Will 30% of Early Stage (1-IIIA) go on to metastasize??
Comments
-
mountain...there is a huge difference and it isn’t contradictory. I see your point that there are many risks involved in reconstruction. The anesthesia alone comes with risks. However, when it comes to chemo, physicians and researchers spend years developing data that become guidelines. With those guidelines, a single oncologist can confidently make a recommendation to the patient. Now if something happens to a patient and the doctor didn’t follow the guidelines...well you know what can happen to the doctor.....those guidelines protect both the doctor and the patient. Again, I wonder what happened to the sister with the Oncotype Dx 8 score. I wonder if after MSK refused to give her the chemo if she found a willing doctor...
0 -
MikaMika, I take Oncotype results with a grain of salt. Well, a pound of salt, actually. Do a search on this site with my name and "Oncotype". I was responding to specific comments in several posts. Because an Oncotype score had been referenced, I used an Oncotype score as an example. Nothing more.
My very simple post on one very specific point has been taken to imply all sorts of things that I was in no way saying, implying, nor believe. Counter arguments have been made against points I never made, and I in fact agree with the counter arguments. It's become exhausting in this thread to constantly have to explain what I was not saying. So I've deleted my post. I'd decided a couple of days ago that I would be wise to stop posting in this thread. I should have stuck to my guns on that one.
0 -
Beesie,
I am grateful for all your posts, knowledge and help! And my point is that everyone is taking their risks with extra treatment or without. Since treatment is not ideal, everyone can decide which risk is preferable.
Thanks
0 -
MinusTwo, I get what you're saying. Having a lifetime of problems is a very good reason, IMO, to have BMX. I think there are many women who do come to this board who haven't experienced that, yet end up opting for the whole go-round of surgeries.
My point is not that it is a bad idea for them to do so (although I think it is, for some reasons, for many of them.) My point is that we have conflicting opinions about what the costs and benefits of various treatments are, and what makes it "worth it" for some and not for others. It is interesting and confusing, and something that would be easier to discuss out loud, rather than in this limited format.
0 -
Everybody is different and depends on what s/he feels comfortable with surgeries vs/or treatments after the diagnose. The doctor would suggest one thing and in the end, the patient will decide. In my case, I was recommended lumpectomy with radiation and it was my decision to go for BMX. I worked hard to convince my BS and DH for my decision and I have no regret. The difference between people like me and those who will preserve their breasts is how much do we trust treatments. Can radiation, chemo, AI kill all cancer cells? I am not a strong believer in the success of treatments vs surgery. I feel more comfortable removing all the breast tissue. But this is me. I haven't met anyone who went for radical surgery and has a regret. We make certain decisions to prevent future anxieties and worries. Right now I am in letrozole. Am I in the 30-40% group where letrozole is working or am I in the 70% where letrozole is not working? At least I know that I don't need to have mammograms+ anxiety every 6 months. As I said, everyone is different.
I also want to add a note to Beesie, you are followed by most of us and we respect your suggestions and we love to read your posts.
 0
0 -
Beesie, Beesie, Beesie! Don't tire yourself out on this thread....there will always be another thread that will command your attention! And it will also demand that readers follow your attention!
 0
0 -
Beesie - if you're still reading here, I concur that for my money, you are hands down one of the most - if not THE most - knowledgeable persons on BCO. I always appreciate reading your posts. And I always learn something. It is fantastic the amount of time you spend trying to calm people who are frightened and give new members a way to move forward.
I know discussions might get off track, but I hate that you felt it necessary to delete a post. Thank you for ALL your contributions.
1 -
MountainMia, I totally see what you're saying.
The fact that evidence says mastectomy doesn't prevent metastatic recurrence seems to always get lost in the mx vs. lumpectomy+rads discussions; why should we trust the surgery any more than the systemic treatments to keep us alive? The evidence tells us we shouldn't. But we tell women to go with their gut on this..but on chemo decisions we're more likely to support what the MO/treatment guidelines recommend. (by 'we' I mean generic consensus on the msg board...)
