VITAMIN K2 combined with Vitamin D3 IMPROVES bone density
Comments
-
bump
0 -
Since my cancer diagnosis, I have upped my supplements by consulting with a Pharmacist I trust, i.e., Vitamin D3, calcium, magnesium, multi, probiotics and taking the highest amount available. Because I had an episode last year with iron deficient anemia, my doctor has triple my iron supplement. My oxygen, iron, kidney function, liver function have good values. I have switched to an alkaline diet - no carbs, no sugars, healthy fruits and vegetables, etc. Walking as much as possible, and have lost five pounds. Using essential oils on my feet. So far it's making feel better and more positive about handling this diagnosis.
0 -
That's great for taking control of diet and supplements, 53Nancy!
If you are taking calcium, it is good you are taking D3, but also ESSENTIAL you take K2. It will help the calcium deposit in your bones rather than your arteries.
0 -
That's so true, Vitamin K2 is essental for making sure the Calcium winds up in your bones, not your blood vessels. Calcium supplementation without Vitamin K2 causes increased risks of Coronary Artery Disease, the number #1 killer of women.
Science News
from research organizations
Benefits of calcium supplements may be outweighed by cardiovascular risks
- Date:
- May 12, 2016
- Source:
- The Norwegian University of Science and Technology (NTNU)
- Summary:
- Taking calcium and vitamin D can help prevent broken bones in older women. However, this benefit may be cancelled out by an increased risk of heart attack and stroke, say researchers.
- Share:
FULL STORY
Taking calcium and vitamin D can help prevent broken bones in older women. However, this benefit may be cancelled out by an increased risk of heart attack and stroke.
With the highest reported risk of hip fractures in the word, Norway has good reason to consider the benefits and risks of calcium supplements. The challenge is that too little calcium and vitamin D in your diet leads to an increased risk of osteoporosis and broken bones, which taking supplements has been shown to help prevent.
However, some studies have also shown that taking supplemental calcium may also increase your risk of heart attack and stroke.
"We conclude that the moderate effect of supplemental calcium and vitamin D on the risk of fractures is not large enough to outweigh the potential increased risk of cardiovascular disease, specifically in women who are at a low risk of bone fracture," said Gunhild Hagen, a PhD candidate at the Norwegian University of Science and Technology's (NTNU) Department of Public Heath and General Practice who was first author of an article recently published in Osteoporosis International.
Analytical model of health effects
Researchers at NTNU and the University of Oslo used an advanced analytical model to investigate the total health effect of taking a combined calcium and vitamin D supplement, compared to taking no supplements, based on a group of healthy women aged 65 with a BMI of 24 kg/m2.
"Our analysis shows that if 100,000 65-year-old women take 1000 mg calcium every day, 5890 hip fractures and 3820 other fractures would be prevented. On the other hand, as many as 5917 heart attacks and 4373 strokes could be caused. So for women of this age, the risks outweigh the benefits," the authors of the study wrote in an article in Aftenposten, one of Norway's national newspapers.
0 -
I find this thread really helpful. I had a recent bone density test and my oncologist is now concerned that I've rapidly developed osteoporosis. I eat plenty of beans and veggies but not dairy. I walk a lot on the job and exercise often. I'm already on Vit D3 (2000) but not on Vit K2. I take Calcium/Mag/Zinc supplements but was very wary about taking a full dose so because I read somewhere that calcium supplementation is modestly effective. Now I'm second guessing myself my onco reiterated that I take 1200 mg Calcium. He also wants me to start Zometa infusions! I still have 2.5 years to go for Letrozole and I'm postmenopausal so my osteoporosis is most likely to get worse. But upon reading this thread, I'm glad to see that some of you have been able to find a "fix".
0 -
Well dang. My pcp just told me stop the vit K2. I take Tamoxifen that can cause blood clots, and so can vit K2. I have osteopenia and she's going to speak with my MO about putting me on a med for it, forgot the name.
0 -
Hi Michelle, sorry to hear your bones are having issues, but that is par for the course with all AI's. Definitely look into having an increased amount of Vitamin K2, either through food or by supplements, to balance out your Vitamin D3. Why such low Vitamin D3 doses? What is your Vitamin D3 blood levels? It is recommended to have a range of 40 to 80ng/mL, depending on the study quoted. I don't think that 2,000IU of Vitamin D3 will give you sufficient blood levels. My oncologist tested me and said I should be on 5,000IU per day.
D
Endocrine Society Says Vitamin D Deficiency May Be Common in U.S.
June 6, 2011 -- Noting that vitamin D deficiency is "very common in all age groups," new treatment guidelines call for many Americans to take more vitamin D than is currently recommended.
The guidelines, from the Endocrine Society, offer some contradictory advice. They say that virtually everyone in the U.S. should be taking vitamin D supplements, but that only those at risk for vitamin D deficiencyshould have their vitamin D blood levels checked.
Only those whose serum 25(OH)D blood levels are above 30 ng/mL are getting enough vitamin D. Lower levels are "insufficient," and those with levels below 20 ng/mL are frankly deficient.
But much higher levels are better, says guideline committee chairman Michael F. Holick, MD, PhD, director of the vitamin D skin and bone research lab at Boston University.
"The committee decided that 30 ng/mL is the minimum level, and recommended 40 to 60 ng/mL for both children and adults," Holick said at an online news conference
0 -
Yes I had my Vit D level tested but I don't remember the exact numbers. I will call and find out. Looking closely, besides the 2000 iu pill, there's 1000 iu in the multivitamin I take. I'm going to make an appointment with a naturopath so I can get a better clue on the optimal doses I can take considering my background. Since I'm already on supplements, does it make sense to get blood tests done related to bone health and density? What tests do you think are helpful?
