Will 30% of Early Stage (1-IIIA) go on to metastasize??
Comments
-
Hi Peregrinelady,
My oncologist at Johns Hopkins says no more than 4 glasses of wine a week. 2 glasses max, twice a week were actually his exact words.
0 -
My oncologist is still saying moderation - in everything
0 -
Peregrinelady---Both my MO and my BS offered the same advice. They said lose 10 pounds (which still wouldn't put me in normal BMI but pretty close), exercise 5 days a weeks for at least half and hour to 45 minutes ( I do 6 days a week for 45-60 minutes sometimes broken up throughout the day), eat "some" fruits and/or veggies every day, try for 8 hours of sleep in a dark-as-you-can-get-it room which helps with melatonin production and get Vitamin D levels up to good range.
As to Vit D, my levels were in the 20s as diagnosis despite an outdoor job which my BS attributes to heavy sunscreen use. He'd like it to be closer to the 70s. So he put me on 5000IU daily and I am now at 73. He's completely convinced that low Vit D levels contribute to BC and our increased use of sunscreen is the problem. He doesn't advocate sitting around in the sun of course but taking Vit D supplements.
As to getting "good" sleep, he advocates keeping a regular bedtime, sleeping in a very dark room (I use a sleep mask) and keeping the temperature low which promotes healthy sleep. I have a fitness watch which tracks and scores my sleep and I can attest to all these tips working very well!
As to the fruits and veggies, I am a terrible eater of the good stuff! I hate to cook and prefer that all my food come at me through a window!
 But I've gotten better and try to eat at least one big serving of a fruit and veggies every day even if it's nothing more that adding a bunch of lettuce to a sandwich.
But I've gotten better and try to eat at least one big serving of a fruit and veggies every day even if it's nothing more that adding a bunch of lettuce to a sandwich. Both of these doctors gave me percentage improvements for these tips. They said if my recurrence put me at about 7-8% then losing 10 pounds would cut that by 20% and exercising daily (ish) would cut that by another 30%. And the fruits and veggies, for me, would give another 20% and the Vit D another 20%. They put it all to paper for me and calculated that I would go from the 7-8% chance to about a 2-3% chance. And that would reduce my odds by more than if I continued on Tamoxifen for another 5 years!! I'll take those odds any day! Now none of this means they would EVER say not to do my 5 years on Tamoxifen. It's just an example of how much lifestyle changes can help with recurrence rates.
And as a last note, I no longer drink. Even before my diagnosis, I would only drink about half a dozen times a year. I had a total hysterectomy 2 years after BC and drinking makes my hot flashes so bad it's totally not worth it. But my best friend was diagnosed after going through a rough patch and drinking waaaay too much at night. I asked my docs about how that could have affected her diagnosis and they both said they think drinking more than a drink or 2 a couple of nights a week increases your risk by about 30-40%! They don't say quit totally but definitely would rather I didn't drink. So yeah, just another reason for me to not drink. Doesn't mean I'm giving up my chocolate though!! I just make sure it's 72% or greater cocoa just to make me feel a wee bit better for eating it!!
Sorry this is so long. Hope some of it helps!
0 -
Thanks, guys. Lala, thank you for the detailed answer. I agree about the vitamin D and the advent of sunscreen. I was drinking more than usual when diagnosed and have cut way back, but have considered stopping altogether. Good to hear what other oncologists are saying. Mine gives absolutely no recommendations at all.0
-
lala1...wow! I refused anti hormone therapy from the start and have always thought that weight loss and exercise reduces recurrence rates by about 40 percent. Now you are telling me that an expert in BC is saying 50 percent! I also have always thought that taking a drug that makes both weight loss and exercise difficult, if not impossible for some, is very contradictory. We all have to make our own informed decisions and I expect that, but this is very enlightening information! Thank you and good luck.
0 -
My oncologist recommends the Mediterranean diet. I think my survivorship plan spoke to alcohol, but at age 65, I don't plan to give up my handful of Sangria Margarita swirls annually so it's a moot point for me.
Lala1, this statement cracked me up!
As to the fruits and veggies, I am a terrible eater of the good stuff! I hate to cook and prefer that all my food come at me through a window!