(I understand the *other* reasons a pt might choose a mx ... but when comparing to chemo decisions the underlying purpose of the treatment is the same: to preserve life so on that basis the recommendations should be similarly weighted).
It's an interesting distinction.
0 -
I hesitate to wade into the mastectomy vs lumpectomy w/ radiation debate, but here it goes.
I wish people would understand that *IF* we die from breast cancer (and many do not), it is usually because of metastatic disease. (Although there are some who die of treatment complications not related to metastatic disease, or other causes altogether.)
Mastectomies do not stop metastatic recurrences of the invasive breast cancers we already got. That's what systemic treatment does.
People may choose a mastectomy, and that's okay. But I am concerned that some people seem to choose a mastectomy out of a false sense of security rather than a realistic understanding of the actual risk reduction a mastectomy provides *after* already developing an invasive breast cancer.
MountainMia asks a valid question. There is no single answer, obviously.
0 -
Thanks to all of you for your thoughtful comments. Again, I posed the questions in a "devil's advocate" manner, and it's been very interesting to read through responses. I don't think I have a more solid opinion on a "right" answer! But it's a pretty complicated question, and each person's own circumstances mean there will never be a single answer, even for the individual.
0 -
let’s be clear...mountain first proposed the difference between someone wanting BMX FOR DCIS vs. the decision to have chemo for a low Oncotype DX score....then....the question morphed into BMX for an invasive cancer vs. lumpectomy and rads...
I think we need to step back and not lump all of them together and say they all are the same when it comes to PERSONAL decisions. A BMX for DCIS, yes, a personal decision. A BMX for an invasive cancer in one breast, yes, a personal decision. Reconstruction following mastectomy, yes, a personal decision. A lumpectomy with radiation if medically possible, a personal decision. Chemo for a high Oncotype DX score, or a lower score with a younger age, STILL a personal decision. Chemo for a LOW Oncotype DX score, NO, NOT a personal decision. Most physicians will not make that an option.
getting back to O/P, I think in the coming decade we should see the “numbers” improve as a result of better recordkeeping more than anything else. Think about this, here in the US we have switched over to mostly electronic recordkeeping. We record everything. So, moving forward we could potentially follow people over longer periods of time. In other developing countries, where recordkeeping lags, the “numbers” might be artificially skewed. Hopefully, going forward, fewer patients around the world will be lost to follow up and we can follow up a lot more patients.
likewise, have you ever noticed when some landmark study presents its data, it will say in small print how much longer the lead investigators are going to try to continue following the patients. Back in the day that was almost impossible to do. Electronic recordkeeping is now making that possible. Even now, it is still sometimes hard to do. But investigators and researchers are getting better at it. And, they are doing so much retrospective analysis that is becoming better and better at filling in gaps, finding new patterns and finding new leads to study.
so, in a few years from now, we may be able to better determine how many early stagers progress to metastatic bc. Until then, let’s stay well, stay safe and enjoy living0 -
The recent discussions highlight one of the things I am finding the hardest to wrap my head around, as someone who is just high-risk. At first I could not grasp how mastectomy didn't clearly improve outcomes for women with, say, stage I cancer. On the surface, this made NO SENSE to me. Now I have a better understanding that, by the time one gets a stage 1 diagnosis, in many cases, cells may have circulated and intrinsic aspects of the tumour govern how effective systemic therapy will ultimately be.
In some way it feels like mastectomy actually makes the most sense for someone at very high risk but who (hopefully) does not have invasive cancer yet (e.g. DCIS). This is how I interpret the standard of care re: BRCA 1/2 carriers. It's obviously incredibly hard to figure out who else is in the same boat, in the absence of such a clear genetic risk factor. But a lot of advice feels like it goes from "it's too early / overkill to do something drastic" then ... if anything is found, "it's too late, there's no point, we can't prove a survival advantage". (Of course, this also points out what a blunt tool mastectomy is as a treatment.)
1 -
These are not easy decisions, and I think that either surgical option can be a good decision depending on the circumstances. My overall point is really more that I hope patients (especially new patients in the shock and awe phase) will make an informed choice based on reality, rather than on fears that are not particularly based in reality.