My multivitamin has 80 mcg of Vit K but it doesn't specify what kind. I've been vegan since my initial diagnosis so it's a challenge to get the Vit K2 from food. I do eat lots of beans, spinach, other greens. I decided today I'm going to start eating an egg a day. I do eat salmon occasionally; add more sardines/herring.
0 -
Well, there aren't really blood tests that test bone health, other than Vitamin D (25 OH-D) and Undercarboxylated Osteocalcin (ucOC) which is a test that correlates with Vitamin K2 intake. Your Naturopath can help get you those tests, or try Genova, which is on the link. A good, somewhat odd Vegetarian sourced Vitamin K2 rich food is the Japanese Fermented Soybean food called Natto.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC288157/
GENOVA Diagnostics is a lab that does these tests, not always common in mainstream labs like Quest or LabCorp, although there could be other labs that do this test also.
https://www.gdx.net/product/vitamin-k-test-serum
Serum undercarboxylated osteocalcin is a marker of the risk of hip fracture in elderly women.
P Szulc, M C Chapuy, P J Meunier, and P D DelmasAuthor information ► Copyright and License information ►See commentary "Vitamin K nutrition and postmenopausal osteoporosis." on page 1268.
This article has been cited by other articles in PMC.
Abstract
It has been previously shown that the level of circulating undercarboxylated osteocalcin (ucOC) is elevated in elderly women in comparison with young, healthy, premenopausal ones. To understand the mechanism of the increase in the ucOC in the elderly and to assess its potential consequences on bone fragility, we have measured ucOC in the sera of 195 elderly institutionalized women 70-101 yr of age. In 45 women (23%) serum ucOC was above the upper limit of the normal range for young women. The level of ucOC was negatively correlated with 25OHD (r = -0.32, P < 0.001) even after excluding the effect of age, parathyroid hormone (PTH), and creatinine by partial correlation (r = -0.24, P < 0.002). During an 18-mo follow-up, 15 women sustained a hip fracture and their baseline ucOC level was higher (P < 0.01) in women who subsequently sustained hip fracture than in the nonfracture group contrasting with no significant differences for serum calcium, phosphate, alkaline phosphatase, creatinine, PTH, 250HD, and total and carboxylated OC. The risk of hip fracture was increased in women with elevated ucOC (relative ratio 5.9, 99.9% Cl 1.5-22.7, P < 0.001). During 1 yr of calcium/vitamin D2 treatment, ucOC decreased (P < 0.05), especially in those with the initially increased values (from 2.22 +/- 0.35 to 1.41 +/- 0.29 ng/ml, P <0.005) contrasting with an increase in the placebo group (P < 0.05). In conclusion, the increase in ucOC in the elderly reflects not only some degree of vitamin K deficiency but also their poor vitamin D status, suggesting that vitamin D may be important, either directly or indirectly through its effect on bone turnover, for achieving a normal gamma-carboxylation of OC. The ucOC, but not conventional calcium metabolism parameters, predicts the subsequent risk of hip fracture, suggesting that serum ucOC reflects some changes in bone matrix associated with increased fragility.
0 -
Bump
0 -
My Vit D 25-OH level is currently 52.8 ng/ml (reference rate 30-60 ng/ml) so that's good news. I started Vit K2 500 mcg (MK-4 400, MK-7 100 mcg) . I finally got to see a naturopath and she says the Vit K dose is adequate. I joined a gym and started on resistive exercises based on a study about exercise effects on osteoporosis and even got a weighted vest (10 lbs) to wear around the house and when on elliptical machine. She did emphasize taking calcium supplements in small doses spread throughout as >500 mg taken at one time increases calcium too much at a time and that's when it gets deposited in other places of the body other than the bone. She also added strontium citrate.
I also read a study on eating lots of dried prunes which increased bone density. I figured that based on my background I have increased risk of developing osteoporosis anyway. My body build is small especially in the upper half so I think my bones have not been getting much weight bearing through the years. I also didn't grow up drinking dairy and eating cheese and meat. I tan easily and since living in the northwest in the past 19 years did not help with Vit D levels.
0 -
That sounds really good Michelle. I forget occasionally, but am taking Vitamin D3 10,000IU every other day. Last year when I checked my level of Vitamin D it was only 36, and my Naturopath wants my levels up to 70ng/m, because of the bc history. I also am taking the Vitamin K2 every day, although I forget the dose at the minute. I also get weight bearing exercise 5 to 6 days per week walking my dog up and down the hills in the wooded trails near my house.
Where in Washington do you live? I live in Seattle.
0 -
I live at the north end of Tacoma! Great to know you're close. It's been a blessing in disguise that now I really have to exercise. I hate it but I literally feel benefits immediately. I have less joint pains and have more energy. I dread the winter coming up. It's going to get harder to step out of the house.
0 -
Michelle49
May I ask you which brands of calcium, K2, and strontium citrate you use? Thanks for the tip about taking calcium supplements in smaller amounts throughout the day for better distribution of calcium to bones. I have bought some Vitamin K off the shelf at a drug store, along with off-the-shelf calcium citrate supplements with D3 and just started using them, so not sure they are doing the job. Next bone mineral density is in August (I had one in August and was borderline osteoporotic). I do have a Vit D 25-OH coming up this month. I am also on Prolia x2 per annum.
Thanks,
0 -
SajeScents,
I take the Calcium/Magnesium/Zinc by Solaray, Vegan K2 500mcg by Country Life which I got from Marlene's a local natural health food store and the Strontium Pure Encapsulations which I got from naturopath's office. I'm planning on shopping online for the latter two for better pricing. She said to skip a calcium dose and substitute strontium because they compete for absorption. I asked her if she's seen cases when the osteoporosis was reversed. She said yes up to 10-12% reduction, more so with osteopenia. I wanted a BMD done after six months but she said it's too soon; a year is adequate.
