Will 30% of Early Stage (1-IIIA) go on to metastasize??
Comments
-
Shetland. Was was reading research last week that shows you would fall into high risk category based off I have read thru this whole post and I am wondering if not getting chemo even early stage is a good thing. I opted to get Chemo and I was same as you. My decision was based off of knowing 3 ladies with METs. I just had the BCI test last month which shows I am high risk for late distant reacurance 5 to 10 years.. I have done all the treatments available so next year when I finish my AI drugs I just sit back and hope it worked. https://clincancerres.aacrjournals.org/content/19/15/4196
0 -
Herb, have you discussed that with your MO? You could continue AI beyond five years, I guess it all depends on risk assessment. Current guidelines probably say five years on AI for someone who was stage I and node negative, but as additional data become available I don't see why you couldn't continue AI if that were recommended due to a high risk. Like anything else, that would be a trade-off between potential risk reduction and severity of side effects if you are experiencing any.
I am spared this decision because I had many positive nodes, so ten years of hormonal therapy are a given (assuming no relapse in the meantime.)
0 -
Herb, if your BCI test showed high risk of late recurrence for you, why would you discontinue therapy after five years? Why not stay on an aromatase inhibitor or even tamoxifen? I thought the purpose of the test was to help decide between five and ten years of hormonal therapy.
I’m not sure our diagnoses are so similar. You had grade 3 IDC and I had grade 1 ILC. Also I was premenopausal and I assume you were postmenopausal since your stats show anastrazole without Lupron.
Since I did not do the BCI test we don’t know what risk category it would have assigned to me. Now, it is the case that with the new, refined information we have about Oncotype scores, as a premenopausal woman with a score of 16, I would now fall into the category of consider chemo or at least more aggressive hormonal therapy with ovarian suppression and an aromatase inhibitor. I knew back then my being premenopausal had to be important. Furthermore, I had doubts about Oncotype’s accuracy for ILC, and about tamoxifen’s effectiveness for ILC. I wish I had followed my own intuition about that and not the cookie-cutter recommendation of all three medical oncologists I consulted.
Good luck to you, herb. Be well!
0 -
I agree, I would ask your MO. The link is from 2013, something may have changed since then. The 10 yrs has also changed. In 2017 it was recently thought that 7 yrs. hormone therapy is just as good as 10. I don't know where that stands now.
Beesie, you are a godsend to this site! I read on one of my test results that my lifetime risk was greater than 25%. I thought, where did that come from? You just explained it above. Thanks again for your wealth of information.
0 -
Number of years on AI is not a one-size-fits-all protocol. I read the synopsis of the studies that showed 7 years on AI is the same as 10 but those are just statistical averages. I just saw my MO two weeks ago and in my case, she recommends at least 10 years of hormonal therapy (will decide whether to switch me to tamox down the road and depending on bone density). In fact, she left the door open for more than 10 years if everything else is stable.
0 -
Beesie, I'm not gifted to calculate my risk of distance mets. Can you help? Tia!
0 -
I have never been able to correctly interpret a graph, but in my opinion that is not the best format to reflect the risks of recurrence of bc. If the greatest risk of recurrence for ep + is during the first 5 years, the blue line should reach its maximum point at 60 months, then be flat until 120 months and begin to lower. I think that graph suggests that the risk of recurrence is increasing and reaches its peak at 20 years
0 -
The reason BCI test shows to stop after 5 years is based off the DNA of the tumor and how well it response to hormone therapy and they combine that with the risk of Osteoporosis, which is the highest risk factor side effect for taking AI drugs. So now that I have looked over my report, even though I have a higher score 7.8 on BCI. on my dexa scan I lost 8%bone loss after Chemo and next 2 years I lost another 6% and was put on Prolia so my risk factor for osteo (which also kills) is higher than my risk factor for a recurrence from BC cancer.
0 -
since this was bumped up just after metastatic breast cancer awareness day, I will share some current research.
The first one I have is from the Netherlands. 20% of treated patients (someone above said the stats referred to untreated - this is not so!) had recurrence and of that 20%, 72% had distant metastases (as opposed to local or regional recurrence) over 10 yr follow up.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC56020...
One of the problems we have is that the USA is not counting recurrences properly (stage 4 are only the de novo and anyone who recurs technically stays at whatever they were staged when diagnosed) So we need to do retrospective studies to see how many go on to metastasize.
I am at my cancer center in between appointments atm but will try to come back with more studies/resources. Definitely the risk is not insignificant and IMO not talked about enough.