It's true that in may cases the tumor has already seeded itself distantly by the time it is detected by a mammogram and we make a surgery decision. The doctors know this, but as patients it is hard to wrap our heads around this in the beginning.
Current tests are not sensitive enough to know whether we have tumor cells lodged somewhere distantly, and we have to make a systemic treatment decision based on that best guess. In most cases, if the cancer never comes back, either systemic treatment worked for you, or your tumor never successfully seeded itself distantly anyway.
sasamat, you raise an interesting point too. If I had known I would get breast cancer at 32, I would have wanted a mastectomy at 20. If I had known at 32 that I would have a metastatic recurrence at 36, I would not have bothered with a mastectomy. But that's life - we do the best we can with the information we have at the time, I suppose!
0 -
Interesting discussions. Back to original post, bottom line, I think people should hear the data on risk recurrence for early stage cancers, understanding it may be 5 years old already and that it is changing. In my case, the data that 20 - 30% of people with early stage BC will go on to metastasize was never, ever said to me when I was dxed with DCIS, no lymph node,BC ER+ PR+ HER2- , in 2007 at age 54. (Showed up from in tiny calcifications. We know that significant % of women who die of other causes in their 80s have calcifications, and it was 1 radiologist who said we must biopsy this one, the one w a star shaped pattern in which biopsy found the DCIS.) I understood from the charts that following lumpectomy + radiation that my chance of being cancer free 5 years out was nearly 99 % . I had no risk factors, no family history, except that I weighed 40 lbs more than I did at 25, but which no one mentioned at the time as a risk factor. Five years later, I self-identified a lump at a different spot in the same breast, this one negative for ER, PR, but HER2+, Stage 2A, no lymph node involvement, with underlying DCIS in tumor tissue. Treated then with chemo, TCH, mastectomy. No hormone prophylaxis, as the cancer was hormone negative. Risk of being disease free 5 years out was now more like 85%, according to the data.
And yet, here I am, it's 2021, my bones all over my body filled with MBC dxed in 2018, again found to be ER+PR+, HER2-. My doc says it is possible the estrogen fueled cancer was already hiding in blood, marrow, years ago so that local steps didn't stop it, that we don't know what turns on those cancer cells to activate wherever they are hiding, and why some women go on to metastasize and most women don't. Should I have had chemo in 2007 for DCIS? No one would recommend that!!! And I had chemo in 2012, but that didnt stop those suckers from appearing 5/6 years later.
To me, the 30% risk of recurrence/metastases is important information for every woman to know, and it seems hidden from people w early stage cancers, because docs talk in 5 year, 10 year increments of PFS, where the numbers who go on to recurrence are small. But at the same time it wouldn't have changed my treatment decisions at the time. I wasn't put on tamoxifen after 1st bout of dcis because of hx of blood clots, so onc thought risk 50/50, cancer recurrence v blood clot. Said we might try an AI later after we see how they are doing, as one was newly on the market. Then we forgot about it in the face of good mammos, busy life. Would it have just petrified me and made me insist on more full body screening beyond the mammograms in my remaining breast had I known risk of recurrence was so high? I do wonder why MRIs and PETs aren't done periodically on someone with 2 bouts of BC, e.g. every 3 years, or even why doc stopped checking my CA27-29 after 3 years out from last cancer, which marker had never been elevated during bout 2 in any case. Might have seen metastases 1 - 2 years earlier? But I learned/was told regular PET/MRI in someone disease free for years doesn't change OS so not standard of care for someone with treated early stage BC. But really, might metastases have been found while still limited in number, and then treated aggressively? Maybe. The only known risk factors for recurrence after my 2012 bout were the fact of the 2 cancers, and the nature of the 2nd tumor, which was grade 3. Oh, also I'm overweight and I drink wine.