Hey, I usually get a fruit cup at the Chick-fil-A or Jason's Deli drive-through lane. Doesn't that cancel out any bad mojo? 🤔
Seriously though, I wonder how those who were already living a super healthy lifestyle feel about information seeming to suggest that diet and exercise is a panacea? Not that anyone "deserves" cancer, but it must be especially frustrating to get it under those circumstances.
Lyn
0 -
yeah. There is no magic bullet. I know some big time exercisers who eat healthy mets. Blows my mind. It's a crapshoot bottom line.
0 -
rosabella- I turned 60 this past March. My whole life I've eaten healthy/no meat, avid runner, minimal alcohol and never had any issues with weight. I don't even like sweets. Therefore when I was diagnosed there really wasn't much I could change with my lifestyle. I was already doing everything that was recommended. I live the same lifestyle as I did prior to being diagnosed with cancer. My oncologist encourage me to have one glass of wine per evening. I don't even do that. I have a glass of wine when I feel like it. which is infrequent. I do believe being in excellent health helped me deal with my double mastectomy, chemo and h&p for a year. I worked through chemo and I power walk or ran almost every single evening. Within 8 days post BMX, I tied my drainage tubes to my oversized shirt and started walking. My oncologist encouraged me to power walk and start running as soon as I felt like it. Iran a 5K 6 weeks post op and the day after my second chemo I'm not Superwoman. Exercise keeps me sane. There were days I had to give myself a very stern talk to get off my ass and get moving. I had no issues with radiation. I do not lecture others about making drastic changes to their lifestyle because people are going to do what they're going to do. Dealing with cancer is Tough Enough. My Lifestyle works for me and hopefully each of you will find a balance that works for you. What I find very annoying is when acquaintances feel that they have to search for a reason as to why I would have cancer. There have been a few individuals who have told me, see. You've done everything right and you still have cancer. I've LED my life exactly the way I wanted to with plenty of mistakes along the way. It's easy for individuals to sort of blame others for their cancers. They must have drank too much, smoke, overweight, never exercised, etc. It really scares the hell out of healthy people when they find out I have cancer. I have always been the poster child for healthy living . My friends look at it if I can get cancer so can they. Reality check we all can get cancer . Sometimes it is just a bad hand. Most of the time I deal with stupid comments with patience and education. There are moments when I just look at them and say get real.
0 -
jo..... I am in the same boat. I eat healthy, am thin, exercise daily (did a half marathon during chemo...albeit a slow one), and still got BC...twice. We do all we can to reduce our risk, but many things come into play, and sometimes things just are the way they are. I also recovered from surgery quickly, and had an "easy" time with chemo. I don't know if it was lifestyle or luck, but I know the lifestyle surely didn't hurt!
0 -
My point of view is that living healthy can possibly give us an edge in avoiding cancer or in dealing with it if we get it. But it can’t overcome genetics. I think that many bc patients, especially the premenopausal ones, do have something genetic going on, even it it is unknown at this time.
0 -
Shetland, both my twin sister and I were premenopausal at diagnosis and that is exactly what the geneticist said. Not BRCA positive but will probably find some other genetic component down the line. Our father had pancreatic cancer, as well. His brother had colon cancer. Their mother had breast cancer, so obviously there were cancer genes on my paternal side.0
-
So true. We can't run from genetics.
0 -
Genetics are a tricky thing: my Mom just turned 96, last time she was at a hospital, was when she gave birth to me which as you can guess, was a while ago :-) Same longevity on my father's side of the family, no BC in close relatives. I actually think mutations accumulated during our lifetime might be the culprit too, not just the genetic profile inherited at birth.
0 -
muska- you are correct. We cannot just rely on genetics. My mother's side of the family live into their late 90s and early one hundreds with relatively good health. The females on my father's side also lived until their mid 90s. The men not so lucky. Most of the men were heavy smokers and heavy drinkers and they died before age 65. The man either died from lung cancer or liver disease. We are going back quite a few years before there was adequate research regarding heavy smoking and drinking.