I also think many pts get confused by what their Oncotype results mean...
0 -
Thanks, moth. You are a font of important information.
0 -
The 30% figure has been around for decades. As part of another discussion here recently, I found a couple of studies that suggest that the percent of early stage patients who go on to metastasize has come down significantly. I'll copy and paste some of that information here.
"The observed fifty percent relative decline in distant breast cancer recurrence over time may be related to both improved treatment for initial disease at diagnosis decreasing recurrence risk (hormonal therapy, polychemotherapy, dose-dense chemotherapy, taxanes, and trastuzumab) and stage shift to more early and less late stage disease at diagnosis with improved screening technology and screening program participation. Distant recurrent disease incidence decline over time differed by phenotypic characteristics. We observed a 70% decline in distant disease recurrence among hormone receptor-positive patients and a 50% decline among hormone receptor-negative patients over time. We observed a 60% decline in distant disease recurrence among HER2 positive patients from 1999 to 2006. The differential decline associated with phenotypic subtype creates a new profile of recurrent metastatic breast cancer with fewer HR and HER2-positive cases and relatively more TNBC cases. Ten-year cumulative incidence comparisons to accommodate the longer interval to distant recurrence among HR-positive versus HR-negative disease did not significantly differ from 5-year rates." Source: Examination of a paradox: recurrent metastatic breast cancer incidence decline without improved distant disease survival: 1990–2011 https://link.springer.com/article/10.1007/s10549-018-05090-y
From Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990–2010, here's a graph showing, over 3 time periods, the percent who have developed recurrent MBC, by stage at time of initial diagnosis: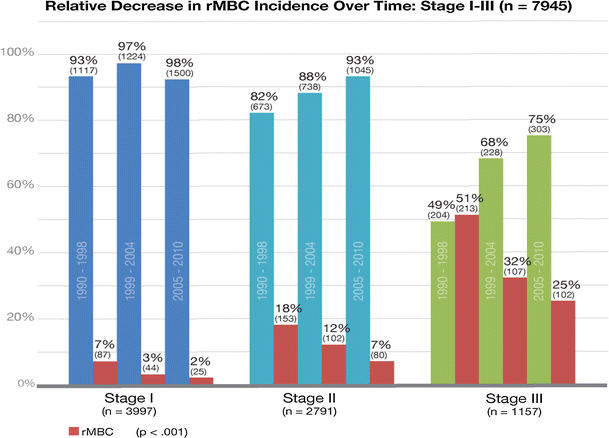
And moth, to your comment, this article presents an attempt to determine the number of people living with mets in the U.S., Estimation of the Number of Women Living with Metastatic Breast Cancer in the United States:
"This study demonstrates that there are a large number of women in the United States living with MBC and that this number has increased in more recent years, likely the result of treatment and aging of the U.S. population. This study demonstrates a growing burden of MBC in the United States. It also makes clear that the majority of patients with MBC, the three out of four who are diagnosed with nonmetastatic cancer but progress to distant disease, has never been properly documented. Given the growing burden of MBC, it is critical to collect data on recurrence to foster more research into the specific needs of this understudied population."
 0
0 -
the thing that stands out for me from the examination of a paradox article "Out of 8292 invasive breast cancer cases stage I–III at initial diagnosis from 1990 to 2011, 964 cases (11.6%) had distant metastatic recurrence (rMBC)."
That's quite a bit smaller than what the Dutch study found
0 -
Beesie and Moth, I follow this thread. Its where my fear lingers. Beesie, I have to admit that when I see the graphs and quotes I hear this humming white noise, much like the blank panic I experienced in grade 5 when asked to do long division at the blackboard. I need it interpreted for those of us intellectually challenged who could look at a graph all day and not gain one iota of information from it (me).
Moth, what were you meaning when you said many people don't understand their Oncotype scores?0 -
runor, the italicized paragraph in my previous post provides a summary interpretation.
0 -
Beesie, I appreciate you sharing the article and analysis. Being a fan of graphs (sorry, runor!) I read the entire article and examined the graphs. One thing that jumped at me was the length of follow up. The study is based on follow up results through 2016. They talk about the 2005-2011 cohort having the lowest rMBC incidence, yet this is the only cohort that had patients with less than 10 year follow up. As we know (and article states), HR+ time to distant recurrence can be a lot longer than 5 or even 10 years, so I'm not sure if this is accounted for anywhere in the study. In other words, some of the patients diagnosed in 2005-2011 may still develop metastatic disease, while patient from other cohorts are a lot less likely to develop any after >20 years since their DX. Am I missing something?