So much is unknown about BC and what we do know is changing all the time. We as individuals cannot prevent it beyond taking simple steps of weight control, exercise, healthy diet, no smoking, very limited or no alcohol, and regular medical care with latest data to guide it. Fundamentally, I feel we are dealing with the fact that recurrence is not in our hands, it is still in the control of the disease. It is just bad luck to be a part of the 30 %. And that is infuriating, especially for those of us who see ourselves as being in charge of our lives.
0 -
Beesie, I love your posts and look for them. I wish I had 1/2 your brain power...even a 1/4 of it would lift me up, LOL.
regarding the mastectomy vs lump/rads, my BMX decision was based on more than just risk of local recurrence. My choice was also based on amounts of screenings (dyes that are cummulative, relocation to area that may not have breast MRI), the nervous-nellie w/ health-cancer and horrific scanxiety I would have and though I could still have a local recurrence, my odds are much lower. Also, the radiation is not without danger and I've known enough women (in my real life) who went on to develop cancers from the rads that ultimately took their life, not the original breast cancer. It is rare, but if I could avoid it, that was my goal.
0 -
I am late to this discussion, but would like to add my story to this. I was told that I was cured after 5 years. There was never any discussion of recurrence from either my GP nor my MO. In fact my MO told me "I am dumping your chart because you're too healthy" even though I had complained about pain in my arm & back.
It would be another year before I was sent to the surgeon because of another problem & as an aside he asked if I was having any pain anywhere. I told him about my arm, back & by that time pain in my sacrum that he ordered a bone scan, the next day all hell broke loose with 3 Dr's calling me with the results.
At no point was I told that breast cancer could come back in my bones. I kick myself for not reading more about recurrence but I figured my Dr's would tell me anything I needed to know.
0 -
none of my doctors have wanted to discuss chance of recurrence or what my long-term outlook is. They only want to focus on the 5-year survival number, which is a very happy 95% in my case. After it turned out that I did have a positive node, discovered after surgery, my doctor didn’t want to go Into how that might change my staging and thus my long term statistical outcomes - he only wanted to focus on how successful the chemo was.
In some ways I get it - statistics are good for big studies and not really useful for individual outcomes. At the same time though, it’s a real disservice to patients to not even discuss the possibilities. It was through this site and threads like this one that I learned I would always have an increased chance of breast cancer returning and that there was really no way to know if I was “cured.”
0 -
Oy, I should know better but I'm wading in again.
If we are talking about what doctors should telling breast cancer patients about their future risk, there are actually three separate categories of risk that should be discussed, and while one or maybe two might be, all three rarely are.
1) Metastatic cancer risk, which is what this thread has been focused on.
2) Local recurrence risk, i.e, a recurrence in the breast (after a lumpectomy) or breast area (yes, local recurrences can happen even after a MX, something patients aren't always told).
3) The risk of a new primary breast cancer. Too many people seem to think that after a breast cancer diagnosis, we are immune from getting another. The opposite is true. After a diagnosis of either DCIS or invasive cancer, our risk to develop a new primary breast cancer, either in the same breast or the contralateral breast, is significantly higher than the risk level faced by someone not previously diagnosed. This second diagnosis is completely unrelated to the first, and the cancer itself could be quite different - sometimes less aggressive/advanced but sometimes more aggressive/advanced. Timing could be anything from a couple of years after the first diagnosis to 20+ years later. Breast cancer risk increases as we age and for all women is highest in our 60s and 70s; for those previously diagnosed, our risk during these years is even higher. Women are usually shocked when they get a second diagnosis so many years after their first diagnosis, but they shouldn't be.
MountainMia, while I understand and agree with many of your thoughts about a BMX for those who have a small low risk DCIS, the risk of a second primary, particularly for someone yet to enter their highest risk years, is one to add into the column favouring a BMX - a new primary can develop after a BMX but the risk is extremely low compared to the risk for those who retain one or both breasts. I've been on this site long enough that I know of several people who had DCIS and then years later developed a second primary which was invasive and aggressive and which eventually developed into mets. (And before anyone says "but what about", let me say that I think there are many items in both columns, for BMX and against BMX - which is why a BMX for any small early stage cancer is as much a personal decision as a medical one.)