Exercise study:
https://universityhealthnews.com/daily/bones-joint...
Prune studies
https://www.cambridge.org/core/journals/british-jo...
https://www.ncbi.nlm.nih.gov/pubmed/26902092
0 -
Thank you, Michelle. That's very helpful!
0 -
I am crazy confused right now. I was just reading in another cancer forum (Canadian) that cancer likes calcium to grow, and consequently we should avoid ingesting too much calcium. However, I have osteopenia already, am on AI daily, had one injection of Prolia (rx'd twice per year) and was advised by my MO to take Vit D3 and increase my intake of calcium and calcium-rich foods. It looks like a no-win situation if it is true that calcium grows cancer, or is that just a myth? I am taking Vitamin K2 supposedly to help distribute the calcium to bone and not to soft tissue. I also like Gouda and Brie cheese for the same reason.
What's the real truth on calcium ingestion and cancer growth??? Thanks in advance.
0 -
From Wikipedia
CalciumEdit
Some studies have found a relationship between calcium intake and lowered breast cancer risk.
- In the Nurse's Health Study, a high dietary intake of calcium showed 33% lower risk of breast cancer.[23]
- Cancer Prevention Study II Nutrition Cohort Concluded 20% lower risk of breast cancer with 1250 mg of calcium intake.[24]
- Women's Health Study shows an inverse association between total calcium intake and premenopausal breast cancer risk.[25]
- Another two studies, one in France[26] and another in Finland,[27] showed significant inverse relation between calcium intake and breast cancer.
- Hypotheses
- Calcium reduces cell proliferation and induces differentiation in mammary glands.
- High calcium intake decreases fat-induced epithelial hypoproliferation of mammary gland and chemically induced carcinogenesis.
- Breast density is positively associated with breast cancer. Dietary calcium intake reduces the breast density.
- High calcium intake is associated with a reduced risk of benign proliferative epithelial disorders which are thought to be precursors of breast cancer.
Vitamin DEdit
Main article: Vitamin D § Role in cancer prevention and recovery
Vitamin D is related to reduced risk of breast cancer and disease prognosis. A 2011 study done at the University of Rochester Medical Center found that low vitamin D levels among women with breast cancer correlate with more aggressive tumors and poorer prognosis. The study associated sub-optimal vitamin D levels with poor scores on every major biological marker that helps physicians predict a patient's breast cancer outcome. The lead researcher stated, "Based on these results, doctors should strongly consider monitoring vitamin D levels among breast cancer patients and correcting them as needed."[28]
- Hypotheses
- Vitamin D metabolites (25 (OH) D, 1, 25 (OH) 2 D) promote cellular differentiation and it is important for chemoprevention.
- Low circulating levels of 25 (OH) D in adolescence may be an important predisposing factor for breast cancer risk in later life.
0 -
Wow! Marijen, thank you very much for taking the time and sharing your research! This helps a lot!
0 -
I don't worry too much about my Calcium intake. I have yogurt several times per week, and a little bit of milk every day in my tea. I never take Calcium Supplements, since it is shown to increase risks of Coronary Artery Disease. When you look at the low incidence of Osteoporosis in Japan, and the fact they have a very low amount of Calcium in their diet, Calcium, by itself, is not as crucial to bone health as it used to be assumed. Vitamin K2 is important for bone health, and without sufficient K2, it is harder for the Calcium to get into the bones.
Lower calcium intake in Japan, with 400-500 mg/day mainly as soybean products, small fish with bones, and vegetables.
- Osteoporosis in Japan: factors contributing to the low incidence of hip fracture.
Fujita T1.
Author information
Abstract
Hip fracture incidence seems to be lower in Japan than in many Western countries, but the difference is apparently becoming smaller with progressive Westernization of the Japanese lifestyle and nutritional habits. Nutrition cannot explain the lower incidence of hip fracture. A lower calcium intake prevails in Japan. Genetic differences in body build, including a lower center of gravity, better motor function and agility, well developed hip musculature and small but more fracture-resistant bones secondary to a difference in life- and work-style may contribute to fewer falls and a lower fracture rate among Japanese than among their Western counterparts. Such traditional lifestyle habits as sitting directly on the floor are rapidly decreasing, and time will tell how much of the low incidence of hip fracture in Japan can be explained by lifestyle and how much by genetic and other factors. The Japanese women who now enjoy a low hip fracture incidence led a hard physical life when they were young. This may be a lesson to the young of future generations in how to avoid bone fractures when they are old. Bone health may be achieved by enjoying life through sports or even the tea ceremony in place of the hard physical work of their ancestors, which is gradually disappearing.
0 -
I'm very grateful that I've found this thread! I've been reading a book Vitamin K2 by Dr. D. Goodman. He does a great job of explaining the processes involved as well as showing the decades of research supporting it. Basically Vit K2 is needed to activate the proteins responsible for inhibiting calcium mineralization in the arteries (the matrix G1a) and for binding calcium to the bone matrix (osteocalcin). The activation of these proteins ensures calcium goes to the bone and not the blood vessels and other soft tissues.
Then I read a couple of books on magnesium supplementation by Dr C. Dean. I understand now how important it is, as much as calcium, Vit K2, and Vit D3 for bone health. There's just too much good information to include here but she's basically saying that 1:1 ratio calcium/magnesium is ideal. Also not to take more than 2000iu of Vit D3. Magnesium converts Vit D supplements or its storage form into its active form which is then absorbed in the gut. Too much Vit D in storage form (and calcium) depletes the magnesium that is needed for its many other roles in the body. I'm finding out that I may have some symptoms of magnesium deficiency.