0 -
FarAwayToo, interesting that you mention that. It's the same thought I had when I read the study.
The shorter follow-up for the most recent cohort is mentioned only once:
"Colleoni et al found a lower annualized hazard of recurrence among ER-positive versus ER-negative breast cancer in the first 5 years post-diagnosis which reversed at 10 years post-diagnosis [29]. With less follow-up, our last cohort (2005–2011) findings may be skewed towards more triple-negative and less HR+ distant recurrence due to differential time to distant relapse associated with hormone receptor status. For this reason, we ran additional analysis using only the first two cohorts and Kaplan–Meier plots with at least 10-year follow-up and found no difference in proportional change over time."
From reading the report, it appears that modelling was used in the calculation of the results. And of course, a portion of the most recent cohort did have 10 year follow-up. Still, I would agree that the results for the 2005-2011 patients might be under-estimated. But if you just compare the 1990-1998 cohort with the 1999-2004 cohort, the 5 and 10 year results show significant declines in the percent of patients who develop mets. So whether the decline is 30% or 50% may be in question, but in either case it's good news.
0 -
While I'm glad to see there are apparent declines in recurrence (esp in some subtypes of breast ca) I do wish that they would list the actual rates rather than just listing relative declines. But also, a 30% relative decline would knock the recurrence down from the high of 30% that was batted about, down to 20%. And it's possible that the 30 was high to start with?
One problem with us not counting cases well is that the studies - even ones published very recently - are often looking at datasets which closed 5-10+ years ago but that's what we have.
As an aside, I've read the Estimation of the Number of Women Living with Metastatic Breast Cancer in the United States several times now because I feel like the data point we're looking for *should* be in there somewhere. They know how many women get dx with breast ca, they know how many are de novo and how many are recurrent, so they should be able to say what percentage of early stage dx get recurrence. But I read over and over and didn't find it. I almost want to email an author and see if they know the number...0 -
YES, email the author!! I've done this a couple of times and gotten very quick responses. People are excited to share what they're working on and they WANT people to understand it. Please do, and let us know!
 0
0 -
I did email the prinicipal author. Will let you know if I hear back. She works for NIH. Who knows, maybe it will land on her desk when she's procrastinating and glad to do something else for a bit :P
0 -
I am not great with all of the statistics but often wondered if the 30% was high. The latest figure I have seen is a survival of 80% for 15 years. If stage 4 de novo is 6 to 10 % and some of those are in the 80% that would definitely mean less than 20 % of the others have recurred. Am I missing something here? Thank you
0 -
This thread was started 7 years ago. The 30% figure may have been an accurate long-term stat at that time, but even then it would have been important to note that long-term mortality and survival stats by necessity are based on people who were diagnosed a long time ago. So at best this stat was only minimally relevant to someone diagnosed in 2013. And now, 7 years later....
I wish this thread would be allowed to fade into oblivion. The topic and discussion is relevant, but the subject line of this thread unnecessarily scares so many people, and too many people believe this stat just because they read the subject line. Not many people bother to read all the comments, many of which question or contradict this stat, as my previous recents posts did, and as this post will.
If you look at the most latest SEER data in the chart below, the most current 25-year survival rate stat available is based on people who were diagnosed during the period of 1985-1989. Treatments today are completely different. Even the most recent 15-year survival data is based on people diagnosed and treated in 2002, 18 years ago. So the long-term survival figures from this chart need to be considered in the context of the years when these individuals were diagnosed, and the treatments available at that time.
What is significant and meaningful from this chart are the long-term trends. Take the 15-year survival stats, for example: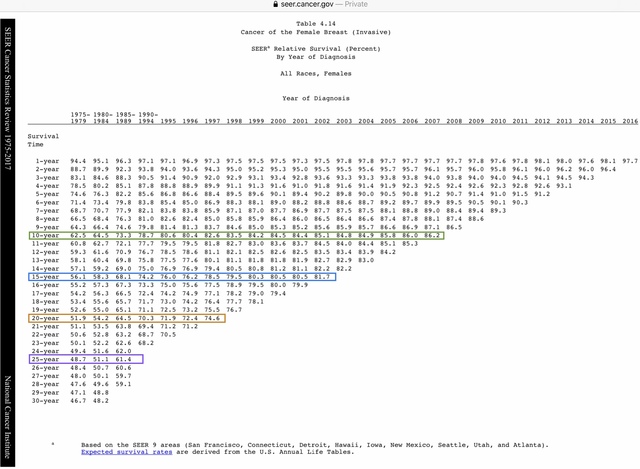
- For those diagnosed between 1975-1979, the 15-year survival rate was 56.1%.