Moominmamma, your second diagnosis would have been either #2 or #3. Since the cancer was in a different part of your breast, and was HER2+ vs. your DCIS being HER2-, I wonder if it's #3. That would mean that your DCIS was in fact successfully treated, but you had the crappy luck to develop a second more aggressive cancer. Did your doctors ever discuss whether they thought your second diagnosis was a new primary rather than a recurrence?
Thanks to all for the very kind comments. Some days I hit overload.0 -
Dear Beesie
Thank you for a very helpful clarification. Yes, my docs did discuss whether #2 was a recurrence or new primary, and leaned toward new primary. They did tell me radiation didn't work, so wouldn't be repeated and I wondered if it might have played any role in #2 dx. The spot was where in 2007 they had removed a spot of ADH, but no sign of anything else at the time.
Important information about SEER beginning(!) to collect recurrence data finally, see https://www.medscape.com/viewarticle/943796.
GG27- your story is so familiar. My docs really thought I was a success, and "cured" once I was out 2 or 3 years from treatment. When I started complaining of underarm pain on both sides off and on over the course of the next couple years, one did an ultrasound side once and found nothing, and at my last mammo in early 2018 the BC doc decided on feel that the lumpiness under my left arm where I also had scar tissue from BC #2 surgery was necrotic scar tissue and sent me to PT to improve range of motion and comfort. No ultrasound ordered at the time. 4 months later it was SOB & chest pain concerning for PE that sent me to ER where on chest CT they incidentally found extensive bony metastases in ribs and left underarm axillary stranding. Of course it was diffuse cancer in axilla as biopsy revealed. My primary doc says it likely wouldn't have mattered to discover cancer 4 months earlier, but really all the weird new symptoms I was having beginning in 2018 - like sudden onset of urinary frequency and even incontinence, pain in back, chest, legs at night - were all signs of metastases which no one looked for. Each symptom was treated separately and not as possibly related.
Anyway, it is good to hear more focus on recurrences in BC is starting to happen!
0 -
Hi all
Just to add my bit to this thread
We should be told that we are never cured remission would be a better word
We should never be discharged from our onc
It's just too easy to forget ( me included) because life goes on and we cannot worry all the time
I don't know about percentages but if it's you it's 100%
Now I enroll in stage4 Could it have been prev. who knows?
Best to all
0 -
Reading. Awesome talk. Beesie, I think your last post above should be printed and mailed to every breast surgeon, doctor, oncologist and radiation oncologist in Canada and the U.S.
Annadou, I think the word 'cured' should be stricken from breast cancer talks by doctors. It's the word we all want to hear. It's the promise we all want to believe. It's the goal we pay for with surgery, chemo, radiation, vomiting, neuropathy, our hair, our sexuality (damn you tamoxifen!). We throw A LOT of ourselves into the fire to hopefully appease the Cancer god, that he may pass us over and not take us before we are very, very old and ready to go. We want so badly for someone to bring us good news. To ease that sickening feeling in the pit of our stomach as we sit in a waiting room to hear the news. When people ask me how I am, meaning how is my health, I have one answer and it's always the same answer and it is as close to the truth as I can get. I say, "I'm fine. For now."
We dance on the razor's edge, don't we?
1 -
runor, thanks.
The one thing that I would add to my previous post - and maybe it ties to my frustration with the subject line of this thread - is that for most Stage I patients who have not had a BMX, and maybe for some Stage II patients too, the risk of a new primary breast cancer is actually higher than their risk of mets. How many people know that?
Obviously the risk of mets is a much more serious concern and a more immediate concern when we are first diagnosed and for the next 5-10 years. At some point though the risk of mets starts to decline; how long that takes depends on whether the diagnosis was triple negative, HER2+, or ER+/HER2-. And of course the risk of mets never fully disappears. But I think we all reach a point where we start to breathe a bit easier, thinking that most of our risk is behind us. Yet for those diagnosed in their 40s and 50s (or younger), the risk of a new primary has continued to increase as they've been getting older. So 15 years out from diagnosis, the risk of mets might only be 2% but the risk of a new primary might be 20%.