The next book I want to read is the calcium paradox. As for the supplement brands and dosages I'm taking, I've changed it a bit. I'm looking closer at the multi vitamin I'm taking and of course it doesn't have calcium, magnesium, zinc and Vit K2. Since the ratio that I'm following has changed I can't use the same Solaray Ca Mag Zinc I've been taking, I've switch to magnesium citrate for better absorption up to 500mg/day. I'm going to try the Remag also. I've switch to a separate Calcium citrate supplement for better absorption and I'm not taking 1200 mg like the MO recommends (!), more like 500-700mg/day in the 1:1 ratio. Still on K2 750mg. And I have to add zinc.
This goes without saying that I'm eating lots of nuts and seeds, added eggs to my diet, going to the gym for resistive exercises, and weight bearing exercises. What a difference a month makes. When I left the MO office after he told me about the bone density test and reiterated that I increase my calcium supplementation, I did not feel good about a lot of things. I felt that I needed to advocate for myself instead.
0 -
Hi Michelle49, glad you came over to share what you have been doing.
I am too worried about Heart Disease to do Calcium in supplements. There were those 2 studies, saying supplements of calcium increase risks heart disease, but not calcium from food. I only get my calcium from my diet.
Science News
from research organizations
Calcium supplements may damage the heart
- Date:
- October 11, 2016
- Source:
- Johns Hopkins Medicine
- Summary:
- Taking calcium in the form of supplements may raise the risk of plaque buildup in arteries and heart damage, although a diet high in calcium-rich foods appears be protective, say researchers at conclusion of their study that analyzed 10 years of medical tests on more than 2,700 people.
Calcium Intake From Diet and Supplements and the Risk of Coronary Artery Calcification and its Progression Among Older Adults: 10‐Year Follow‐up of the Multi‐Ethnic Study of Atherosclerosis (MESA)
0 -
Michelle - is it really 750 milligrams of K2? I take 100 micrograms (0.1 mg)
0 -
I was going to ask the same question! Mine is 100mcg mk-7 and 500 mcg mk-4
0 -
It's mcg, sorry. I can't keep it straight
0 -
There is no harm in using much, much, much higher doses of Vitamin K2. I take Osteo K Minis, which is the Japanese dose of 45 milligrams per day of Vitamin K2. This dosing is a thousand times higher, with no side effects ever noted. I know people don't always like nonmainstream journal articles, but here is the information summarized from all the research. Obviously, if you are on Anticlotting medications, talk to your provider about any K2 supplementation.

Protecting Bone and Arterial Health with Vitamin K2
March 2008
By William Davis, MD

Millions of people take calcium supplements to maintain healthy bone. Yet few patients or physicians realize that optimizing bone integrity involves more than taking a single mineral supplement. A critical additional component for bone and cardiovascular health is vitamin K2.
Recent research has revealed that, without vitamin K2, calcium regulation is disrupted. In fact, low levels of vitamin K2 are associated with an increased risk of heart disease and atherosclerosis.1 Astute doctors have long known that people with a lack of calcium in their bones are more likely to possess an excess of calcium in their arteries, and vice versa. The resulting lack of calcium in bone leads to osteoporosis, while the deposition of calcium in the arterial wall leads to coronary heart disease and other manifestations of cardiovascular, renal, and neurodegenerative disease.
Although vitamin K has been around for decades, dietary recommendations have been overshadowed by the nominal amount required for healthy blood clotting—and have ignored the optimal amounts of vitamin K needed to maintain healthy bones and arteries. In this article, we'll explore how vitamin K2 regulates calcium as well as the recent evidence supporting this unique vitamin in preventing heart disease and osteoporosis as well as certain types of cancer.
Vitamin K2—Essential for Healthy Arteries and Bones
Osteoporosis and heart disease—they seem as unconnected as two conditions can possibly be. On the surface, they do share a few common features. Both conditions develop with age. It's rare for someone to have either condition at age 30, but both are common in the sixth or seventh decade of life. Both conditions don't develop overnight, but require many years to emerge. Just as osteoporosis requires decades to develop, coronary atherosclerosis also accumulates bit by bit over decades, starting in a person's 20s (or earlier) and building gradually until a heart attack or other catastrophe occurs.

But the resemblance appears to stop there—that is, until we dig beneath the surface. As long ago as the 19th century, scientists knew that an unknown material lining diseased arteries resembled a bone-like structure. For the next 100 years, however, this finding was dismissed as a curiosity, an inevitable accompaniment of aging, and evidence of "wear and tear," just like arthritis.
Dr. Linda Demer and her team at the University of California, Los Angeles, were among the first to unravel this curious connection by successfully identifying a protein in human atherosclerotic tissue, which was previously believed to reside only in bone tissue. This protein, called bone morphogenetic protein-2, plays an important role in bone formation.2 Since then, several other key regulators of bone formation have been identified in atherosclerotic plaque tissue, such as matrix GLA-protein and osteopontin, suggesting that common factors might influence both arterial and bone health.3

Another curious observation increased the momentum to find a link between bone and arterial diseases. People who had osteoporosis, or a lack of calcium in their bones, were more likely to possess an excess of calcium (bone) in arteries and vice versa. In fact, what had often been simply assumed to be calcium deposits or calcified plaque was actually fully formed bone tissue. Vascular calcification should therefore be more properly designated as vascular ossification—bone formation within blood vessels. Likewise, many "risk factors" for coronary atherosclerosis were also prevalent in osteoporosis: aging, diabetes, sedentary lifestyle, smoking, and high cholesterol.3 Scientists questioned why there was such a tight link between excess calcium in one organ (bones) and deficient calcium in another (arteries). And why, in some apparently healthy people, are the two present simultaneously to such extremes?
Initially, some proposed that there may be an abnormal transfer of calcium from bones to arteries. This did not hold up to scrutiny, however, since each system proved to be under its own regulation.