0 -
the test objective is to show whether or not you need to take the 10 years of AI drugs instead of 5 years, but it also predicts risk of METS. Once you reach 4 years of AI drugs you can ask Onco to do test and submit to insurance. Insurance does not like to pay for a test this early to determine if AI drugs are needed for 10 years as by the time you reach almost 5 years on AI drugs they will have something new. I wanted to post my score which is 7.8 out of 1 to 10. I am high risk, but the test also showed another 5 years of AI drugs would not benifit me.
0 -
I am with you Lala High risk and no benefit from AI drug past 5 years. We are in a small group.. Most like 83% get a good score ... So I read the trials. they compared tumor cells in node negative patients. the study started to collect tumor samples in 2006 til 2009.. so they have the 10 year data on which patient ended up with METS, stage 4... distant reacurance.. They know the genetic make up of those tumors and compared our tumors to those who ended up with Mets to determine our score.. The trial did not get personal information on the patients so they do not know if they had Chemo or not. My only saving grace is I threw the book at this, I took chemo, radiation and I did all the AI drug no matter how awful I felt from them. I can only hope that I killed off any cells that may have spread to another area thru the blood, since I was node negative. I do feel like I have the grim reaper following me, but I keep fighting the thoughts in my head. I decided it will not put me down and I will not curl up in a ball and stop functioning. One thing I am doing is not concentrating on save big for retirement and started making more memories. taking trips more often.. I would hate to have this come up on me and here I sit.. all set for my retirement that I will never enjoy. So Live Large...
0 -
My BCI score is 9.1%. What other scores have people received?0
-
herb-- I hear ya! I've decided to live my life while I can....just in case.
 Hence the new little lake cabin I bought myself.
Hence the new little lake cabin I bought myself.  0
0 -
lala-Congrats on your lake house.
0 -
0
-
Metastatic BC--- ER/ PRs positive recurrence rates 50% 0-5 years and 50% 5-10 years. after 10 years risk is unlikely. on Her2 after 3 years they get an all clear. Triple negative no idea, they are lucky if they can find a chemo that will work on it...
0 -
Below are the rates for HER2+ cancer up to 2015. I think they have improved since then. But I certainly did NOT get an "all clear" after 3 years, even if I am NED. I had no mets and I am still on 6 month recalls with cancer antigen testing every 6 months also to watch the curve. I had imaging again this year 5 years after final chemo.
5-year relative survival rates for women diagnosed between 2009 and 2015:
- localized: 98.8 percent
- regional: 85.5 percent
- distant (or metastatic): 27.4 percent
- all stages combined: 89.9 percent
0 -
While over half of ER+/PR+ recurrences happen within the first 10 years, the risk of a metastatic recurrence continues for at least 10 years beyond that:
- Beyond 5 years: enduring risk of recurrence in oestrogen receptor-positive breast cancer https://www.nature.com/articles/s41571-018-0145-5#Abs3
"Women with early-stage oestrogen receptor (ER)-positive (ER+) breast cancer who receive standard endocrine therapy for 5 years remain at risk of distant recurrence for at least 15 years after treatment discontinuation."
"Oestrogen receptor (ER)-positive (ER+) breast cancer is at least as likely to recur beyond 5 years as it is before 5 years from diagnosis."
.
- 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years https://www.nejm.org/doi/full/10.1056/NEJMoa1701830
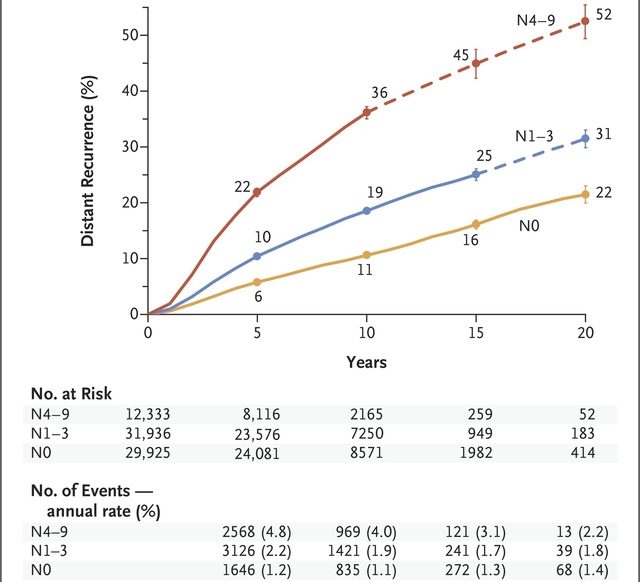
"Breast-cancer recurrences occurred at a steady rate throughout the study period from 5 to 20 years. The risk of distant recurrence was strongly correlated with the original TN status. Among the patients with stage T1 disease, the risk of distant recurrence was 13% with no nodal involvement (T1N0), 20% with one to three nodes involved (T1N1–3), and 34% with four to nine nodes involved (T1N4–9); among those with stage T2 disease, the risks were 19% with T2N0, 26% with T2N1–3, and 41% with T2N4–9."