I hate seeing posts from people who develop mets and didn't realize that they could - those told by their doctors that they were "cured" or those who think that because they had a BMX they can't develop mets, or those who think that because they were node negative they can't develop mets.... There are lots of reasons for this misunderstanding and these are things that no patient should misunderstand (recognizing, to the earlier discussion, that some patients just don't want to know and tune out what they are being told).
But I also hate seeing posts from people who develop a new primary and don't understand how that could happen. Posts that say "I'm 17 years out and I really thought I had beaten this thing, but now it's back in the other breast." I've written dozens of posts that try to gently explain that they probably have successfully beaten the original diagnosis, but unfortunately they've developed a new breast cancer, and in fact they've been higher risk all along because of having been diagnosed previously. And this too is something that no patient should not know and yet is something that very few patients seem to know.
Unfortunately there is no lack of lack of understanding.
0 -
Yes, Beesie. I'm at the break-point. Diagnosed 2 years ago at age 58, stage 1 tnbc, lumpectomy, chemo, rads. My risk of new primary is still in the range of 10-15%, likely, and my risk of mets is approx the same.
That's my personal status. I hate it, and also I'm glad I understand it. I'd hate to be blindsided with either.
0 -
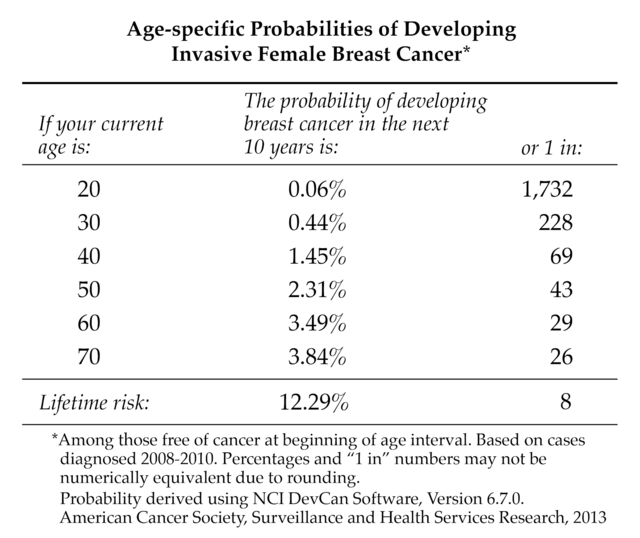
MountainMia, not to scare you, but based on my reading, I would guess that your risk of a second primary might be higher than you estimate. The average 58 year old has about a 9% to 10% remaining lifetime risk of breast cancer. Breast cancer patients appear to have between a 60% to 100% increase in breast cancer risk (100% increase equating to double the risk) vs. the general population, and it appears that those with a TN first primary breast cancer have a higher risk than that.
Second Primary Breast Cancer Occurrence According to Hormone Receptor Status https://www.ncbi.nlm.nih.gov/pmc/articles/PMC27209...
.
Estrogen receptor, progesterone receptor, and HER2-neu expression in first primary breast cancers and risk of second primary contralateral breast cancer https://www.ncbi.nlm.nih.gov/pmc/articles/PMC41444...
.
Hormone receptor status of a first primary breast cancer predicts contralateral breast cancer risk in the WECARE study population https://breast-cancer-research.biomedcentral.com/a...
0 -
Beesie, you raise many excellent points. Just as an added clarification, or in depth discussion about this particular point, when you said the following about "most" patients...
"The one thing that I would add to my previous post - and maybe it ties to my frustration with the subject line of this thread - is that for most Stage I patients who have not had a BMX, and maybe for some Stage II patients too, the risk of a new primary breast cancer is actually higher than their risk of mets. How many people know that?"
...would this mainly apply to those with low and intermediate Oncotype scores? As a person with a high Oncotype score, I think my metastatic recurrence risk was always higher than my risk of a new primary, even as a young person. That was always just the reality that I lived with, although I think you are correct in pointing out that for many/most the risk of a new primary is higher. Interesting.