Although certain prescription drugs, such as raloxifene (Evista®) and alendronate (Fosamax®), addressed the problem of osteoporosis, no solution emerged to address both bone and arterial health, that is, until now. Current research is highlighting the importance of nutritional solutions to control the link between arterial and bone diseases by addressing calcium metabolism in the body—in particular, the role played by vitamin K2.
VITAMIN K BASICS
In nature, vitamin K is found in two forms: vitamin K1 (phylloquinone) in leafy, green vegetables, and vitamin K2 (menaquinone) in organ meats, egg yolks, and dairy products.
Vitamin K is required by the human liver to manufacture blood-clotting proteins (factors II, VII, IX, X; and proteins S and C). This is the basis for administering the vitamin K-blocking drug, warfarin (Coumadin®) to people who have blood clots or are at risk for blood clot formation, since clot formation is effectively suppressed by the drug.
Determination of the human need for vitamin K was therefore based on the amount necessary to maintain a normal balance between blood clotting and thinning. Blood shouldn't be excessively "thinned" and prone to abnormal bleeding, nor excessively "thick" and prone to clotting in the wrong place.
Beyond its role in blood clotting, recent research has revealed that vitamin K also plays a vital role in maintaining healthy bones and arteries by keeping calcium in the bones and out of the arteries.
Unfortunately, the recommended dietary intake of vitamin K required for blood clot regulation is much lower than that required for optimal bone and arterial health.
Osteoporosis and Vitamin K2 Intervention—the Evidence
Since it was first discovered in 1929, vitamin K has been best been known for its crucial role in the blood-clotting process. Since that time, scientists have uncovered compelling evidence that vitamin K plays an equally important role in bone health.
The majority of vitamin K research to date has focused on vitamin K1, the dominant dietary form of vitamin K that occurs in green, leafy vegetables. Yet it appears that vitamin K2, which occurs in organ meats, egg yolks, and dairy products, is a more important inducer of bone mineralization in human osteoblasts (bone-building cells) than vitamin K1.4

The Japanese long ago recognized the power of vitamin K2 to maintain or restore bone health. In certain regions of Japan, a staple dish called natto or fermented soybean, frequently eaten several times a week, is uniquely rich in vitamin K2. Recent scientific examination has pinpointed vitamin K2, and in particular vitamin K2 as menaquinone-7 (MK-7), as the active ingredient in this popular eastern Japanese dish, as having a supportive effect on bone quality during osteoporosis treatment.5
People living in the Japanese regions where this dish is eaten have several-fold greater blood levels of vitamin K2 (MK-7), accompanied by less osteoporosis and bone fractures.6
These findings are supported by clinical trials, in which vitamin K2 has been shown to successfully reduce the incidence of bone fractures. A two-year Japanese study found that vitamin K2 (MK-4) reduced the incidence of vertebral (spine) fractures by 52% in 120 patients with osteoporosis, compared with patients who did not receive this nutrient.7 The high dose used in this trial—as with most studies examining vitamin K2's effect on bone density—was 45 mg/day, a prescription dose used in Japan to treat osteoporosis that is unavailable in the US. As you will read later, lower doses of K2 found in dietary supplements appear to also provide significant benefits.
CASE HISTORY: HEART DISEASE LINKED WITH OSTEOPOROSIS
Fit and trim at age 67, Walter had no reason to believe that he had any hidden health conditions.
He'd had annual physicals for the past seven years, passing them all. According to his doctor, his cholesterol numbers had been fine for years. But Walter's brother-in-law, a physician whose own brush with heart disease prompted him to warn everyone else in the family about the possibility, suggested that he undergo a computed tomography heart scan. Walter's heart scan score was 3,367, a high score that signaled a dangerous content of calcified atherosclerotic plaque in his coronary arteries linked to a high risk for heart attack. In fact, Walter's score put him in the 99th percentile, meaning that his calcium score was in the worst 1% of all men in his age group (and carried an annual risk for heart attack of 25% without preventive efforts).
At about the same time, Walter enrolled for a screening service that came to his church offering ultrasound screening for abdominal aneurysm, carotid disease, and osteoporosis. While Walter proved to have no aneurysm or carotid issues, he did show the bone density of someone 20 years older, revealing an advanced state of osteoporosis.
While seemingly unrelated, Walter's arterial calcification and osteoporosis were likely connected through the common mechanism of inadequate levels of vitamin K.
Vitamin K2 has also proven to be as effective as prescription drugs in reducing the incidence of bone fractures. In one Japanese study in post-menopausal women that compared the effect of K2 (MK-4) with the drug etidronate (Didronel®) on the incidence of vertebral (spine) fracture, women taking K2 at a dose of 45 mg per day experienced a fracture rate of 8.0% compared with 8.7% for those taking the drug therapy. Furthermore, women taking both MK-4 and the drug experienced a 3.8% fracture rate—a dramatic combined effect. In comparison, in a placebo group who received neither K2 nor drug therapy, nearly 21% of women experienced bone fractures.8
Experimental animal models of osteoporosis have also revealed that MK-4 improves bone architecture, increases bone mass and mechanical strength, stimulates mineralization (deposition of calcium), and enhances collagen architecture—a cross-linking of fibrous tissue that yields tough but supple bone that is more resistant to fracture.9
On the other hand, osteoporosis—the excessive loss of bone mineral density—results in fractures and leads to devastating events common in those over 65 years, even with minor injuries like a fall. Unfortunately, the drug industry focuses on prescribing drugs late in life when the risk for fracture is high. Strategies that involve nutritional supplements are different. Firstly, they lack the high cost and side effects of prescription drugs. Secondly, they can potentially be started at an earlier age and taken over 20, 30, or more years in order to yield possibly greater benefit than drug therapy started at the age of 60 to bail out a process that has developed over decades. Although there are no clinical trials for such an extended period, this is an area worthy of future investigation.