For triple negative, the greatest risk of recurrence is within the first 3 years, and the risk drops off very significantly after 5 years:
- Analysis of pattern, time and risk factors influencing recurrence in triple-negative breast cancer patients https://link.springer.com/article/10.1007/s12032-012-0388-4
"The highest risk of recurrence was during the first 3 years after primary treatment, and then, during the next 2 years of observation, it did not change significantly (plateau after 3 years; Figs. 1, 2). In the study population, the risk of local relapse and metastases to the brain and lungs peaked in second year and then declined significantly, whereas the risk of metastases to the liver and bones was also the highest in the first 2–3 years but then fell slightly. Furthermore, 5 years after initial diagnosis new metastases occurred only in bones. However, longer follow-up is needed to complete and verify these results."
HER2+ cancers treated with Herceptin have a low recurrence risk after 5 years:
- What Is the Risk of Recurrence in HER2-Positive Breast Cancer? https://www.cancernetwork.com/article/what-risk-recurrence-her2-positive-breast-cancer
"A combined analysis of 2 trials totaling more than 3000 patients found a generally low risk of recurrence (RoR) in years 5 to 10 after HER2-positive breast cancer diagnosis. Hormone receptor (HR)-positive disease was associated with improved recurrence-free survival (RFS)."
OVERALL:
- Factors that predict recurrence later than 5 years after initial treatment in operable breast cancer https://wjso.biomedcentral.com/articles/10.1186/s12957-016-0988-0
 0
0 -
Thanks Beesie.
0 -
Da**. I recently assumed/realized that I would probably die of cancer, but I was hoping to have and raise a child before that happened. It is like a slowly falling guillotine that is coming down faster than I thought. I fought and won the grim reaper the first time, but I know he is stalking me. How did my future get cut so short. The things I wanted to do in life seem out of reach now.
0 -
Herb
Im confused on what you are saying . Are you saying 50%of ER/ PRs positive will have a recurrences in 5 years or 50% of those that do have a recurrence happen in first 5 years . Please explain
0 -
IAmAcat, my coworker Minh was young when she received a diagnosis like yours she was considered stage3C grade 3 hormone positive, I don't know what her her2 status was. Her youngest daughter was 6 months old at the time about 1995. She didn't have any children after her diagnosis like you she did chemo and radiation. She had a bmx with DIEP reconstruction later on. At the time we all thought her situation was beyond desperate but she is with us and still cancer free. She was particularly frightened because all the lymph nodes removed were full of cancer. She had 2 sets of full blown radiation treatments on the lymph nodes apparently both sides. She also was given AI drugs years later she may still be on them not sure.
She helped me come to terms with BC and gave me hope, there is no reason to believe you will not have a full cancer free life. Good luck to you.
0 -
Honey - the charts & data from Beesie are more accurate. See if those make sense.
0 -
HI everyone. Does anyone know how recurrence patterns may be effected for weaker Er cancers. I'm in the UK and have a Er score of 33 to 66 % positive an Allred score 6 and Pr + Allred 4.
I've never been told it's any different and I had all the treatment plus i take anastrozole but it's seems a weaker score to me. It was also very aggressive and didn't seem like a standard Er breast cancer. I've searched and searched and can never find much info on it. I always thought being aggressive if it was going to recur it may be earlier and I'm three years recurrence free this week .Many thanks.
0 -
HoneyBeaw, the idea is that of the ER+ people who do have a recurrence, for half of them it happens beyond five years from first diagnosis. NOT that half of them will recur. That’s too high a number.
0