initial diagnosis: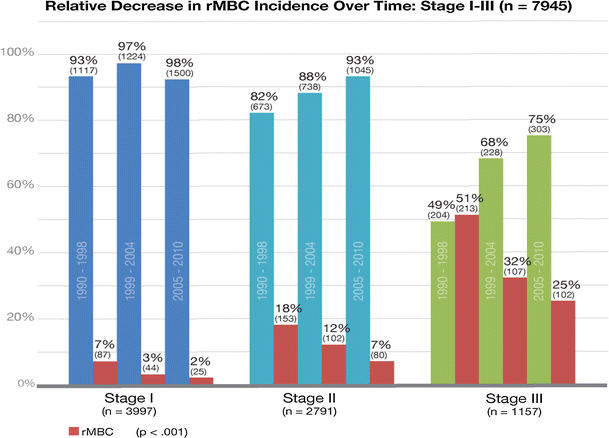
So, maybe 30% is not wrong after all? No, it is wrong. Once upon a time, for those diagnosed about 20-30 years ago, the 30% figure was correct. But for those diagnosed over the past 5 years and those diagnosed today, it is wrong.
aprilgirl, the problem with stats is that even when the stats are favorable, there will be those who fall on the bad side of the odds. Your risk of mets at time of diagnosis was estimated to be 10%. The fact that you developed mets doesn't mean that this original estimate was wrong - and that maybe your risk really was more in the range of the 30%. It only means that you had the crappy luck of being one of the 10 out of 100 who developed mets, rather than one of the 90 of 100 who didn't develop mets. I'm sorry you developed mets despite having a favorable diagnosis and doing all the treatments you could. Unfortunately that's the risk that we all face, even when the odds are overwhelmingly in our favor. But the flip side of that is that there are no doubt some people reading this who are facing a very high risk of recurrence, and yet fortunately some of them will never recur. To repeat the common saying around here, it's a crap shoot.0 -
Beesie - yes, I agree. One correction - I was told that my risk was 10% or less after completing treatment. I believe the risk without chemo was around 20%? Regardless, there are cases like mine, which does show that it is a bit of a crap shoot.
Thankfully, I am a good advocate and when I had a couple of odd symptoms for me , I pushed and pushed to get a CT (took me 2.5 months). I was repeatedly patted on the head and told I had a virus causing my "laryngytis" and other symptoms. I caught it fairly early, for stage IV and have so far responded well to treatment .
There is no way to predict if a stage 1 patient will be the 1 out of 10 to develop mets so I think it's important that all patients KNOW this and don't get complacent. I should not have had to fight to get a CT and have both my GP and Seattle Cancer Care Alliance dismiss my concerns because "your risk of recurrence is really low" and "insurance won't cover a petscan when it could be a virus" after I offered to pay out of pocket for the scan. Really frustrating.
0 -
Beesie, I was diagnosed less than 18 months ago and I was told from MO that my recurrence is 30% without letrozole and 15-20% with letrozole. I guess MO uses some other data when they come up with these numbers.
0 -
See I'm not convinced that 30 is wrong. Why did they get this result ". They looked at breast-cancer-specific mortality (as identified on death certificates) in 12 health districts in the United States from 2008 to 2012. They were surprised by the finding: "28% of the women who died of breast cancer during that time period had localized disease at diagnosis,"
This isn't 20-30 yrs ago so I don't get it.
0 -
aprilgirl, I couldn't agree more with your comment about those with low risk not becoming complacent. Everyone should understand that no matter how low their risk, it could happen to them. If they develop symptoms that could be suggestive of mets, get them checked out! My risk is low, but I remember going to my MO after I had a breast MRI that had an incidental finding of a spot on my spine. The description of the spot could have indicated something benign but it also could have described mets. My MO, who I hadn't seen in years, saw me very quickly but I could tell when I walked in that he wondered why I was there. But as soon as he read the report he became very serious. Fortunately it did turn out to be nothing serious. Yup, no one should think that low risk is no risk because that isn't the case at all.