WHAT YOU NEED TO KNOW: VITAMIN K2
- While calcium is essential for good health, aberrant calcium metabolism can lead to disorders such as osteoporosis and cardiovascular disease. Vitamin K2 is emerging as a key factor in regulating calcium in the body.
- Insufficient vitamin K2 leads to decreased bone mineral density, a key factor in osteoporosis, and an excess of calcium in the arterial wall, which increases the risk of heart disease.
- In Japan, vitamin K2 has been shown to substantially improve osteoporosis when given either as a high-dose prescription agent or in the staple Japanese dish called natto, which is particularly rich in K2.
- Studies have also shown that even modest amounts of vitamin K2 fight heart disease by controlling calcium-regulating proteins in vascular tissue, which keeps calcium out of the arteries and prevents the formation of dangerous calcified plaques.
- Vitamin K2 occurs in much smaller quantities in the diet than vitamin K1. Most of us, therefore, get little of these K2-rich foods.
- Current dietary guidelines for vitamin K focus on how much is needed to regulate blood clotting and have largely ignored the much higher amount needed to maintain healthy bones and arteries.
Vitamin K2 Protects Against Coronary Heart Disease
Normal deposition of calcium occurs in two organs: bone and teeth. Abnormal deposition of calcium in the body occurs in three places: the inner lining of the arteries (the intima) where atherosclerotic plaque accrues; the muscle layer of arteries ("medial calcification"); and heart valves. Vitamin K2 appears to be the form of vitamin K that contributes to controlling all of these phenomena.
However, calcium has historically been viewed as a passive marker, certainly not an active participant in heart disease. Some maintained that calcium was nothing more than a remnant of prior "rupture," a scar from dangerous inflammatory activity of soft plaque. They even argued that calcium was, in fact, a reflection of increased plaque stability, as the "hard" material was not itself prone to rupture. Thus, they believed that calcium played no active role in contributing to atherosclerotic plaque.

Those arguments have now been dashed by new observations. A definitive connection between vitamin K2 levels and heart disease, in terms of a large-scale, well-controlled clinical trial, was first described in 2004 in the Rotterdam Heart Study—a Dutch trial that tracked 4,800 participants for seven years.1The study revealed that participants who ingested the greatest quantities of vitamin K2 in their diet experienced a 57% reduction in death from heart disease than people who ingested the least. The same relationship did not hold for vitamin K1. Unfortunately, in this study MK-4 and MK-7 intake and levels were not separately analyzed but were grouped together, along with other MK categories such as MK-8 and MK-9.
Higher intakes of vitamin K2 also corresponded to less calcium deposition in the aorta (an indirect measure of atherosclerosis), whereas participants who ingested less K2 were more likely to show moderate or severe calcification. The lowest risk of heart attack and aortic calcification was seen in participants who included more than 32.7 mcg a day of vitamin K2 in their diet.1
The size and quality of the Rotterdam Heart Study gave credibility to the powerful association between vitamin K2 dietary intake and heart disease and suggests that vitamin K2 may confer cardiovascular benefits by inhibiting arterial calcification.
Physicians and scientists are now intensely interested in monitoring and halting the accumulation of coronary calcium, since they know that it comprises a significant portion of atherosclerotic plaque volume.
It appears therefore that the accumulation of calcium signals actively growing atherosclerotic plaque and that vitamin K deficiency may set the stage for this pathogenic process.
VITAMIN K2 ENCOMPASSES A GROUP OF IMPORTANT SUBSTANCES KNOWN AS MENAQUINONES
The menaquinones make up about 10% of vitamin K consumption and can also be synthesized in the gut by healthy microflora. There are several different forms of menaquinone. Menaquinones are short-listed using the notation MK-n, where the 'n' specifies the number of prenyl side chains. MK-4 is available in high doses by prescription. MK-8 and MK-9 are found in fermented food products like cheese. Soy natto is a rich source of the highly bioavailable form of K2 known as MK-7.
MK-4, also known as menatetrenone, is distinct from other menaquinones because it is not a major constituent of MK-n produced by gut microflora.
Does Vitamin K2 Prevent Cancer?
Exciting preliminary evidence is emerging that vitamin K2 may suppress cancer.
In a serendipitous study, initially conducted to explore whether vitamin K2 provided protection against bone loss, investigators noticed that this nutrient dramatically reduced the risk of liver cancer.
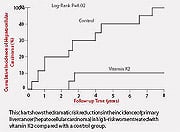
In this small Japanese study of 40 women who had liver cirrhosis from viral infections, there was a marked difference in the incidence of liver cancer, with only 2 of 21 developing cancer in the MK-4 group compared with 9 of 19 in a control group.15 The chart on this page shows the significant protective effect against primary liver cancer conferred by vitamin K2 in this study.
Similarly, a pilot study in 61 people recovering from surgical removal of hepatocellular carcinoma (liver cancer) showed that 45 mg/day of MK-4 (the dose used in Japan to treat osteoporosis) enhanced cancer-free survival by a wide margin.16
In the laboratory, vitamin K2 demonstrates inhibitory effects against myeloma and lymphoma, suggesting possible applications for individuals fighting these hematologic cancers.17
Perhaps this is just the tip of the iceberg with vitamin K2's fascinating effects on cancer. As most of the observations are just getting underway and some have arisen by chance observations, this is an area worth watching. Perhaps even more exciting for our purposes is discovering whether vitamin K2 prevents cancer if taken over a long period.