- For those diagnosed 10 years later, between the years 1985-1989, the 15-year survival rate was 68.1%.
- Another 10+ years later, for those diagnosed in 1999, the 15-year survival rate was 80.3%.
- And for those diagnosed in 2002, the most recent year for which 15-year survival data is available, the rate is 81.7%.
Over this 23 year period, 15-year survival has improved from 56.1% to 81.7% - this is very significant. For the 20 and 25 year survival stats, while the 'most recent' data available is not very current, we do see similar significant improvements when compared to the 1975-1979 period.
Judy, Stage IV de novo is consistently 5%-6% of those diagnosed in any given year. And while I've used the example of 15-year survival stats in this discussion, I wouldn't consider 15-year survival to be an equivalency for what percent of early stagers develop mets. Many patients who develop mets, particularly those who have ER+/HER2- cancers, may not be diagnosed for 10, 15 or even 20 years, and might then survive for an extended number of years. 25 or 30 year survival stats probably better reflect what percent of early stagers develop mets, but these stats are just not relevant to someone diagnosed today, with such different treatment protocols.0 -
Beesie, thanks as always for digging out and presenting the stats in a way that (I consider) is easy to understand. Most people don't have any training at all in statistics or in reading academic research of any subject. It's pretty confusing in general, and even more in trying to figure out how those stats apply to the individual. And even if you can get that far, it's hard to know what to do with that information. That's a big part of where the fear or anxiety comes in, at least for me. Anyway, thanks.
0 -
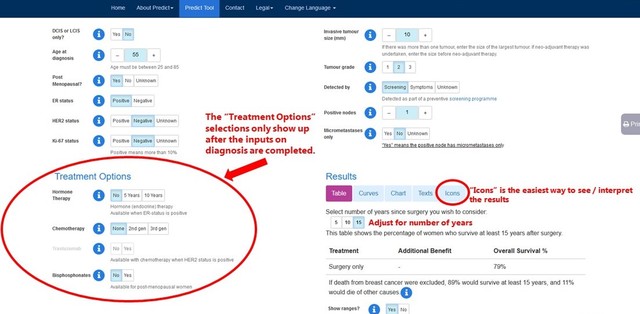
For the individual, IMO Predict is a good tool (in addition to discussing with the MO, of course). https://breast.predict.nhs.uk/tool
I was technically a 'caught early, stage 1 blah blah' but 22% of women with my stats & treatment are dead 15 yrs later. Not as bad as 1/3 but again otoh, I was supposed to be a "we got it early" success.
Ultimately, it's binary. You recur or you don't. You're metastatic or you're not. You can try to put your thumb on the scale by doing all the treatments, exercising, not drinking, not smoking, maintaining good BMI etc etc etc but if dna wants to misbehave, our bodies can't always control it.I think it lingers in our minds forever. I don't think it's about freaking people out so much as being clear that there is no guarantee, there is no cure, anyone can recur, or have a new primary that is metastatic & having had cancer once itself raises risk 3-4 fold so there is always going to be the lurking worry.
0 -
Thank you Bessie for your reply. Very Interesting information. Judy
0 -
Beesie,
Thank you so much for being willing to share your knowledge with people on this site. I was just thinking today how grateful I am that you have chosen to read and learn and help those of us who are interested in the science and statistics. I am grateful.
For me, it is important to understand my risk of recurrence, because even though “only" DCIS, I did have close margins and additional surgery, and because ER-/PR-, it would be harder to treat a recurrence. And of course as Moth points out, the greater risk for those of us who have had breast cancer is always there. I want to understand as much as I can, and not be blindsided if it comes back. Then I want to put that info and fear into a box and only let it out occasionally. (Sometimes that works, and then I have a twinge in my foob or under my arm and all rational thought leaves my brain).Still, of all the things that worried me and I thought might happen to me, breast cancer just wasn't it. So, if I can't control if it comes back (not really), I will learn as much as I canand try not to be shocked.