LillyIsHere, did you have an Oncotype test done? Otherwise your MO might have used Adjuvant Online (not sure if that's the current name) or even PREDICT, which patients can access themselves. Have you used either PREDICT or CancerMath? Both are easy to use on-line models that estimate metastatic risk with and without various treatments
One thing I want to clarify. My beef is with the 30% figure as an average for all early-stagers, Stage IA to Stage IIIA. I simply do not believe that the 30% figure is accurate any longer, although I know when I joined here in 2005, the digging I did back then did seem to support the 30% figure. But a lot has changed in terms of breast cancer treatment over 15 years. However I am not saying that some early stagers might not have a risk that is 30% or even higher, and certainly those with more aggressive cancers may face risks in that range if they don't have chemo. My two issues with the 30% stat are that: 1) the 30% figure is outdated; I don't know what the current "average metastatic risk" would be for all early stagers, but I would guess probably closer to 20% than 30%; and 2) whatever the correct number is, an average risk figure that groups together such a huge population with such a wide range of diagnoses is completely meaningless for any one individual who wants to understand her own risk. This "average risk" figure is probably very useful for those planning breast cancer treatment resources and funding, and those assessing long term mortality trends, but it just doesn't apply to individuals.
moth, if someone diagnosed with early stage breast cancer died between 2008 and 2012 (between 9 and 13 years ago), when would she have been initially diagnosed and treated? How long is the time between diagnosis to development of mets to mortality? By my calculations (which are just my own estimates), I came up with the years between 1988 to 2005 for initial diagnosis (between 16 to 33 years ago). But even if everyone in the group passed away within 5 to 15 years of initial diagnosis, we would be looking at a group of people who were all diagnosed and initially treated between 1993 and 2007. My point about treatment advances and mortality reduction since those years doesn't change. The 30% figure was valid 10 years ago (the approx. time frame of the article) reflecting the treatment of those diagnosed 20 years ago. The 30% figure is not valid today for those diagnosed now, reflecting the treatment available today.
0 -
Thank you for your patience with us Beesie
 . In my case, I don't have an Oncotype number because it wasn't enough material for the test. The 3mm cancer tissue was sent out but came back as not enough tissue to be studied. However, MO at that time thought it was a low number of Oncotype because it is ILC. Yes, I tried PREDICT and it gave me amazing numbers, with or without letrozole it was the same extremely low recurrence. I wish I could go with PREDICT, I would have stopped letrozole immediately.
. In my case, I don't have an Oncotype number because it wasn't enough material for the test. The 3mm cancer tissue was sent out but came back as not enough tissue to be studied. However, MO at that time thought it was a low number of Oncotype because it is ILC. Yes, I tried PREDICT and it gave me amazing numbers, with or without letrozole it was the same extremely low recurrence. I wish I could go with PREDICT, I would have stopped letrozole immediately. 
Thank you for all the info here and other forums.
 0
0 -
I know I haven't spent as much time immersing myself in this literature as some of you, but I am a biostatistician by training.
When I first started getting up to speed ~4 months ago, I had a hard time reconciling all sorts of seemingly contradictory stats that appear in reputable, peer-reviewed venues. I feel like I'm starting to have partial success at making sense of it all. Of course some of the ambiguity will never go away, because the different studies all have different strengths/weaknesses and are looking at things from a different angle.
I think the thing Beesie points out is really significant here, which is ... we can't really say what the lifetime probability of distant recurrence is for someone diagnosed today. By definition. Because the relevant population hasn't experienced enough follow-up for us to quantify it.
But we can put a bound on it because I'm quite sure that "we" are getting better at breast cancer detection and treatment. Someone diagnosed today is likely to be diagnosed at an earlier stage and receive a treatment that is more effective re: preventing recurrence than someone diagnosed 5, 10, or 20, years ago.
The math Beesie does about the year of diagnosis for those dying in 2008 - 2012 makes sense to me: they represent a population initially diagnosed at least 8 years ago and, in most cases, many more than 8 year ago. So I interpret the 28% from death certificates as an upper bound on the distant recurrence probabiliy for those diagnosed today. And probably a very pessimistic upper bound, i.e. the true number is substantially lower now.
0 -
(Also that figure makes me twitch (although it's very interesting and I basically believe it,). The bar for those diagnosed as Stage 1 from 2005 - 2010 is clearly wrong. It reports a proportion of 98% and therefore should be higher than all other bars. Clearly some glitch happened in this publication, which is of course going on all the time in these papers.)
0 -
So we're putting all the benefit on early detection? Because tamoxifen and herceptin came on board just before 2000 so those benefits should be seen in those earlier 2008-12 numbers, shouldn't they?
Perjeta is too new to show results yet but it's the only new early stage thing isn't it? Someone asked me on Twitter what else is new that would make us think things are better now? Same surgery, rads and chemo for early stage (I can think of new mets tx but not early stage).
0 -
mostly I'm just so so so frustrated that recurrent mbc is not being properly counted. We're sifting tea leaves here looking for signs. It's ridiculous
0