Obtaining Optimal Amounts of Vitamin K2
Vitamin K1 occurs naturally in green leafy vegetables, whereas vitamin K2 is found in relatively few foods. Organ meats, egg yolks, and the Japanese condiment natto, are sources of vitamin K2, of which natto is by far the richest source. Unfortunately, natto is an acquired taste and a dish that the average American may be unwilling to try. Vitamin K2 is also found in modest quantities in traditionally fermented
cheeses, in particular, Swiss Emmental and Norwegian Jarlsberg.18 Of total vitamin K dietary intake, only about 10% is the K2 form.
Vitamin K deficiency can also result from impaired absorption, in addition to not getting enough in the diet. It can also be caused by prolonged use of anti-biotics, since bacteria that normally reside in the colon (and are obliterated by antibiotic use) are responsible for producing approximately half of the vitamin K needed every day.
Unfortunately, the present recommended dietary intake of vitamin K, 90 mcg/day for women and 120 mcg/day for men, may be inadequate to maintain optimal heart and bone health.4,9,19
Although vitamin K1 is rapidly cleared from the blood, K2 lingers in the blood for an extended period when taken orally and can rise to much greater levels than seen with K1. Vitamin K2 appears to be safe, with no side effects identified even at high doses. In Japan, K2 substantially improves bone density and prevents osteoporotic fractures, given either as a high-dose prescription agent (45 mg/day) or in the Japanese dish natto.7,20 Together, these findings suggest that vitamin K2 may be the preferred form of vitamin K for supplemental use.
What dose of vitamin K2 is best? Scientists are still debating this question. Supplements generally contain between 50 mcg and 1,000 mcg of vitamin K2. Even the low end of the supplement dose of 50 mcg a day may help to support healthy bone density and protect the arterial wall from calcification. Life Extension has long recommended about 1,000 mcg a day of vitamin K2, along with 9,000 mcg vitamin K1 for most people.
CALCIUM-REGULATING PROTEINS
The possible role of vitamin K2 in preventing coronary plaque development has emerged from observations of its effects on several bone proteins, whose main function is to keep calcium where it belongs in the body.
Osteocalcin is a calcium-regulating protein that is controlled by vitamin K2. When vitamin K is present, osteocalcin normally undergoes a process called carboxylation, which binds osteocalcin to the mineral portion of bone. However, in vitamin K2 deficiency, osteocalcin cannot perform this function, resulting in unrestrained calcium resorption (removal) from bone tissue that leads to osteoporosis.
The opposite situation seems to occur in the arteries. Calcium is deposited because another protein called matrix GLA-protein, which is a calcification inhibitor and is also K2-controlled, cannot undergo the process of carboxylation in a vitamin K-deficient state. Because only carboxylated matrix GLA-protein inhibits calcification, undercarboxylated matrix GLA-protein has been found to occur in unusually high concentration at the edge of calcified and atherosclerotic plaques, suggesting it plays an active role in depositing calcium in plaque.4 Impairment of the function of osteocalcin and matrix GLA-protein due to incomplete carboxylation results in an increased risk for developing osteoporosis and vascular calcification, respectively.
Further evidence for the connection between vitamin K2 and arterial calcium comes from other research:
People with more advanced atherosclerotic plaque have reduced levels of carboxylated matrix GLA-protein, a vitamin K-dependent protein.10
- In animal studies, mice genetically bred to lack a protein that uses vitamin K2 develop unrestrained calcium deposition in the arteries (aorta and coronary) so powerful that they die within a few weeks of birth.11
- A similar mutation in the human gene that controls vitamin K production doubles the likelihood of atherosclerotic diseases like coronary disease, stroke, and aortic disease.12
- Furthermore, pregnant women taking the potent blood-thinning agent and vitamin K blocker, warfarin (Coumadin®), give birth to babies with severe abnormalities of bone structure.13
- Likewise, people who take Coumadin® suffer more osteoporotic fractures.14 They also show substantially more abnormal calcium deposition in other areas, such as heart valves—twice as much as non-Coumadin® takers.13
Safety Caution
If you take Coumadin® (warfarin), use of vitamin K should be discussed with your doctor before you begin supplementation, as changes in blood thinning (prothrombin time or INR [international normalized ratio]—measures of how quickly blood clots) will occur. Note, however, there are data to suggest that modest supplementation of vitamin K1 and perhaps K2 adds to long-term stability of blood coagulation.21 Further discussion can be found in the report, Vitamin K and Warfarin: Stabilizing Anticoagulant Therapy—While Protecting Cardiovascular and Bone Health, in the June 2007 edition of Life Extension Magazine.
Conclusion
The vitamin K2 experience requires further exploration to establish the scope of this exciting and underappreciated nutrient. Given the compelling science behind vitamin K2, enormously powerful benefits of supplementation may soon be realized for both good bone and arterial health.
If you have any questions on the scientific content of this article, please call a Life Extension Wellness Specialist at 1-800-226-2370.
Dr. William Davis is an author and cardiologist practicing in Milwaukee, Wisconsin. He is author of the book, Track Your Plaque: The only heart disease prevention program that shows you how to use the new heart scans to detect, track, and control coronary plaque.
He can be contacted through www.trackyourplaque.com.
References 1. Geleijnse JM, Vermeer C, Grobbee DE, et al. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study. J Nutr. 2004 Nov;134(11):3100-5.
2. Bostrom K, Watson KE, Horn S, et al. Bone morphogenetic protein expression in human atherosclerotic lesions. J Clin Invest. 1993 Apr;91(4):1800-9.
3. Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004 Jul;24(7):1161-70.
4. Schurgers LJ, Dissel PE, Spronk HM, et al. Role of vitamin K and vitamin K-dependent proteins in vascular calcification. Z Kardiol. 2001;90 Suppl 3:57-63.
5. Iwamoto J, Takeda T, Sato Y. Menatetrenone (vitamin K2) and bone quality in the treatment of postmenopausal osteoporosis. Nutr Rev. 2006 Dec;64(12):509-17.