0 -
"I think it lingers in our minds forever. I don't think it's about freaking people out so much as being clear that there is no guarantee, there is no cure, anyone can recur, or have a new primary that is metastatic & having had cancer once itself raises risk 3-4 fold so there is always going to be the lurking worry."
moth, I agree. I hate it when I see people come back here, shocked that they have been diagnosed with a local recurrence or with mets, or with a new primary. It's one thing to be angry or upset, but nobody should be shocked. Everyone should understand their risk and know that no matter their diagnosis, no matter how low their risk, and no matter what they do, a local recurrence or a metastatic recurrence or a new primary is possible.
That said, there is a difference between having a 5% risk and a 35% risk. And everyone should understand that too, and understand where they fall and why.
The discussion about future risk is important, and one that I engage in often on this board. What I dislike is the title of this thread, which is 2020 is misleading and simply no longer true. And it's just so broad. All "early stagers"? Stage IA and Stage IIIA do not confer the same risk. All other things being equal, ER+/PR+ and triple negative do not confer the same risk. Risk is so complicated; how can a single statistic be in any way meaningful for 80%+ of all breast cancer patients? Yet I see the 30% stat parroted back by women on this board who have small, favourable, early stage cancers and likely have a risk more in line with 5%-10%. I have seen too many women terrified by this stat that doesn't apply to them.
This is a 7 year old thread with an outdated title. I cringe whenever I see it pop to the top of the active list, sometimes after months of inactivity. I wish this thread could be retired. But I'm all for continuing and participating in any discussion about future risk.
0 -
Oh my god! I'm reading along and realize there are two posts here by two long-time posters that so perfectly sum up the picture. There is Beesie, calmly, steadily, with facts and rationality talking us out of the tree. And Moth sums up perfectly why we're up the damn tree in the first place!
Beesie, I get why you wish this thread would fade, It does have an inflammatory, misleading title that jolts and jars and makes people climb trees in panic and despair. Sussing out the truth requires thinking, rational examination of all the stats and numbers and being able to figure out how they apply to us and what we're going to do about it : come out of the tree or wait for a hunky fireman with a ladder. With my luck they'd decide rescue was too risky and shoot me with rubber bullets until I fell out.
I follow this thread because while I have gotten on with life more and more all the time it is never, NEVER out of my mind. That blissful bubble of eternal life was popped and their ain't no going back.
0 -
Perhaps the Mods could revise to the title somewhat? Instead of will 30%, What % of early stagers will go on to metastasize?
I don't know if that type of modification is allowed, if the original creator of the thread would be willing to have that revision made.
Thanks, Beesie for your wonderful absorbable information. It is so very helpful and so appreciated.
0 -
Beesie - Thanks so much for sharing your knowledge with the rest of us. I'm still a newbie currently going through chemo. I like to educate myself as much as possible, but find I get discouraged/confused by so much misleading and outdated information out there. I'm throwing everything I can at this beast with the hopes of no recurrence, but I'm also not naive to think it can't happen. I already find myself worried about every new ache and pain, and I'm sure that will continue. The title of this thread is what made me click on it to find out more information so I'm thankful for that. I agree there are many who probably read the title without reading the comments so may not helpful for them.
Moth - I tried the IMO Predict tool but it only gave me %s with surgery only. I assume (hope!) these increase the odds of survival.
I had a low oncotype score of 9. However, my breast surgeon ran it on my tumor biopsy and not post surgery. Before my surgery, my tumor size was estimated at 2 cm with no lymph node involvement. My tumor ended up 4.5 cm with 3 lymph nodes affected. So not sure how much to trust that score. I wasn't educated enough at that time to challenge the timing of the Onco test. My MO office then got me in a Mammaprint study. On that, I'm considered "Low" risk but it's at the upper end of Low, not too far from High, so of course I worry.
Thanks ladies!
0 -
brittonkb, you should be able to input your treatment into the PREDICT model once you complete the section on your diagnosis. The treatment options don't show up on the page until that top diagnosis section is filled out.
Since the Oncotype score is based on a test of the genetics of your cancer - the test looks at 21 genes within the cancer cells - I wouldn't think that the result would be different with a biopsy sample vs. a a surgery sample. What would be different is the scale on which the recurrence risk is assessed, since there is a different scale for node negative vs. node positive. So if your score and recurrence risk were provided based on the assumption that you'd be node negative, while the Oncotype 9 score likely wouldn't change, your recurrence risk might be a bit different based on being node positive. I don't know however how different the node negative vs. node positive scales are for scores in the low range.
 0
0