0 -
Beesie--all I can say is WOW. Just WOW! This is information that is worthy of its own thread with a well worded title. Women on this site need to understand this information!
I am one who experienced the reality of a second breast tumor: a Phyllodes Tumor in 1996 and IDC in 2018. The Phyllodes never threatened my life (just lost half a breast), but I never knew that I was at such heightened risk until I was having the biopsy in 2018. While I was on the table with the radiologist taking samples, she told me my dense breast tissue put me at a 4-6 times greater risk of developing breast cancer and the Phyllodes Tumor only increased the risk of having developed a new cancer. I wish I'd met her at a party a few years before rather than learning this while having a biopsy for what turned out to be cancer. I would not have been putting so much faith in 3D mammograms and would have insisted on ultrasounds along with my mammograms, at the very least--along with MRI's at reasonable intervals.
This is truly the kind of information women who participate in this site need to know.
0 -
I'm not scared, but thanks for the clarification and links. I knew the stats aren't great, so a few more percentage points don't change that. Well, I should say, I'm not more scared than I already was. Basically, I figure there's a relatively high chance of another diagnosis. If I get out of this life without that happening, I'll be kind of surprised.
0 -
buttonsmachine, that's a good question, and I think the answer is , "it depends".
While higher Oncotype scores confer a higher risk, this risk is of course reduced by treatment. Based on this chart, it appears that post-chemo/hormone therapy metastatic risk (the solid blue line) comes in at about 14% for an Oncotype 48 score (I'm using a "48" since it's the highest score on this chart.)
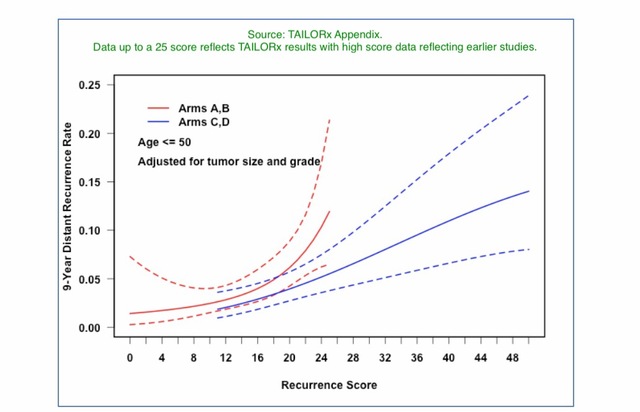
Then we have to consider that Oncotype scores reflect a 9 year risk, but metastatic risk for ER+/HER2- patients runs out for 20 years. Based on this chart I posted previously, at 9 years there remains outstanding a bit more than 20% of the metastatic total risk. This means that someone with a 48 Oncotype score would have a lifetime metastatic risk of around 18% (14% being 78% of 18%).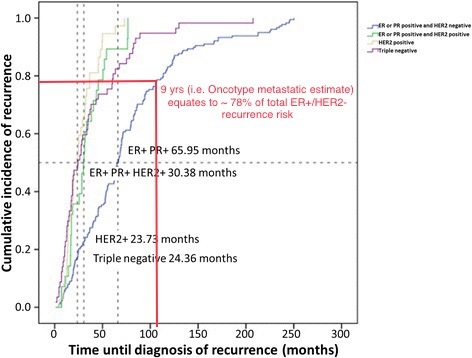
Next complication, patient age and pathology. I post on BCO often about the Oncotype RSPC model (Recurrence Score Pathology Clinical) that takes the patient's Oncotype score and the average recurrence risk associated with that score, and adjusts the risk based on patient age, tumor size and tumor grade. This means that a very young patient with a 48 score will have a risk that is higher than the average Oncotype risk of 14%. A grade 3 tumor and a larger tumor would increase risk further. So this could turn an average lifetime risk of 18%, based on an Oncotype 48 score, into... I don't know. 25? 30? (Note that this is a discussion of "Stage I" and "high Oncotype score"; age doesn't factor into staging but tumor size does, and for the newer Pathological Prognostic Staging, tumor grade does as well. So while someone young with a high Oncotype score might be Stage I, we're unlikely to see many people in Stage I who have large, grade 3 tumors.)