6. Kaneki M, Hodges SJ, Hosoi T, et al. Japanese fermented soybean food as the major determinant of the large geographic difference in circulating levels of vitamin K2: possible implications for hip-fracture risk. Nutrition. 2001 Apr;17(4):315-21.
7. Shiraki M, Shiraki Y, Aoki C, Miura M. Vitamin K2 (menatetrenone) effectively prevents fractures and sustains lumbar bone mineral density in osteoporosis. J Bone Miner Res. 2000 Mar;15(3):515-21.
8. Iwamoto J, Takeda T, Ichimura S. Combined treatment with vitamin K2 and bisphosphonate in postmenopausal women with osteoporosis. Yonsei Med J. 2003 Oct 30;44(5):751-6.
9. Iwamoto J, Takeda T, Sato Y. Effects of vitamin K2 on osteoporosis. Curr Pharm Des. 2004;10(21):2557-76.
10. Schurgers LJ, Teunissen KJ, Knapen MH, et al. Novel conformation-specific antibodies against matrix gamma-carboxyglutamic acid (Gla) protein: undercarboxylated matrix Gla protein as marker for vascular calcification. Arterioscler Thromb Vasc Biol. 2005 Aug;25(8):1629-33.
11. Luo G, Ducy P, McKee MD, et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature. 1997 Mar 6;386(6620):78-81.
12. Wang Y, Zhang W, Zhang Y, et al. VKORC1 haplotypes are associated with arterial vascular diseases (stroke, coronary heart disease, and aortic dissection). Circulation. 2006 Mar 28;113(12):1615-21.
13. Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF. Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2. Arch Intern Med. 2006 Jan 23;166(2):241-6.
14. Schurgers LJ, Aebert H, Vermeer C, Bultmann B, Janzen J. Oral anticoagulant treatment: friend or foe in cardiovascular disease? Blood. 2004 Nov 15;104(10):3231-2.
15. Habu D, Shiomi S, Tamori A, et al. Role of vitamin K2 in the development of hepatocellular carcinoma in women with viral cirrhosis of the liver. JAMA. 2004 Jul 21;292(3):358-61.
16. Mizuta T, Ozaki I, Eguchi Y, et al. The effect of menatetrenone, a vitamin K2 analog, on disease recurrence and survival in patients with hepatocellular carcinoma after curative treatment: a pilot study. Cancer. 2006 Feb 15;106(4):867-72.
17. Tsujioka T, Miura Y, Otsuki T, et al. The mechanisms of vitamin K2-induced apoptosis of myeloma cells. Haematologica. 2006 May;91(5):613-9.
18. Hojo K, Watanabe R, Mori T, Taketomo N. Quantitative measurement of tetrahydromenaquinone-9 in cheese fermented by propionibacteria. J Dairy Sci. 2007 Sep;90(9):4078-83.
19. Shoji S. Vitamin K and vascular calcification. Clin Calcium. 2002 Aug;12(8):1123-8.
20. Katsuyama H, Ideguchi S, Fukunaga M, et al. Promotion of bone formation by fermented soybean (natto) intake in premenopausal women. J Nutr Sci Vitaminol (Tokyo). 2004 Apr;50(2):114-20.
21. Sconce E, Avery P, Wynne H, Kamali F. Vitamin K supplementation can improve stability of anticoagulation for patients with unexplained variability in response to warfarin. Blood. 2007 Mar 15;109(6):2419-23.
0 -
Thank you for the above posts! I have some mild calcification of my ascending aorta root as shown on echocardiogram. While K2 can help prevent calcification of vessels, is there anything that can aid in reversing calcification of soft tissues once it has occurred?
0 -
You know, weirdly enough, there is almost no research on this topic, almost like the goal of reversing Coronary Artery Disease, the no # 1 killer of women, is not worth their time. Here is a research abstract about reversing arterial calcifications in rats with a high Vitamin K2 diet. People on Warfarin, the anticoagulant, are known to become Vitamin K2 deficient.
Regression of warfarin-induced medial elastocalcinosis by high intake of vitamin K in rats.
Schurgers LJ1, Spronk HM, Soute BA, Schiffers PM, DeMey JG, Vermeer C.
Author information
Abstract
Arterial calcification (AC) is generally regarded as an independent risk factor for cardiovascular morbidity and mortality. Matrix Gla protein (MGP) is a potent inhibitor of AC, and its activity depends on vitamin K (VK). In rats, inactivation of MGP by treatment with the vitamin K antagonist warfarin leads to rapid calcification of the arteries. Here, we investigated whether preformed AC can be regressed by a VK-rich diet. Rats received a calcification-inducing diet containing both VK and warfarin (W&K). During a second 6-week period, animals were randomly assigned to receive either W&K (3.0 mg/g and 1.5 mg/g, subsequently), a diet containing a normal (5 microg/g) or high (100 microg/g) amount of VK (either K1 or K2). Increased aortic calcium concentration was observed in the group that continued to receive W&K and also in the group changed to the normal dose of VK and AC progressed. Both the VK-rich diets decreased the arterial calcium content by some 50%. In addition, arterial distensibility was restored by the VK-rich diet. Using MGP antibodies, local VK deficiency was demonstrated at sites of calcification. This is the first study in rats demonstrating that AC and the resulting decreased arterial distensibility are reversible by high-VK intake.
I will look around and see if there is any other research.
Happy Holidays to you all!
0 -
macb, Thanks so much for providing this information.
If VK2 were a pharmaceutical, you know there would be plenty of studies on it!
Do be aware that if you are on warfarin or coumadin, that your dose should be smaller than others. (Reference "Vitamin K2 and the Calcium Paradox")
0 -
Thanks for the timely reminder zogo about only having Vitamin K2 through the diet for those on Warfarin.
Happy Holidays to all of you marvelous women!
0