As for new primary risk, what my MO told me was that my risk was double that of the average woman of the same age who'd never been diagnosed before. One of the studies I linked in my post to MountainMia also found that for those who've had ER+/HER2- cancers, risk is double. If we take the average 40 year old, her remaining lifetime risk (she no longer has to worry about the risk she faced in her 20s and 30s) is 11.8%. Double that, and you get a 23.6% lifetime new primary breast cancer risk for someone aged 40 who was previously diagnosed with an ER+/HER2- breast cancer.
Lots of playing with numbers and reliance on individual studies, so this calculation has to be taken as an estimate only. But it's probably in the ballpark. And what it says is that even for someone with a 48 Oncotype score, if she follows treatment protocol, then depending on her age and the pathology of her cancer, her risk of a new primary might be higher than her risk of mets. But for some, those younger who had an aggressive pathology, the risk of mets might be higher than the risk of a new primary.
So, it depends.
0 -
My god. Do you ever get the feeling this ought to be some gruesome game show where you, the bewildered and slightly addled cancer patient, gets called up onto the stage and a massive wheel gets whirled around titled "All The Things That Can Kill You, Cancer Edition" ? Some of the notches on the wheel are immediate bad news and others are bad news that you get the fun of waiting for, like a surprise package of dog poop being delivered to your house at some unknown point in the future. Wait for it, be ready for it, brace for it, it's dog poop.
I confess that at some point considering all this became Too Much. Trying to figure out how big a state of spazzing out I should be in became exhausting. I had no reason to have cancer. I had a 'thing' that I was assured multiple times by different people along the way did NOT really look like a typical cancer, so it probably wasn't. It looked like a radial scar and most of those aren't cancer. But sorry, sucks to be me, it was cancer, it was a radial scar, it was on the large side at 2.5 cms and when radial scars are found to be cancer it doubles (if I understand my reading correctly) your chances of having another cancer. I carried all this information in my head and in my heart for a long, long time. I got rid of possessions. I updated my will. I wrote a medical directive and power of attorney. I got my life in order. I woke up every day thinking about cancer. I looked at my husband and kid and thought about leaving them forever. It broke me.It was then and is now of crucial importance for me to have a solid, reality based handle on the situation. I was caught off guard once by cancer. Never again. It may very well show up in the other boob which frankly is the best possible place for it to show up. Better there than anywhere else, that's for damn sure. So if I skip off into the sunset thinking I am cured I am setting myself up for a very ugly shock in the future. I hope it never comes back. But what I hope just as much is that I never go through those feelings of terror and utterly stupifying anxiety and despair that paralyzed and crippled me. I try now to cultivate an attitude and philosophy about the reality I face. It is hard, I fail mostly, but knowing is of absolute value. It is a burden I choose to carry.
I think the compelling nature of the title of this thread may jar some of those Not Want to Knows, into I Better Pay Attentions. It is eye catching in that it pings anxiety. They can come here in a panic and leave here in an informed panic. I think that's better.
0 -
I am one of the lurkers that never posts, but I want to agree with rumor about the title of this thread. I know (because i have read it from the beginning) that some don’t like it but personally I think it’s good if it catches people’s attention - the “Not Want to Know’s” as rumor puts it. There are far too many people, including MOs, who seem to feel that the less you know, the less you will worry. Probably true. But I don’t think that burying your head in the sand (whether it has to do with cancer, your financial situation, or anything else) solves anything and in a lot of cases, just ends up making things worse. If the title scares a lot of stage 1 (or 2 or 3) women into reading this thread, it will be to their benefit. They will be far better educated and have a very realistic understanding of where they stand (thanks to Beesie and others who provide a wealth of information that is invaluable). And they will understand that the odds for them may not be 30%, or 20%, maybe not even 10%, but at least they will know that their odds are not zero, never were, never are going to be and that they should remain vigilant and keep their head firmly unburied!
0